Use of the Ilizarov technique to correct complex knee deformities associated with end-stage tuberculosis of the knee joint.
Dr. Syed Nihal, Post-Graduate Resident, Department of Orthopedics, Sree Balaji Medical College and Hospital, No 7 CLC Works road, Chrompet - 600044, Chennai, Tamil Nadu, India. E-mail: sydnihal95@gmail.com
Introduction: After the spine, the knee is the second most common location for skeletal tuberculosis. An unusual complication of tuberculosis infection is triple knee deformity. The combination of knee flexion, posterolateral tibial subluxation, and external tibial rotation over femoral condyles manifests as a severe deformity. Currently, a variety of surgical intervention techniques are recommended for knee deformity correction, including the use of an Ilizarov ring fixator or limb reconstruction system, total knee arthroplasty, and arthrodesis with synovectomy.
Case Report: A 17-year-old adolescent with a 2-year limping history and left knee flexion deformity and swelling was examined. The patient was treated with anti-tuberculosis therapy for 9 months after being diagnosed as having pulmonary tuberculosis. The results of the left knee synovial fluid aspiration revealed confirmation of tuberculosis knee. The Ilizarov technique was used to treat the patient’s 95° fixed flexion deformity of the knee which was associated with painful jog of movements.
Conclusion: The Ilizarov procedure has been regarded as the best way to treat complicated deformities of the knee caused by tuberculosis sequelae because it has great clinical results and few side effects.
Keywords: Complex knee deformity, tuberculosis, Ilizarov fixator.
After pulmonary tuberculosis, skeletal system tuberculosis has the second highest morbidity rate, and knee joint tuberculosis is the second most prevalent site of involvement after the spine (1). Treatments for early synovial or bone tuberculosis of the knee include anti-tubercular drugs, joint lavage, and thorough debridement. To reduce swelling, and pain, and achieve normal gait, end-stage tuberculosis typically presents with severe articular surface deterioration, joint abnormalities, and severe dysfunction, necessitating deformity correction followed by arthrodesis using the Ilizarov technique(2,3). Due to the challenge of diagnosing early and the lack of economic and transportation means in a few places, individuals with tuberculosis knee are frequently referred for treatment later in the disease’s progression or when it has deteriorated fatally. Deformity correction followed by arthrodesis employing the tension-stress concept of the Ilizarov technique has been universally acknowledged as the best treatment option for this condition because of its low cost, lack of the need for further surgery, and effective curative results (4,5).
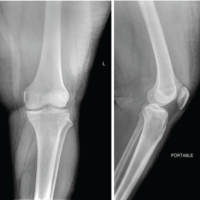
A male patient, age 17, complained of left knee fixed flexion deformity that had worsened over the past 2 years and prevented him from using his affected leg for walking. The patient allegedly had a history of pain in his left leg and limping 4 years prior, for which he was treated conservatively. Subsequently, he had an alleged history of slips and falls at home, for which he underwent native splints (8 splints over 80 days). After three to four splint changes, the patient started to notice a deformity over his left knee because of manipulation and massage that was done during each splint change. The patient lost weight and presented with constitutional symptoms; as a result, he was diagnosed with pulmonary tuberculosis and started on anti-tubercular medications. Left knee synovial fluid aspiration showed increased Adenosine deaminase, total counts, glucose, and protein levels along with a POSITIVE acid-fast stain, following which he was diagnosed with tuberculosis of the knee joint. The patient noticed a worsening of flexion deformity during his anti-tuberculosis therapy course. The patient underwent lower tibial pin traction at an outside hospital, but after complaining of paresthesia in his left foot, the pin traction was discontinued. Upon examination, the patient had a left knee flexion deformity associated with a painful jog of movements, a fused patella, and a full range of motion in the left hip without involvement of the opposite limb. Muscle atrophy in the patient’s thighs and calves was evident (Fig. 1a and b).
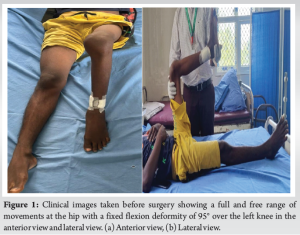
Preoperative planning was completed along with routine blood investigations. Knee X-ray Anteroposterior and lateral views and a CT scanogram showed a knee flexion deformity of 95° (Fig. 2b). A left knee Magnetic resonance imaging revealed articular surface damage, extensive subchondral erosions, and diffuse synovial thickening.

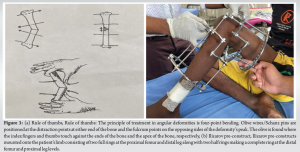
A diagnosis of fibrous ankylosis of the left knee was made with fixed flexion deformity because of post-tuberculosis sequelae and the patient was planned for a two-stage procedure: Common peroneal nerve release and deformity correction using the Ilizarov technique in the first stage, followed by left knee arthrodesis as a second-stage procedure. On the CT scanogram, femoral and tibial mechanical and anatomical angles, and the patient’s flexion contracture were all measured and were found to have a direct flexion contracture of 95°. Before the surgery, the Ilizarov frame was pre-built after checking the patient’s thigh and calf diameters using the four-point bending rule for angular deformity correction to shorten the surgical time (Fig. 3a). The pre-built Ilizarov frame was mounted onto the patient’s leg and checked (Fig. 3b).
Surgical technique
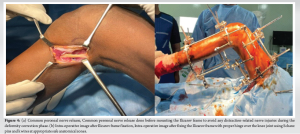
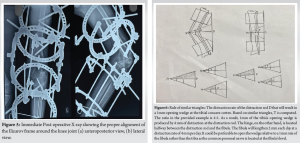
Stage I: Ilizarov correction of the left knee deformity and release of the common peroneal nerve. The patient was in a supine position under spinal and epidural anesthesia, an oblique 6 cm incision was made below the head of the fibula, and common peroneal nerve release was carried out (Fig. 4a). The patient’s left leg was fitted with the pre-built Ilizarov frame, which consisted of two full rings at the proximal aspect of the thigh and distal leg levels, and at the levels of the proximal leg and distal thigh, two half rings combined to form a full ring with accurate hinge placement and an appropriate distractor using C-ARM guidance (Fig. 4b). A post-operative X-ray was done to check the Ilizarov frame alignment around the knee joint (Fig. 5a and b). Following post-operative rehabilitation guidelines, the post-operative time was uneventful.
Post-operative management and assessment
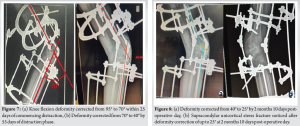
After surgery, the patient was put on daily analgesics and prophylactic antibiotics. The pin site was regularly dressed in a local antiseptic for pin care. We advised the patient to start using crutches to walk on the 2nd day after surgery. Utilizing both clinical and radiographic exams, we evaluated the patient. White blood cell counts, erythrocyte sedimentation rate, and C-reactive protein were routinely analyzed using blood samples. The pace of distraction was calculated using the rule of similar triangles (Fig. 6), and it began 1 week after surgery. Depending on the patient’s cooperation or the emergence of any distraction-related issues, the pace of distraction was altered. Distraction began at a pace of 2 mm/day and continued for 2 months and 10 days and the deformity was corrected from 95° to 26°. After achieving a knee flexion deformity correction of up to 26°, we discovered a uni-cortical supracondylar stress fracture. Distraction was halted and serial radiographs were done until the fracture site showed signs of good union with 3 weeks of rest and immobilization. Distraction was restarted again and continued for 3 weeks. Every month, radiographic imaging with lateral and anteroposterior views of the knee joint was carried out to measure the deformity correction angle until deformity correction of up to 10° was achieved (Fig. 7-9). The tibial condyle and femur were perfectly aligned and locked at 10° of knee flexion for 4 weeks during the consolidation phase post-deformity correction.

The Ilizarov external fixator was removed at 4 months 20 days post-operatively (Fig. 10a-c) with the most recent radiograph showing good bone quality. After removing the fixator, we put the patient in an above-knee plaster of Paris slab in extension with a 10° knee flexion for 1 month and advised strict non-weight-bearing walking with walker support. The patient was then placed in a tube cast and was advised to begin full weight-bearing walking for 1 month. The patient was then advised to have long knee braces and full weight bearing for 3 months with brace support after which, the patient was able to walk without brace support and carry on his day-to-day activities without any discomfort. The patient was followed up for 1 year post-operatively during which clinical and radiological evaluations of the patient were done every 3 months. The Lysholm score was used to assess the knee’s functionality, discomfort, and the patient’s self-reported observations before and after surgery. Excellent was defined as a score of 95–100, good as 84–94, fair as 65–83, and poor as < 65.
Some surgical methods to treat fixed flexion knee deformity include hamstring lengthening, posterior capsulotomy, epiphysiodesis of the distal femoral growth plate, femoral or tibial osteotomy, femoral shortening, or arthrodesis. Although osteotomies are successful, they change the structure of the joint, in contrast to soft tissue releases, which don’t seem to be very effective in repairing the deformity. Massive soft tissue release could cause instability in the joints. Because it is inexpensive, has few difficulties, and produces positive results, gradual extension with external fixators has been universally accepted as the best course of treatment (6,7). The following are some benefits of this procedure: (1) No internal fixation or other external fixation can pressurize 360°, fix accurately, and allow for rapid weight bearing after deformity correction like Ilizarov rings can; (2) In the early post-operative stage, the fusion angle and pressure might be modified if they are not optimum; (3) Installation is far from the affected area, which limits the spread of tuberculosis; (4) For individuals with sinus cavities, skin defects, thin skin tissue, or numerous bone defects, the external fixation method is preferable to internal fixation; (5) When compared to internal fixations, its intraoperative radiography fluoroscopy frequency and duration are comparatively less; and (6) Due to the steel rings on the device utilized for this patient, the material cost was less than that of internal fixations. The fixator’s hefty weight, the discomfort of dressing, and the increased risk of pin tract infection are some of the drawbacks of this procedure (8). Lysholm’s score for the patient at the past follow-up (86), which dramatically improved from that before surgery (36) showed that his first-stage Ilizarov technique deformity correction procedure enhanced the patient’s knee function and lifestyle quality. The patient was content with the deformity correction that had been achieved, providing him with a stable and pain-free joint, and he wanted to schedule his second-stage treatment, arthrodesis of the knee joint, for a later time (9). After a month of being in a leg cylinder cast, the patient was given an above-knee brace to encourage complete weight bearing. An ongoing point of contention has been the angle at which knee joint deformities should be corrected. Most specialists recommend correcting the knee joint up to full extension to prevent additional limb shortening. Patients rotate the lower limb outward and abduct the hip joint to make up for the knee stiffness when the pelvis is elevated excessively at 0° flexion of the knee, which increases the amount of energy used when walking. At a knee flexion angle of roughly 15°, the shortening will increase by about 2 cm. In addition, a flexion of 5°–10° can more effectively resolve the paradox between energy expenditure and limb shortening. After the deformity was corrected, we were able to create a satisfactory gait, and our patient was happy with the results of the treatment (10). The patient received advice regarding the possibility of developing early-onset joint arthritis and joint instability, which may necessitate knee arthrodesis as a second-stage procedure down the road (11).
The patient’s knee functionality drastically improved post-knee deformity correction using the Ilizarov technique, and we were able to achieve a good functional outcome with a minimum complication rate.
When treating end-stage tuberculosis, the Ilizarov method is seen to be the best alternative for arthrodesis and reversing knee joint abnormalities. It has a lot of advantages, including low cost, instantaneous capacity to bear weight, high fusion rate, and only a few issues.
Ilizarov technique is widely considered one of the best methods of treatment for deformity corrections due to its ability for accurate deformity correction in all planes and its ability to instantaneously weight bear post-surgery and minimal complication rate.
References
- 1.Hoffman EB, Allin J, Campbell JA, Leisegang FM. Tuberculosis of the knee. Clin Orthop Relat Res 2002;398:100-6. [Google Scholar | PubMed]
- 2.Soeroso N, Ananda F, Rahmadhany H, Putra D. Tuberculosis of the knee: A pitfalls in clinical settings (A case report and literature review). Int J Surg Case Rep 2020;71:14-8. [Google Scholar | PubMed]
- 3.Shah P, Lohiya D. A rare case of post tuberculosis sequelae of left knee with triple deformity. PAMJ Clin Med 2022;9:16. [Google Scholar | PubMed]
- 4.Gaurav K, Vilas J. A new approach to the management of fixed flexion deformity of the knee using Ilizarov’s principle of distraction histogenesis: A preliminary communication. Int J Low Extrem Wounds 2010;9:70-3. [Google Scholar | PubMed]
- 5.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res 1989;238:249-81. [Google Scholar | PubMed]
- 6.Salama W, Abdelaal A, EL-Azab H, Hafez A, Masse A, Marzouk A. Correction of lower-limb deformities using Ilizarov device. Egypt J Orthop Res 2020;1:11-6. [Google Scholar | PubMed]
- 7.Cravener E. Device for overcoming non-bony flexion contractures of the knee. J Bone Joint Surg Am 1930;12:437-9. [Google Scholar | PubMed]
- 8.Bor N, Rubin G, Rozen N. Ilizarov method for gradual deformity correction. Oper Tech Orthop 2011;21:104-12. [Google Scholar | PubMed]
- 9.Sun J, Li Q, Gao F, Xiang Z, Huang Q, Li L. Application of the Ilizarov technique for knee joint arthrodesis as a treatment for end-stage tuberculosis of the knee. BMC Musculoskelet Disord 2020;21:579. [Google Scholar | PubMed]
- 10.Spiegelberg B, Parratt T, Dheerendra SK, Khan WS, Jennings R, Marsh DR. Ilizarov principles of deformity correction. Ann R Coll Surg Engl 2010;92:101-5. [Google Scholar | PubMed]
- 11.MacDonald JH, Agarwal S, Lorei MP, Johanson NA, Freiberg AA. Knee arthrodesis. J Am Acad Orthop Surg 2006;14:154-63. [Google Scholar | PubMed]