The ideal treatment is based on anatomical reduction, stable fixation, and surgery as early as possible to prevent complication such as avascular necrosis and post-traumatic arthritis.
Dr. Amit Manohar Awachat, Assistant Professor, RGMC and Chhatrapati Shivaji Maharaj Hospita, Kalwa, Thane, Maharashtra, India. E-mail: awachatamit1141@gmail.com
Introduction: Pediatric hip fractures comprised <1% of all pediatric fractures. These fractures are usually associated with high-energy trauma, such as motor vehicle accidents or fall from height. The Delbet classification of pediatric hip fractures is frequently used to describe these injuries and to relate the fracture type to the development of avascular necrosis. Treatment should be given as an emergency basisand monitoredaccording to the type of fracture and the patient’s age. Historically, casting was used for such fractures; however, due to the high complication rate, the treatment modality has shifted to early anatomical fixation.
Case Report: We presentthe case report withdetailed history, examination, and treatment of a 12-year-old boy with an uncommon site of fracture at right transepiphyseal hip fracture with dislocation. Emergency initial operation was done and followed up for 2-year duration on regular basis. The patient has currently normal gait with painful terminally restricted movements.
Conclusion: Early recognition and operative management of pediatric hip fractures has improved outcomes.
Keywords: Fracture neck of femur, femoral epiphysial fracture, pediatric hip fracture, Ganz safe dislocation of hip, Delbet classification, hip spica application
Pediatric hip fractures are very rare and are usually caused by high-energy trauma, often combined with multiple injuries [1-4]. These fractures are frequently associated with additional extremity, visceral, and head injuries in approximately 30% of cases. Proximal femur fractures in children occur at a rate of 1.2–2 cases per year, accounting for approximately 0.3–0.5% of all fractures in children [1-4]. The peak incidence is between the ages of 10 and 13 years (with a range from 1 day to 18 years), and the male-to-female ratio is approximately 1.3–1.7:1 [5,6]. In pediatric hip fractures, thereare of significant concern due to the high rate of complications and the potential for lifetime morbidity. Dysfunction and pain are the most frequently reported complications, affecting 20–50% of patients. These complications may result from osteonecrosis, coxa vara, proximal femoral physeal growth arrest, non-union, and growth abnormalities leading to limb length discrepancy or angular deformity [7].
Classification of proximal femur fracture in pediatrics
Pediatric hip fractures are generally classified by the method of Delbet (Fig. 1) [8].
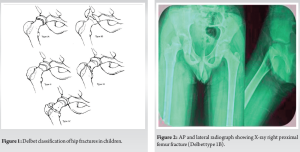
Type 1-transepiphyseal fracture
1A-without dislocation
1B-with dislocation
Type 2 – transcervical
Type 3 – cervicotrochantric
Type 4 – intertrochanteric
This fracture classification not only provides descriptive information but also has prognostic significance. In , osteonecrosis occurs in 16–47% of cases. Type 1 and Type 2 fractures are more prone to osteonecrosis and growth arrest, whereas the latter two groups tend to have higher rates of varus malunion. The outcome for Type 1B fractures is inferior, with osteonecrosis and premature physeal closure occurring in nearly 100% of patients. When a dislocation is not reduced within 6 h, the risk of AVN increases dramatically due to compromised blood flow to the affected area, especially in joints like the hip [9]. AVN can lead to the death of bone tissue, resulting in long-term issues such as stiffness, discomfort, and instability.
A 12-year-old male presented in emergency department after 3 days with a history of a motor vehicle accident, accompanied by pain in the right hip, inability to bear weight and wound over the right knee. The patient was initially taken to primary health care center where multiple close reduction attempts were given. Later patient brought in our hospital for further management. There was no history of any previous chronic medical illness. Advanced Trauma Life Support (ATLS) protocols were followed. The patient was conscious, alert, and oriented to time, place, and person. A head-to-toe examination revealed a lacerated contaminated wound with measuring 8 × 3 cm on the anterior aspect of the right knee. Local examination of the right hip showed swelling and tenderness over the joint line. The range of motion in the right hip was restricted and painful. Pelvic and bilateral hip X-rays confirmed a right proximal femur fracture with transepiphyseal dislocation (Delbet type 1B) (Fig. 2).
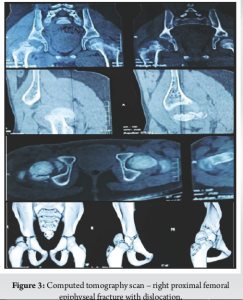
Emergency CT pelvis with bilateral hip was done (Fig. 3). After examining the X-rays and CT scan considering the fracture type and age, emergency surgical intervention was planned. Treatment options and complications were discussed with the family, written informed consent was taken.
The patient was taken to the operative room, under combined spinal epidural anesthesia with patient in left lateral position, under all aseptic precaution parts painted and draped. A lateral incision was made, centered over the anterior and middle thirds of the greater trochanter. The fascia lata was incised along the skin incision, and the gluteus maximus was split. The vastus lateralis was retracted anteriorly, and the interval between the piriformis and gluteus medius was developed. The capsule was identified deep to the gluteus medius. A greater trochanteric osteotomy was performed and the trochanteric flip piece along with its muscular attachments was reflected anteriorly. The hip capsule was then opened with Z-shaped incision (Fig. 4).
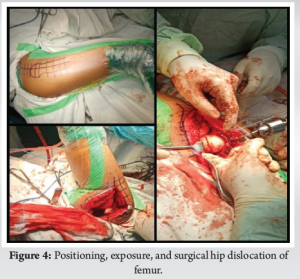
A safe surgical dislocation of the hip (Ganz dislocation) was achieved by flexing and externally rotating the hip followed by cutting the ligamentum teres with curved scissors. The fracture epiphysis was temporarily fixed with a K-wire and then secured with two Herbert screws. The hip was reduced (Fig. 5).
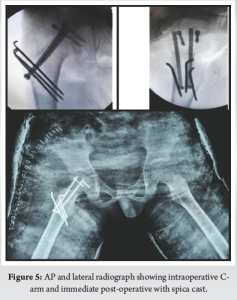
Trochanteric osteotomy is fixed with 2 partially threaded cannulated cancellous screw and 3 k-wires, c-arm shoots were taken, sterile wash given, capsule repaired, and incision closed in layers. Sterile dressing was given and post-operative stabilization was given with hip spica casting.
Post-operative management and follow-up
A post-operative X-ray was taken with the hip spica cast in place. The patient tolerated the procedure well and there were no complications such as deep vein thrombosis or wound dehiscence. The wound over the right knee was debrided and closed primarily. The patient’s parents were instructed on the specifics of spica cast care and the patient was scheduled to be discharged after 5 days. The patient was followed up at regular intervals to monitor for any early signs of avascular necrosis. He was closely monitored by the outpatient department and hip spica cast was removed at 2 months. K-wire and cc screw was removed at 3 months (Fig. 6). The patient showed positive initial improvement and followed a physical therapy plan that included mobilization using a wheelchair and gradual weight-bearing.
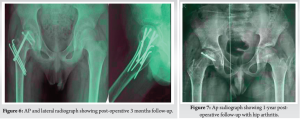
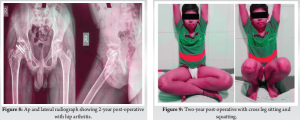
One year after the surgical fixation, the patient presented at the clinic with a normal gait, no active complaints and X-rays indicated complete healing with hip arthritis with signs of avascular necrosis (Fig. 7). After 2 year follow-up, the patient was doing cross leg sitting and squatting (Fig. 8 and 9).
Pediatric hip fractures are very rare and cause significant morbidity in adulthood if not fixed anatomically on acute basis. Accidental fractures are a frequent occurrence in childhood and pose considerable risks to children’s health. The likelihood of bone fractures increases as children grow older. However, the occurrence of multiple fractures in children is rare and usually associated with high-energy trauma. As first described by Delbet, pediatric hip fractures can be classified into four types [7], which help determine whether operative or non-operative treatment is appropriate and predict the risk of avascular necrosis (AVN) of the femoral head. The present case involved Delbets type 1b femur fracture. According to Delbet’s classification, Types I and III are associated with a 15 times higher risk of AVN compared to other fracture types [7]. Even with the timely intervention of reduction and fixation of the femoral head, there is a high rate of associated osteonecrosis (0–92%). Multiple injuries are consistently linked to high-energy trauma and this case included both a knee injury and a femur fracture. Due to the presence of incarcerated fracture fragments and soft-tissue interposition, closed reduction is difficult and potentially more damaging to the vascularity of the head. Non-surgical treatment with spica casting remains the initial method for all patients under the age of five [9]. However, children above this age threshold are increasingly undergoing surgical intervention. Surgical treatment has reduced the burden of care for families, shortened hospital stays, decreased early disability rates, and minimized disruption to families’ lives [10,11]. Optimal outcomes are achieved through the urgent reduction of the femoral head, the use of safe surgical techniques to preserve vascularity, stable fracture fixation, and appropriate rehabilitation. Ideally, closed reduction should be attempted in an operation theater; however, if closed reduction failed open reduction should be done. However, time between injury and reduction does not directly correlate with the risk of avascular necrosis. Urgent closed reduction following patient presentation is recommended for all patients.
This report demonstrates that early surgical treatment with internal fixation followed by cast immobilization can significantly improve functional outcomes. However, the risk of avascular necrosis and post-traumatic arthritis are common sequelae of these fractures and necessitate long-term follow-up to address these complications.
Outcomes of these fractures are best determined by urgent reduction of the femoral head, safe surgical techniques to preserve vascularity, stable fixation of fractures, and proper rehabilitation.
References
- 1.Rockwood CA Jr, Beaty JH, Kasser JR. Rockwood and Wilkins’: Fractures in Children. Philadelphia, PA: Lippincott Williams and Wilkins; 2010. [Google Scholar | PubMed]
- 2.Staheli LT. Fundamentals of Pediatric Orthopedics. Philadelphia, PA: Lippincott Williams and Wilkins; 2008. [Google Scholar | PubMed]
- 3.Kopjar B, Wickizer TM. Fractures among children: Incidence and impact on daily activities. Inj Prev 1998;4:194-7. [Google Scholar | PubMed]
- 4.Walsh SS, Jarvis SN, Towner EM, Aynsley-Green A. Annual incidence of unintentional injury among 54,000 children. Inj Prev 1996;2:16-20. [Google Scholar | PubMed]
- 5.Gallagher SS, Finison K, Guyer B, Goodenough S. The incidence of injuries among 87,000 Massachusetts children and adolescents: Results of the 1980-81 statewide childhood injury prevention program surveillance system. Am J Public Health 1984;74:1340-7. [Google Scholar | PubMed]
- 6.Rivara FP, Calonge N, Thompson RS. Population-based study of unintentional injury incidence and impact during childhood. Am J Public Health 1989;79:990-4. [Google Scholar | PubMed]
- 7.Lasanianos NG, Kankaris NK, Giannoudis PV. Trauma and Orthopaedic Classification: A Comprehensive Overview. London, UK: Springer-Verlag; 2015. [Google Scholar | PubMed]
- 8.Boardman MJ, Herman MJ, Buck B, Pizzutillo PD. Hip fractures in children. J Am Acad Orthop Surg 2009;17:162-73. [Google Scholar | PubMed]
- 9.Barquet A. Natural history of avascular necrosis following traumatic hip dislocation in childhood: A review of 145 cases. Acta Orthop Scand 1982;53:815-20. [Google Scholar | PubMed]
- 10.Moon ES, Mehlman CT. Risk factors for avascular necrosis after femoral neck fractures in children: 25 Cincinnati cases and meta-analysis of 360 cases. J Orthop Trauma 2006;20:323-9. [Google Scholar | PubMed]
- 11.Palocaren T. Femoral neck fractures in children: A review. Indian J Orthop 2018;52:501-6. [Google Scholar | PubMed]