PRP injection and physiotherapy both effectively improve pain and function in supraspinatus tendon tears, with PRP potentially offering faster initial relief. However, long-term benefits may be similar between the two treatments.
Dr. Adnan Anwer, Department of Orthopaedic Surgery, Jawaharlal Nehru Medical College, Faculty of Medicine, Aligarh Muslim University, Aligarh - 202002, Uttar Pradesh, India. E-mail: dr.adnan.amu@gmail.com
Introduction: Supraspinatus tendinopathy is a common reason for shoulder pain, with or without an associated cuff tear. Various modalities of treatment have been described in literature such as physiotherapy, analgesics, corticosteroid injection, surgical repair (open or arthroscopic), and platelet-rich plasma (PRP) injection. Recently, there has been an increasing trend of PRP injection for rotator cuff arthropathy. Hence, we conducted a study to assess the effectiveness of PRP injection under ultrasound (USG) guidance in patients with supraspinatus tear.
Materials and Methods: Twenty-eight patients were divided into two groups: Group A (physiotherapy, n = 15) and Group B (PRP injection with USG guidance, n = 13). Pain (Visual Analog Score [VAS]) and function (Oxford Shoulder Score [OSS]) were evaluated at baseline, 1 week, 4 weeks, and 12 weeks.
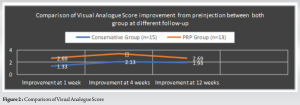
Results: 28 patients were divided into two groups, i.e., Group A (15 pt) - physiotherapy and Group B (13 pt) - PRP injection. On the basis of the VAS, PRP group has better score at 1 and 4 weeks as the results were statistically significant while insignificant at 12 weeks. On the basis of OSS, PRP group has better score at 1 and 4 weeks as the results were statistically significant while insignificant at 12 weeks similar to VAS score.
Discussion: The findings on pain relief (VAS) generally agree that both methods offer short-term improvement, with PRP potentially having a slight edge. However, the long-term effects (beyond 3 months) are less clear. Similarly, physiotherapy shows promise in improving function (Oxford score) in the short term, while some PRP studies suggest sustained benefits, possibly dependent on the specific PRP formulation. Overall, the discussion highlights the need for further investigation into the long-term efficacy of PRP compared to physiotherapy for managing rotator cuff tears.
Conclusion: Improvement in function and relief in pain were better in PRP group when compared to conservative group but we found that PRP has no superior result as compared to conservative therapy in the management of rotator cuff tear.
Keywords: Platelet-rich plasma, supraspinatus tendon tear, physiotherapy, Visual Analog Score, oxford shoulder score.
The supraspinatus is one of the muscles of the rotator cuff of the shoulder and it is responsible for abduction of the glenohumeral joint and assists in preventing subluxation at the shoulder. Supraspinatus tendinopathy is a common reason for shoulder pain, with or without an associated cuff tear. It is the most commonly injured tendon of the rotator cuff. A tear or rupture of the tendon of the supraspinatus muscle can occur in 3 ways: Partial, full thickness, or complete tear, and most of the time, it is accompanied by another rotator cuff muscle tear [1]. Rotator cuff tears have a reported greater incidence among the adult population and are associated with significant functional limitations commonly caused by supraspinatus muscle. Asymptomatic tears are more common than symptomatic tears. The most common risk factors for such cases are trauma, overuse, dislocations, elderly age, male gender, smoking, diabetes, high body mass index, repetitive overhead activities, and occupational such as tennis players, baseball pitchers, painters, and carpenters. The role of imaging is to guide treatment decisions. The diagnosis of rotator cuff injury, tendinopathy, partial or full thickness tear, and its extent can determine whether the patient will undergo surgery or just will be managed conservatively. Surgical treatment can be performed either as an open or arthroscopic procedure, but the repaired tissue is of poor quality and frequently degenerates, and these procedures are carried out under general anesthesia which carries its own risk [2]. Recently, there has been growing interest in the area of biological therapies to assist musculoskeletal repair. Autologous platelet-rich plasma (PRP) is one such therapy that has gained much attention. There are well-established studies demonstrating healing properties, decreased pain, and superior functional outcomes using PRP injections in cases of sport injuries [3]. PRP allows platelet-derived factors to be locally available to the tissue throughout the healing process in patients with rotator cuff disorders. Accordingly, our study aims to assess ultrasound (USG)-guided PRP injection’s role in partial and full-thickness supraspinatus tendon tears.
This clinical prospective randomized case–control study was conducted at a tertiary care hospital from October 2019 to October 2021 on 28 patients who were divided into two groups, i.e., Group A – who received supervised rehabilitation through conservative measures and Group B – patients who received PRP injection [Fig 1]. Patients presented with partial or full-thickness tears were included in the study while rotator cuff tears secondary to fracture and dislocations, patients with an associated dislocation at the time of study, rotator cuff tears that underwent prior surgical repair or revision arthroscopy, patients on anti-platelet drugs, and pre-existing conditions such as local malignancy, gross shoulder instability, pregnant, or plan to become pregnant in the next 12 months were excluded from the study.

Patients in both groups were assessed clinically (Jobe’s/empty can test, Hawkins-Kennedy test, Neer’s impingement test, and external rotation lag test), functionally (VAS and Oxford shoulder score [OSS]), and sonographically at baseline and after 3 months. The sonographic changes were assessed and recorded in the form of the appearance of the tendon, tendon thickness, measurement of tear, etc.
Statistical analysis
The categorical variables are presented in the form of numbers and percentages (%). On the other hand, the quantitative data are presented as means ± standard deviation and as median with 25th and 75th percentiles (interquartile range). The Shapiro–Wilk test is used to ascertain the distribution of data. VAS and OSS variables are normally distributed. Paired samples and independent samples t-tests are applied according to the data. A P < 0.05 is considered statistically significant. Data analysis is done using the Statistical Package for the Social Sciences, software, IBM manufacturer, Chicago, USA, ver 20.0.
Why PRP?
Despite satisfactory results by other treatment modalities, the incidence of persistent tendon defects or re-tears is still significant. 85% of surgical repair failures occur during the first 6 months of recovery, with 74% occurring in the first 3 months. Two years after arthroscopic rotator cuff repair, 70% of supraspinatus repairs and only 27% of supraspinatus with infraspinatus repairs remained intact [4]. Several studies have demonstrated that native tendon-bone insertions are not fully restored after rotator cuff repair. Consequently, repaired tendons have inferior mechanical properties and are more susceptible to re-tearing. Hence, advances are made toward promoting the biological healing of damaged tendons with the forerunner being the local injection of PRP. The growth factors (GF) and cytokines present in PRP include platelet-derived GF, transforming growth factor beta, fibroblast growth factor (FGF-2), insulin-like GF 1 and 2, vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), interleukin-8, keratinocyte growth factor, and VEGF [5]. Insulin-like GF stimulate osteoblast proliferation and differentiation GF, EGF and FGF-2 have been shown to stimulate the proliferation of osteoblastic progenitors. Also, they affect mitogenesis of mesenchymal stem cells and stimulate epidermal cell proliferation. Transforming growth factor beta stimulates collagen synthesis, angiogenic factors VEGF and FGF-2 have shown to enhance early angiogenesis and revascularization [6]. When the PRP is injected in musculoskeletal tissue, it forms a blood clot followed by degranulation of platelets which releases GF and cytokines that help in tissue repair.
PRP preparation
50–80 mL of blood was drawn from the patient under all aseptic precautions. This whole blood was subjected to centrifugation at 2000 rpm (soft spin). The whole blood was separated into three layers. The supernatant layer of plasma and buffy coat was separated and subjected to centrifugation at 3000 rpm (hard spin). In the final end product, the upper two-thirds of the tube contained platelet poor plasma which was removed, and the lower one-third was PRP enhanced with superficial buffy coat which was used for injection. PRP was extracted for injection.
Intervention procedure
Patients were positioned and the site of injection was decided. Then, the local anesthesia was given at the site of injection subcutaneously. Patients were administered PRP under USG guidance at the local site. On an average 5–7 mL of PRP was injected. The patients were advised to give rest to the part, use ice packs in case of pain, and avoid non-steroidal anti-inflammatory drugs (NSAIDS) as NSAIDS are known to decrease the quality of platelets injected. In case pain was unbearable, they were advised to take tablet paracetamol 500 mg as per need. Patients were advised to slowly advance activities of daily living progressively over 2 weeks and return to activity as tolerated.
Study included 28 patients, out of which 15 patients (53.57%) received physiotherapy and 13 patients (46.43%) underwent PRP injections. The age of the patients ranged from 31 years to 68 years with the mean age of patients in conservative group being 39.3 with ± 4.08 with median (25th–75th ) of 40 and patients in PRP group were 45.84 with ± 14.4 with median (25th–75th ) of 40. Male patients were more in our study with 53% in Group A and 61% in Group B. Right side was more common in both the groups. In Group A, 33.3% patients had full thickness tear while 66.7% had partial thickness tear while in Group B, 30.7% had full thickness tear and 69.7% had partial thickness tear. Visual Analog Score (VAS) at 1 week showed more improvement from baseline in PRP group as compared to conservative group with values being 2.69 ± 0.85 and 1.33 ± 0.61, respectively, with the difference being statistically significant in favor of PRP group. At 4 weeks also, PRP group showed more improvement as compared to conservative group with values being 3.46 ± 1.12 and 2.13 ± 0.91, respectively, with the difference being statistically significant in favor of PRP group. Further scores at 12 weeks showed more improvement in PRP group as compared to conservative group with values being 2.69 ± 1.75 and 1.93 ± 1.33, respectively, but the difference being statistically insignificant. The difference in VAS between two groups was only statistically significant at 1 and 4 weeks and insignificant at 12 weeks. Oxford score at 1 week showed more improvement from baseline in PRP group as compared to conservative group with values being 4.53 ± 0.77 and 1.00 ± 0.377, respectively, with the difference being statistically significant in favor of PRP group. At 4 weeks also, PRP group showed more improvement as compared to conservative group with values being 4.23 ± 1.69 and 2.26 ± 0.96, respectively, but the difference being statistically significant in favor of PRP group. Further scores at 12 weeks showed more improvement in PRP group as compared to conservative group with values being 3.3 ± 2.13 and 1.93 ± 1.22, respectively, but the difference being statistically significant. The difference in Oxford score between two groups was statistically significant at 1 week, 4 weeks, and 12 weeks. (Fig. 2)
Oxford score at 1 week showed more improvement from baseline in PRP group as compared to conservative group with values being 4.53 ± 0.77 and 1.00 ± 0.377, respectively, with the difference being statistically significant in favor of PRP group. At 4 weeks also, PRP group showed more improvement as compared to conservative group with values being 4.23 ± 1.69 and 2.26 ± 0.96, respectively, but the difference being statistically significant in favor of PRP group. Further scores at 12 weeks showed more improvement in PRP group as compared to conservative group with values being 3.3 ± 2.13 and 1.93 ± 1.22, respectively, but the difference being statistically significant. The difference in Oxford score between two groups was statistically significant at 1 week, 4 weeks, and 12 weeks. (Fig. 3)
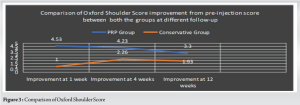
The mean pain score improvement in our study was of 1.93 points on a 10-point VAS at 12 weeks. A study done by Baumer et al. [7] showed that VAS score improved significantly (P < 0.05) from 3.8 before physiotherapy to 1.7 after a mean of 9.8 physiotherapy sessions. This is in contrast to our study where we saw slight deterioration in VAS by the end of 3 months. A study conducted by Munday et al. [8] where one group received manual therapy and another group received placebo and followed for 4 weeks using VAS. Pre-post difference within groups was significant (group 1, 2.7 [P < 0.05]; group 2, 1.9 [P < 0.05]) and difference between groups was 0.80 with P = 0.019, suggesting that conservative treatment has role in pain control. These data parallel the findings in our study and suggest that conservative therapy has short-term efficacy on pain control. On comparing both the groups, the difference in VAS score between 2 groups was statistically significant at 1 week and 4 weeks and insignificant at 12 weeks (P = 0.205). A study done by El Gharbawy et al. [9] showed statistically significant improvement in VAS before (7.1) and 4 weeks (3.7) after PRP injection. In a study done by Rha et al. [10], analyses revealed significant improvement in the VAS score at all assessment points compared with baseline (P < 0.05) in both PRP and placebo groups. This is consistent to our study where there is no statistically significant improvement between both the groups at 12 weeks of PRP injection. A randomized control study was done by Nejati et al. [11], to compare the efficacy of USG-guided PRP versus conservative therapy for treatment of subacromion impingement syndrome. In this study, patients were evaluated using VAS for pain at baseline, 1, 3, and 6-month follow-up. The VAS at baseline in Groups I (8.3 ± 1.1) and II (8.1 ± 1.2) significantly improved after injection (2.3 ± 1.4 and 2.3 ± 1.3; P = 0.0008 and P = 0.0009, respectively). Two-month post-injection, there was a significant improvement of pain in each group; however, there was no significant difference between two groups. The outcome of this study is similar to our outcome. Pre-injection OSS in conservative group was 32.67. At 1 week and 4 weeks, oxford score showed continuous improvement to scores of 33.67 and 34.93, respectively, with all the improvements in scores being statistically significant. At 12 weeks, slight decline was seen in improvement in scores but the decline was insignificant (P = 0.24). In a study done by Dickens et al. [12], patients were divided into physiotherapy and control group. All patients in physiotherapy group had improved constant scores over the 6-month period. The mean constant score at initial assessment was 52 as compared to 56 in control group and the mean improvement in the constant score was 20 as compared to 0.65 in control group. These data parallel the findings in our study and suggest that physiotherapy results in significant improvement in functional outcome during the initial period. Another study conducted by Wirth et al. [13], in which patients were assessed using the University of California-Los Angeles (UCLA) score at baseline and 2 years after conservative treatment, showed a significant improvement in UCLA score from 13.4 at baseline to 29.4 post 2 years of treatment. This is inconsistent with our study, where a slight decline was noted in the pain improvement at 12 weeks. Pre-injection OSS in PRP group was 33.85. At 1 week, OSS showed improvement to score of 38.38. At 4 weeks and 12 weeks, decline was seen in the improvement in score to 38.08 and 37.15, respectively, but the decline was insignificant (P > 0.05). The difference in OSS between two groups was statistically significant at 1 week, 4 weeks, and 12 weeks in favor of PRP group. A study done by Rossi et al. [14] showed continued statistically significant improvement in constant score from baseline (53.8) at 3 (86.1) and 12 months (87.2) after PRP injection. This is in contrary to our study where we saw decline in improvement after 1 week of PRP injection. This could be related to the use of leukocyte-rich PRP used in Rossi et al. study whereas no such formulation was used in our study. A randomized control study done by Ebert et al. [15], to evaluate the arthroscopic supraspinatus repair after repeated post-operative applications of PRP where 30 patients participated in PRP group and 30 patients were in control group. The study showed no significant difference between both the groups for VAS and OSS. This is in contrast to our study where there is a significant difference between both the groups for VAS and OSS.
Sample size was less and duration of follow-up was less due to the COVID-19 pandemic. Single-dose PRP was injected in our study; multiple doses might have shown better results. Furthermore, volume of injection, most effective preparation, and the most effective rehabilitation protocol after PRP injection should be determined by further studies.
We found that both conservative therapy and PRP injections resulted in significant improvement in Visual Analog Scale and Oxford shoulder scale over the course of 3 months. However, the improvement in function and relief in pain were better in PRP group when compared to conservative group. With conservative and PRP group, we found reappearance of mild pain by the end of 3 months as demonstrated by worsened VAS scores although still significantly better than pre-therapy pain with no statistically significant difference between both the groups at 12 weeks. Improvement in function as demonstrated by OSS was seen in both the groups. Difference in functional outcome of both the groups was insignificant after 3 months. Therefore, we conclude that PRP has no superior result as compared to conservative therapy in the management of rotator cuff tear.
This study suggests that while image-guided PRP injection may offer some short-term advantages in pain relief and function compared to physiotherapy for rotator cuff tears, these benefits appear to diminish over time. Considering the lack of long-term superiority and potential cost concerns, physiotherapy remains a reasonable first-line approach. However, PRP could be a potential option for select patients who show limited response to physiotherapy. Further research with larger studies and longer follow-up is needed to definitively compare these treatment strategies.
References
- 1.Simons DG, Travell JG, Simons LS. Myofascial Pain and Dysfunction: The Trigger Point Manual. Upper Half of Body. 2nd ed., Vol. 1. Philadelphia, PA: Williams and Wilkins; 1998. [Google Scholar | PubMed]
- 2.Millstein ES, Snyder SJ. Arthroscopic evaluation and management of rotator cuff tears. Orthop Clin North Am 2003;34:507-20. [Google Scholar | PubMed]
- 3.Ben-Nafa W, Munro W. The effect of corticosteroid versus platelet-rich plasma injection therapies for the management of lateral epicondylitis: A systematic review. SICOT J 2018;4:11. [Google Scholar | PubMed]
- 4.Jo CH, Kim JE, Yoon KS, Shin S. Platelet-rich plasma stimulates cell proliferation and enhances matrix gene expression and synthesis in tenocytes from human rotator cuff tendons with degenerative tears. Am J Sports Med 2012;40:1035-45. [Google Scholar | PubMed]
- 5.Hamid MS, Mohamed Ali MR, Yusof A, George J. Platelet-rich plasma (PRP): An adjuvant to hasten hamstring muscle recovery. A randomized controlled trial protocol (ISCRTN66528592). BMC Musculoskelet Disord 2012;13:138. . [Google Scholar | PubMed]
- 6.Filardo G, Kon E, Di Martino A, Di Matteo B, Merli ML, Cenacchi A, et al. Platelet-rich plasma vs hyaluronic acid to treat knee degenerative pathology: Study design and preliminary results of a randomized controlled trial. BMC Musculoskelet Disord 2012;13:229. [Google Scholar | PubMed]
- 7.Baumer TG, Chan D, Mende V, Dischler J, Zauel R, Van Holsbeeck M, et al. Effects of rotator cuff pathology and physical therapy on in vivo shoulder motion and clinical outcomes in patients with a symptomatic full-thickness rotator cuff tear. Orthop J Sports Med 2016;4: [Google Scholar | PubMed]
- 8.Munday SL, Jones A, Brantingham JW, Globe G, Jensen M, Price JL. A randomized, single-blinded, placebo controlled clinical trial to evaluate the efficacy of chiropractic shoulder girdle adjustment in the treatment of shoulder impingement syndrome. J Am Chiropr Assoc 2007;44:6-15. [Google Scholar | PubMed]
- 9.El Gharbawy NH, Labib HS. Role of platelet rich plasma (PRP) injection in treatment of rotator cuff tear. Egypt Rheumatol Rehabil 2020;47:30. [Google Scholar | PubMed]
- 10.Rha DW, Park GY, Kim YK, Kim MT, Lee SC. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: A randomized controlled trial. Clin Rehabil 2013;27:113-22. [Google Scholar | PubMed]
- 11.Nejati P, Ghahremaninia A, Naderi F, Gharibzadeh S, Mazaherinezhad A. Treatment of subacromial impingement syndrome: Platelet-rich plasma or exercise therapy? a randomized controlled trial. Orthop J Sports Med 2017;5: [Google Scholar | PubMed]
- 12.Dickens VA, Williams JL, Bhamra MS. Role of physiotherapy in the treatment of subacromial impingement syndrome: A prospective study. Physiotherapy 2005;91:159-64. [Google Scholar | PubMed]
- 13.Wirth MA, Basamania C, Rockwood CA. Nonoperative management of full-thickness tears of the rotator cuff. Orthop Clin North Am 1997;28:59-67. [Google Scholar | PubMed]
- 14.Rossi LA, Piuzzi N, Giunta D, Tanoira I, Brandariz R, Pasqualini I, et al. Subacromial platelet-rich plasma injections decrease pain and improve functional outcomes in patients with refractory rotator cuff tendinopathy. Arthroscopy 2021;37:2745-53. [Google Scholar | PubMed]
- 15.Ebert JR, Wang A, Smith A, Nairn R, Breidahl W, Zheng MH, et al. A midterm evaluation of postoperative platelet-rich plasma injections on arthroscopic supraspinatus repair: A randomized controlled trial. Am J Sports Med 2017;45:2965-74. [Google Scholar | PubMed]