With careful patient selection, Arthroscopic assisted reduction and internal fixation is an effective adjunct for treating tibial fractures.
Dr. Meet Shah, Department of Orthopaedics, Dr. D.Y. Patil Medical College Hospital and Research Institute, Pimpri-Chinchwad, Maharashtra, India. E-mail: mbbs_ms_meetshah@yahoo.com
Introduction: Tibial plateau fractures, which constitute approximately 1% of all fractures with an incidence of 10.3/100,000 annually, result from varus or valgus forces combined with axial loading in the knee. These fractures display a bimodal distribution, affecting younger individuals through high-velocity trauma and older individuals through low-energy trauma. Proper management is critical due to the tibial plateau’s role as a load-bearing surface; inadequate treatment can lead to functional impairment and early osteoarthritis. Utilizing the Schatzker classification, this study categorizes tibial plateau fractures to streamline treatment and reproducibility.
Objectives: The objective of the study was to assess the functional and radiological outcomes in the patients operated with arthroscopic assisted reduction and internal fixation (ARIF).
Materials and Methods: This prospective analytical study conducted at a tertiary care hospital evaluates the functional and radiographic outcomes of 20 patients with Schatzker Type 1–4 tibial plateau fractures treated using ARIF. Patients excluded were those with Schatzker Type 5 and 6 fractures due to the increased risk of compartment syndrome from fluid extravasation during arthroscopy. Surgical procedures aimed to achieve anatomical reduction, proper alignment, stable fixation, early mobilization, and minimal soft-tissue damage.
Results: The study conducted in the cohort which constituted of 20 patients with a mean age of 44.3 years with 9 males and 11 females and fracture distribution being Schatzker 1/2/3/4: 3/5/10/2, respectively, found ARIF advantageous in diagnosing and treating articular cartilage and soft-tissue injuries, minimizing soft-tissue dissection, and reducing the need for extensive arthrotomy. The results demonstrated good to excellent outcomes in 85% of patients, with no depression in 70% of cases and no varus/valgus malalignment in 80% of cases after 18 months. However, the technique posed challenges such as increased operative time and a steep learning curve.
Conclusion: ARIF had favorable radiological and functional outcomes in the patient who was selected after careful evaluation.
Keywords: Arthroscopy, Tibia fractures, Trauma, schatzker, arthroscopy assisted reduction
Tibial plateau fractures have an annual incidence of 10.3/100,000 trauma cases, approximately 1% of all fractures [1]. These fractures result from varus or valgus forces combined with axial loading during knee flexion or extension [2,3]. The epidemiology of tibial plateau fractures appears bimodal, with younger individuals typically affected by high-velocity trauma and older individuals by low-energy trauma [4]. Despite their rarity, treating tibial plateau fractures is crucial because the tibial plateau is a critical weight-bearing area in the body. Improper treatment can lead to functional impairments and early-onset osteoarthritis [5]. Classification of these fractures often utilizes systems like the Schatzker classification for simplicity and reproducibility. Management options range widely, including immobilization, skeletal or skin traction, percutaneous screw fixation, and open reduction internal fixation with plating, among others. The primary goals of treatment are: (A) achieving anatomical reduction of the articular surface, (B) correcting varus/valgus alignment, (C) ensuring stable fixation, (D) facilitating early mobilization, and (E) minimizing soft-tissue damage [6]. Tibial plateau fractures frequently involve significant soft-tissue injuries, with associated rates of meniscus injuries up to 71%, anterior cruciate ligament injuries in 51%, posterior cruciate ligament injuries in 25%, and collateral ligament injuries in 5%. In response to these challenges, arthroscopic assisted reduction and internal fixation (ARIF) has emerged as a new management modality. ARIF offers advantages such as precise diagnosis and treatment of articular cartilage and soft-tissue injuries, minimal soft-tissue dissection, reduced need for arthrotomy, and preservation of the anterior horn of the meniscus, thereby reducing morbidity and promoting early mobilization. Potential drawbacks include increased operative time, extravasation of fluid into the injured limb, and potentially less rigid fixation [7].
The aims of this study were as follows:
- To assess the functional outcomes post-operative using Knee Society score
- Radiographical assessment using the Rasmussen score [8].
For simplicity and reproducibility, we use the Schatzker classification to categorize tibial plateau fractures based on their articular involvement and severity. The classification system grades fractures as follows: Grade 1 involves a lateral condyle split fracture, Grade 2 includes a lateral condyle split with depression, Grade 3 comprises a purely depressed lateral condyle fracture, Grade 4 is a medial condyle split fracture, Grade 5 represents a bicondylar fracture, and Grade 6 is a bicondylar fracture with metaphyseal extension [9].
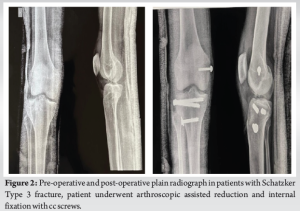
This prospective analytical study was conducted at a tertiary care hospital and included 20 patients: 10 with Schatzker Type 3 fractures, 5 with Type 2 fractures, 3 with Type 1 fractures, and 2 with Type 4 fractures. The study focused on closed tibial plateau fractures classified as Schatzker Types 1 to 4, with follow-up available for up to 18 months. The sample size was calculated considering the incidence of tibial plateau fracture as 1% of all fractures and statistical significance set at 95%. Patients with Type 5 and 6 fractures were excluded due to the unsuitability of arthroscopic reduction techniques for bicondylar fractures, which pose a higher risk of complications such as compartment syndrome, pathological fractures, contralateral fractures, and open injuries graded Gustillo Anderson 2 and above, as well as those with ligament injuries [10]. On admission, patients underwent skin traction and ice compression, with careful evaluation of skin condition for ecchymosis or blister formation. Surgery was scheduled once optimal skin condition was confirmed, typically within 1–7 days post-admission, depending on individual patient assessments. During surgery, patients were positioned supine on the operating table with thigh root support to allow unrestricted varus or valgus knee positioning, and a bolster was placed at approximately 90° of flexion. A thigh tourniquet was applied and inflated appropriately, with an image intensifier positioned on the operative side. Under anesthesia, a meticulous clinical examination for ligament laxity was performed. An anterolateral portal was established for joint visualization, while an anteromedial portal was used for instrumentation and irrigation. Hematoma evacuation from the joint, a time-consuming step, was followed by the potential creation of a superolateral portal for improved visibility, allowing for debridement with a shaver if necessary. Comprehensive arthroscopic examination of the knee assessed peripheral plateau fractures and meniscus status; techniques such as passing a loop from medial to lateral were utilized as recommended by Carro [11].
Techniques of reduction
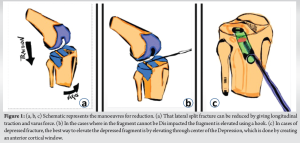
Reduction of Schatzker Type 1 fractures is typically straightforward. Under fluoroscopic guidance, longitudinal traction is applied along with varus force to elevate the lateral fragment, which is then stabilized using two percutaneous wires. For fragments that resist reduction, force is applied at the fracture site using a square driver or spatula against the cortex. Alternatively, a pin can be inserted through the fracture site to act as a lever, similar to the Kapandji technique used for Colle’s fractures. If reduction remains challenging, a slender spatula or palpation hook may be inserted into the joint cavity to disimpact the bone fragments [10]. In cases where reduction is achieved, one or two K-wires are inserted into the fractured plateau to serve as a joystick for elevating the fragment and correcting any rotational displacement. Once ideal positioning is achieved, percutaneous K-wires are used to maintain reduction, which is confirmed via fluoroscopy. For Schatzker Type 3 fractures with subchondral depression, reduction involves lifting the depressed fragment under direct visualization. An instrument introduced through an anterolateral cortical window or directly through the fracture site is used to elevate the cancellous bone beneath the depressed fragment. Central elevation of the depression is critical for achieving a good reduction. An anterior cortical window may also be created to elevate the depressed fragment while minimizing damage to the condyle. In mixed fractures such as Schatzker Type 2 (depressed plus split), the depression is typically addressed first. Once elevated, the split fracture is stabilized using large bone forceps, followed by percutaneous pinning under fluoroscopic guidance to secure the reduction in place. This is depicted in Fig. 1 Image source [12].
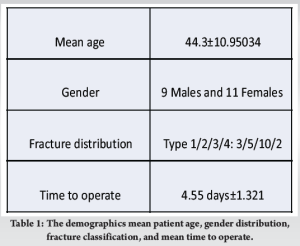
The mean age of patients in the study was 44.3 years. The distribution of fracture types included 10 patients with Type 3 fractures, five patients with Type 2 fractures, three patients with Type 1 fractures, and two patients with Type 4 fractures. The patient distribution was nine males and 11 females. The mean time to operate was 4.55 days from the day of presentation. The study mandated a minimum follow-up period of 18 months, with patients not meeting this criterion being excluded. At approximately 18 months postoperatively, each patient’s Rasmussen score and Knee Society Score were calculated. The Rasmussen score is a clinical and radiological scoring system used to assess the outcome of knee fractures, particularly tibial plateau fractures. It evaluates both functional and radiological outcomes to provide a comprehensive assessment of knee joint recovery. Radiological outcomes are compared by articular depression, angular malalignment and condylar widening. In our study, 12 patients (60%) underwent fixation with plating and the remaining 8 (40%) underwent fixation through percutaneous screws. The demographics of the same are represented in Table 1.
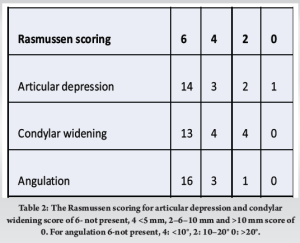
Regarding articular depression outcomes, 14 out of 20 patients (70%) showed no depression, while 3 patients (15%) exhibited <5 mm of articular depression. In addition, 2 patients (10%) showed 6–10 mm of depression, and 1 patient (5%) had more than 10 mm of articular depression. In terms of varus/valgus alignment, 16 out of 20 patients (80%) showed no malalignment, whereas 3 patients (15%) had <10° of angulation, and 1 patient (5%) exhibited 10–20° of varus/valgus alignment. Condylar widening was observed in varying degrees: 13 patients (65%) showed no widening, 4 patients (20%) had <5 mm of widening, and 3 patients (15%) exhibited 6–10 mm of widening. These data are shown in Tables 2 and 3.
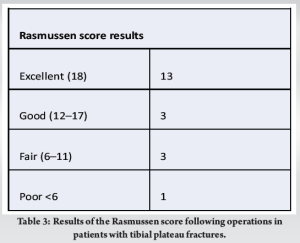
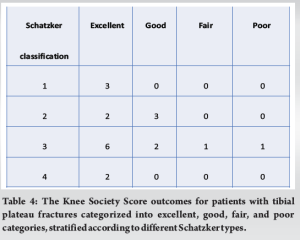
When considering outcomes by Schatzker classification, all five patients with Type 1 and Type 4 fractures achieved excellent results (100%). Among the five patients with Type 2 fractures, 2 patients (40%) had excellent results, and 3 patients (60%) had good results. For the 10 patients with Type 3 fractures, 6 patients (60%) achieved excellent results, 2 patients (20%) had good results, 1 patient (10%) had fair results, and 1 patient (10%) had poor results. An association between condylar widening and functional knee scores, based on the Knee Society Score, was observed. Among the three patients with 6–10 mm of condylar widening, 2 patients (66.66%) showed fair/good scores and 1 patient (33.33%) had a poor score. In contrast, among the 17 patients with no condylar widening or <5 mm of widening, 14 patients (82.35%) achieved excellent scores, while 3 patients (17.64%) had good to fair scores. This is shown in Table 4. When comparing the outcomes of patients based on the modality of fixation, those treated with percutaneous screws mainly had Schatzker Type 1 and Type 4 fractures. Among the remaining patients, two had Schatzker Type 2 fractures and one had a Type 3 fracture. Of these, six patients had excellent functional and radiological outcomes, one patient had a good outcome, and one had a fair outcome.
For patients treated with plate fixation, three had Schatzker Type 2 fractures. Among these, one patient had an excellent outcome, and two had good outcomes. Plate fixation was predominantly used for Type 3 fracture fixation. Out of the nine patients undergoing plate fixation, five had excellent outcomes, two had good outcomes, one had a fair outcome, and one had a poor outcome. Plain radiograph of fixation in patient pre-operative and post-operative is shown in Fig. 2.
Tibial plateau fractures exhibit a bimodal distribution, with younger individuals often affected by high-velocity trauma. Managing these fractures remains a contentious topic due to their complex geometric patterns and associated high complication rates [13,14]. The primary goals of treatment include (A) achieving anatomical reduction of the articular cartilage, (B) ensuring proper varus/valgus alignment, (C) achieving stable fixation, (D) facilitating early mobilization, and (E) minimizing soft-tissue damage [6]. Diagnosis typically involves plain radiographs, complemented by computed tomography scans for detailed fracture morphology assessment. While magnetic resonance imaging may aid in detecting ligamentous injuries, its utility in acute trauma is limited by tissue edema. Arthroscopic evaluation plays a crucial role in diagnosing ligamentous and soft-tissue injuries, often considered the gold standard for evaluation. The optimal method of fixation for reducing these fractures remains a subject of debate regarding biomechanical stability. In our study, 12 patients underwent plate osteosynthesis, typically applied to the anterolateral surface, while eight patients received percutaneous screw fixation. ARIF have become standard in managing Schatzker types 1–4 fractures. However, ARIF is generally avoided for Types 5 and 6 fractures due to their complex patterns, challenging visualization, and the risk of fluid extravasation leading to compartment syndrome [7]. ARIF minimizes soft-tissue dissection and the need for arthrotomy, significantly reducing risks such as wound dehiscence and hospital stays [7]. This study highlights the significant advantages of ARIF in diagnosing and treating soft-tissue injuries associated with tibial plateau fractures. The technique facilitates excellent visualization of the joint and cartilage surfaces, thereby promoting precise reduction of the fracture and concomitant management of soft-tissue injuries. Furthermore, ARIF minimizes the need for extensive soft-tissue dissection, which is often associated with open surgical techniques, thus reducing the risk of infection and promoting quicker recovery. There is controversy surrounding the optimal fixation modality for tibial plateau fractures. Some studies suggest that percutaneous screws are biomechanically effective for managing lateral split fractures. Studies by Koval et al. and Denny et al. have demonstrated that two 6.5 mm percutaneous screws with washers are effective in this regard [15,16]. However, biomechanical studies are limited and show conflicting results. Some research indicates superior outcomes with plating for fracture management, but this claim was challenged by cadaveric studies conducted by Boisrenoult et al., which found no significant advantage of plating over percutaneous screw fixation in lateral-split fractures [17]. In our study, 12 patients (60%) underwent plating, while 8 patients (40%) underwent percutaneous screw fixation. The results demonstrate a high percentage of good to excellent outcomes, with significant improvements in functional scores and minimal complications. However, ARIF is not without its challenges, such as increased operative time, the need for specialized equipment and training, and potential complications from fluid extravasation. Despite these challenges, ARIF remains a valuable technique for the management of specific types of tibial plateau fractures, offering benefits that can enhance patient outcomes when performed by experienced surgeons [12].
Arthroscopy aids in better evaluation of the fracture patterns and in better reduction of the fragments in tibial plateau fractures, especially the depressed fragments. It also helps in evaluating soft-tissue/ligamentous injuries related to the tibial fracture. Arthroscopy allows a more accurate evaluation of the fracture reduction and allows optimal treatment of concomitant lesions without having to make an extensive arthrotomy incision, thus reducing soft-tissue damage. The study shows that the patients managed by ARIF have shown good clinical (Knee Society score) and radiological outcomes (Rasmussen scores). The drawbacks to this technique might be cost and longer duration of the procedure. As with any surgery, there may be a learning curve to ARIF technique. The ARIF may not be suitable for all types of tibial plateau fractures but when applicable has shown to be a useful tool for evaluation and reduction.
ARIF enhances precision in managing tibial plateau fractures, optimizing outcomes with minimal soft-tissue damage, when combined with careful patient selection.
References
- 1.Egol KA, Koval KJ, Zuckerman JD. Handbook of Fractures. United States: Lippincott Williams & Wilkins; 2010. [Google Scholar | PubMed]
- 2.Chen HW, Liu GD, Wu LJ. Clinical and radiological outcomes following arthroscopic assisted management of tibial plateau fractures: A systematic review. Knee Surg Sports Traumatol Arthrosc 2015;23:3464-72. [Google Scholar | PubMed]
- 3.Mendel T, Wohlrab D, Hofmann GO. Akutes Kompartmentsyndrom des Unterschenkels nach Kniegelenkarthroskopie [Acute compartment Syndrome of the lower leg duetokneearthroscopy]. Orthopade 2011;40:925-8. [Google Scholar | PubMed]
- 4.Lubowitz JH, Elson WS, Guttmann D. Part I arthroscopic management of tibial plateau fractures. Arthroscopy 2004;20:1063-70. [Google Scholar | PubMed]
- 5.Siegler J, Galissier B, Marcheix PS, Charissoux JL, Mabit C, Arnaud JP. Percutaneous fixation of tibial plateau fractures under arthroscopy: A medium-term perspective. Orthop Traumatol Surg Res 2011;97:44-50. [Google Scholar | PubMed]
- 6.Chen XZ, Liu CG, Chen Y, Wang LQ, Zhu QZ, Lin P. Arthroscopy-assisted surgery for tibial plateau fractures. Arthroscopy 2015;31:143-53. [Google Scholar | PubMed]
- 7.Jiang L, Chen E, Huang L, Wang C. Arthroscopy-assisted reduction percutaneous internal fixation versus open reduction internal fixation for tibial plateau fracture: A systematic review and meta-analysis. Orthop J Sports Med 2021;9:23259671211027838. [Google Scholar | PubMed]
- 8.Rohra N, Suri HS, Gangrade K. Functional and radiological outcome of schatzker type V and VI tibial plateau fracture treatment with dual plates with minimum 3 years follow-up: A prospective study. J Clin Diagn Res 2016;10:RC05-10. [Google Scholar | PubMed]
- 9.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res 1979:94-104. [Google Scholar | PubMed]
- 10.Ohdera T, Tokunaga M, Hiroshima S, Yoshimoto E, Tokunaga J, Kobayashi A. Arthroscopic management of tibial plateau fractures comparison with open reduction method. Arch Orthop Trauma Surg 2003;123:489-93. [Google Scholar | PubMed]
- 11.Carro PL. Arthroscopic management of tibial plateau fractures: Special techniques. Arthroscopy 1997;13:265-7. [Google Scholar | PubMed]
- 12.Burdin G. Arthroscopic management of tibial plateau fractures: Surgical technique. Orthop Traumatol Surg Res 2013;99:S208-18. [Google Scholar | PubMed]
- 13.Khan H, Grob K, Milne LP, Kuster MS. Tibial tubercle osteotomy to improve exposure in complex knee fractures: A cadaveric study and case series. Injury 2016;47:2331-8. [Google Scholar | PubMed]
- 14.Kim CW, Lee CR, An KC, Gwak HC, Kim JH, Wang L, et al. Predictors of reduction loss in tibial plateau fracture surgery: Focusing on posterior coronal fractures. Injury 2016;47:1483-7. [Google Scholar | PubMed]
- 15.Denny LD, Keating EM, Engelhardt JA, Saha S. A comparison of fixation techniques in tibial plateau fractures. Orthop Trans 1984;10:388-9. [Google Scholar | PubMed]
- 16.Koval KJ, Polatsch D, Kummer FJ, Cheng D, Zuckerman JD. Split fractures of the lateral tibial plateau: Evaluation of three fixation methods. J Orthop Trauma 1996;10:304-8. [Google Scholar | PubMed]
- 17.Boisrenoult P, Bricteux S, Beaufils P, Hardy P. Vis versus plaque vissée dans les fractures séparationenfoncement du plateau tibial latéral. Rev Chir Orthop 2000;86:707-11. [Google Scholar | PubMed]











