Subacromial dislocation of the clavicle at the acromioclavicular joint with associated scapular spine fracture is exceedingly rare and can be successfully managed with open reduction of the acromioclavicular joint, followed by open reduction and internal fixation of the scapular spine without the need for subsequent coracoclavicular ligament reconstruction.
Dr. Jake A Fox, Vanderbilt University Medical Center, Department of Orthopaedic Surgery, 1215 21st Ave S, Suites 3200 and 4200, Nashville, TN, 37232. E-mail: Jake.a.fox14@gmail.com
Introduction: Inferior or subacromial dislocation of the distal clavicle is a rare entity. Previous reports of this injury pattern have largely been limited to Rockwood VI acromioclavicular joint (AC) dislocations, with the distal clavicle located in the subcoracoid position. Few case reports have been described with the inferior clavicle being located in the subacromial space, and these have all been previously associated with clavicle fractures. To our knowledge, no previous case report exists in the literature with this AC joint injury and associated scapular spine fracture.
Case Report: Here, we report on a case of a 30-year-old right-hand dominant African American male who suffered a high-energy left-sided inferior distal clavicle dislocation with an associated scapular spine fracture that was successfully treated with open reduction of the AC joint dislocation, followed by open reduction and internal fixation (ORIF) of the scapular spine fracture. After ORIF of the scapular spine and reduction of the AC joint, the AC joint was deemed to be a capsular injury with intact ligaments, so a simple capsular repair was performed. We also summarize the existing literature on this topic.
Conclusion: Inferior dislocation of the clavicle into the subacromial space with an associated scapular spine fracture is an extremely rare injury which has not been previously reported. This injury can successfully be managed by first reducing the AC joint, and then proceeding with anatomic reduction and fixation of the scapular spine with good functional result. The ligaments surrounding the AC joint in the subacromial pattern are often intact, and the dislocation is a result of capsular injury. This leads us to believe that subtyping the Rockwood VI classification to VIa (subacromial) and VIb (subcoracoid) would be useful for orthopedic surgeons due to differences in associated injury and subsequent operative management.
Keywords: AC joint, clavicle, scapula, Rockwood.
Acromioclavicular joint (AC) injuries are relatively common injuries in otherwise healthy patients, with a frequency of 9.2 per 1000 person years and 2.1 times higher incidence in males [1]. These injuries have historically been broken down into six types by Rockwood et al., with type VI being subcoracoid/subacromial clavicular dislocation [2]. Inferior dislocation (or subacromial dislocation) of the distal clavicle is an exceedingly rare entity. Patterson reported the first case of this in 1967 [3]. The mechanism of injury to cause this pattern is thought to be hyperabduction of the shoulder with associated retraction of the scapula. This injury can be associated with multiple injuries including scapula fracture, rib fractures, clavicle fracture, and accessory nerve damage [4]. Patients typically present with AC joint pain, limited range of motion, swelling/ecchymosis to the involved shoulder, and varying degrees of neurologic symptoms. Previous reports of inferior dislocation of the distal clavicle have been isolated to case reports of Rockwood type VI AC joint dislocations with the distal clavicle being dislocated in the subcoracoid position [3-9]. However, the pattern of inferior distal clavicle dislocation in the subacromial space, not subcoracoid, has been further limited to four case reports to our knowledge, all of which were associated with midshaft clavicle fractures [10-13]. We report on a unique case of a 30-year-old male who was involved in a motor vehicle collision and suffered an inferior dislocation of the clavicle at the AC joint with an associated scapular spine fracture, which was successfully treated with surgery. To the best of our knowledge, such a presentation of AC joint injury with an associated scapular spine fracture has not been previously reported in the literature.
A 30-year-old right-hand dominant male was evaluated in the orthopedic clinic 9 days after his injury. He was the passenger in a motor vehicle collision where his car was hit by another car going about 30 miles/h, and his car flipped over a curb. He was able to self-extricate from the motor vehicle. He was seen in the local emergency department (ED) and diagnosed with a left shoulder inferior (subacromial) distal clavicle dislocation with a displaced scapular spine fracture (Fig. 1-4). Other workup in the ED, including CT of his chest/abdomen and pelvis, were negative for any other injuries. It was also noted that he had an Os Acrominale. When he was evaluated in the orthopedic clinic, his inferior clavicle dislocation was noticed to be a mechanical block to abduction and forward elevation. He was also having significant pain in the lateral shoulder radiating down the ipsilateral ribs. Due to his age, activity level, pain level, and restrictions in range of motion, he was indicated for surgery.
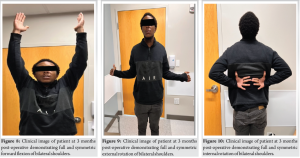
During the surgery, he was placed in a lateral position on a bean bag with his arm in a Trimano arm positioner (Arthrex, Naples, Florida). A 6 cm horizontal incision was made just distal to his scapular spine. The posterior deltoid was released from the scapular spine, leaving a 1 cm cuff for later repair. The supraspinatus and infraspinatus were gently elevated from the superior and inferior aspects of the scapular spine with a wood-handle AO elevator to access the fracture site, with care taken to protect the suprascapular nerve and artery pedicle. An attempt was made to reduce the scapular spine fracture, but anatomic reduction was not possible. It was thought that the inferiorly dislocated clavicle was blocking the reduction. An attempt at a closed reduction of the AC joint was unsuccessful. Therefore, a 3 cm horizontal incision was made over the AC joint. The superior AC joint capsule was incised horizontally for later repair. The distal clavicle was controlled with a small point-to-point reduction clamp and a small Hohman was used as a shoehorn to reduce the inferior clavicle dislocation with medial traction from the clamp. Concentric AC joint reduction was confirmed with C-arm fluoroscopy. After the reduction of the AC joint, the scapular spine was easily reduced to an anatomic position. Two 3.5 mm Arthrex cannulated headless compression screws were placed perpendicular to the fracture line. Then, a 2.7 mm Synthes locking plate was placed on the inferior surface of the scapular spine, and multiple locking screws were placed. Next, an Accumed contralateral side clavicle plate was placed on the superior surface of the scapular spine and two locking screws were placed on each side of the fracture. Dual plates were used in order to increase the points of fixation on the thin shelf of the scapular spine. After the scapular spine was fixed, the distal clavicle was evaluated for stability. The AC joint remained stable to superior/inferior translation and was horizontally stable after the open reduction. It was deemed that the injury represented a capsular injury and the coracoacromial (CA) and coracoclavicular (CC) ligaments were still intact. The AC joint capsule was then repaired with a pants-over vest suture configuration with a 0-vicryl suture in order to imbricate the superior capsule. A 1.9 Arthrex double-loaded fibertak anchor was then placed in the acromion. Each limb of the suture was then krakowed along the superior capsule and tied down to supplement the AC joint capsular repair. His rehab protocol consisted of a sling for 6 weeks. He started pendulum range of motion at the 4-week mark from his surgery date then transitioned to passive range of motion and active range of motion under the guidance of in-person physical therapy. At 9 weeks from surgery, he demonstrated near-complete union of his scapular spine fracture and maintenance of reduction of his AC (Figs. 5-7). At that time, he had no tenderness to palpation of his fracture site or AC joint, so he was allowed to return to work as a line assemblyman. He was also cleared for all activities at 9 weeks post-operative. He started strengthening of the shoulder rotator cuff and periscapular muscles at the 10-week mark from his surgery. At the 3-month post-operative visit, his range of motion was noted to be excellent, with full and symmetric forward flexion, external rotation, and internal rotation (Figs. 8-10). At his 10-week and 3-month follow-up time point, there was no tenderness to palpation at the scapular spine or AC joint. At the 3-month mark, he also had full strength of his rotator cuff, deltoid, and periscapular muscles. He is quite pleased with his functional result and is back to doing all activities he was doing before injury.
AC joint separations in isolation are common injuries that are frequently seen in the ED and clinic by orthopedic surgeons [1]. The majority of AC joint injuries can be managed nonoperatively, but type VI injuries most always necessitate surgical intervention. The management of inferior clavicle dislocations reported previously has most frequently been in regard to the subcoracoid subtype [3-9]. The subacromial subtype of inferior clavicle dislocation has only been reported in the literature four times previously [10-13]. Koka and D’Arcy were the first authors to report on a patient with an inferior clavicular dislocation into the subacromial space, and the patient also had a midshaft clavicle fracture [12]. They advocated for open reduction of the AC joint and pinning of the AC joint, which led to spontaneous reduction of the clavicle fracture. Juhn and Simonian were the next to report a midshaft clavicle fracture with a more mild dislocation of the clavicle into the subacromial space in a 21-year-old ice hockey player [11]. He was initially seen in clinic by the orthopedic surgeon approximately 1 week following his injury. He was symptomatically doing great and had no sagittal plane deformity, so they elected to proceed with non-operative management. The patient was back to full hockey activities at 14 weeks and did very well, which they were surprised by. Davies et al. also reported on a case of a 40-year-old female with a midshaft clavicle fracture and subacromial clavicular dislocation. They proceeded with operative fixation of the clavicle fracture at 10 weeks post-injury, and they found the AC joint to spontaneously reduce following reduction of the clavicle fracture. Given the stability of the AC joint following reduction and intact CC/CA ligaments, they elected not to provide any further stabilization. Milchteim et al. reported a similar case of a midshaft clavicle fracture and subacromial clavicle dislocation [13]. They also reported reduction and fixation of the midshaft clavicle fracture leading to reduction of the AC joint with inherent stability. The uniqueness of our case presentation lies in the fact that our patient had an associated scapular spine fracture, which has not been presented previously. One key point to highlight in our case is that the AC joint had to first be reduced before we were able to achieve anatomic reduction of the scapular spine. During surgery, the inferior dislocation of the clavicle was thought to be blocking the reduction of the scapular spine. It was also helpful to use cannulated screws to fix the scapular spine primary fracture line, as the trajectory can be difficult if drilling freehand. Given the bony geometry of the scapular spine, we also think utilization of dual plating technique confers the highest degree of stability. In addition, we think that it is important to reinforce the notion previously suggested [10,11] that in the subacromial variant of the Rockwood VI classification, the CC/CA ligaments are likely to be intact. This implies that once the associated fracture is stabilized, the AC joint will, in all likelihood, be stable without any reinforcement. However, after reduction of the AC joint, the stability was tested. If the CC ligaments were thought to be incompetent one should be prepared to perform an anatomic AC joint reconstruction. One important consideration in the evaluation of our patient was the concept and importance of claviscapular motion when it comes to shoulder function [14]. The clavicle and scapula must be appropriately coupled with humeral movement to maintain ball-and-socket kinematics through overhead range of motion. If the clavicle and scapula become uncoupled, this can lead to scapular dyskinesis and impaired shoulder complex function. Scapular dyskinesis is associated with scapular protraction and glenoid anti-tilt which leads to diminished upper extremity function [14]. This concept gave us further belief that our patient would greatly benefit from surgical fixation of the scapula and anatomic reduction of the AC joint. We lastly think that further subtyping the Rockwood VI variant into VIa (subacromial) and VIb (subcoracoid) would be a meaningful delineation clinically, as previously suggested by Juhn and Simonian, Davies, and Grossi [4,10,11]. The most important factor is that the CC/AC ligaments are often intact in the subacromial pattern, while they are typically not intact in the subcoracoid variant. This is likely explained by the subcoracoid pattern being caused from a higher energy mechanism leading to increased soft-tissue trauma [10]. This delineation of subtype occasionally is made with advanced imaging in the form of CT scan, as radiographs can be subtle and need to be carefully scrutinized. After reduction of the AC joint intraoperatively, it is critical to assess for vertical stability of the joint with manual superior/inferior translation and horizontal stability with anterior/posterior translation. In the subacromial variant, often capsular repair is all that is indicated. While in the subcoracoid variant, reconstruction of the CC ligaments is often needed to restore vertical stability of the AC joint and lead to a satisfactory functional outcome.
Inferior dislocation of the clavicle into the subacromial space with an associated scapular spine fracture is an exceedingly rare injury which has not been previously reported. This injury can successfully be managed by first reducing the AC joint, and then proceeding with anatomic reduction and fixation of the scapular spine with good functional result. The ligaments surrounding the AC joint in these injuries are often intact, and the dislocation is a result of capsular injury. This leads us to believe that subtyping the Rockwood VI classification to VIa (subacromial) and VIb (subcoracoid) would be useful for orthopedic surgeons due to differences in associated injury and subsequent operative management.
This article summarizes the presentation, diagnosis, treatment, and outcome of a young patient who suffered an inferior clavicle dislocation at the AC joint with an associated displaced scapular spine fracture following a motor vehicle collision. The management of this injury has not been described previously, and we describe a surgical treatment algorithm for reducing the AC joint and stabilizing the scapula spine fracture. We describe to the audience the key differences in the subcoracoid Rockwood VI variant compared to the subacromial Rockwood VI variant.
References
- 1.Pallis M, Cameron KL, Svoboda SJ, Owens BD. Epidemiology of acromioclavicular joint injury in young athletes. Am J Sports Med 2012;40:2072-7. [Google Scholar | PubMed]
- 2.Rockwood CA. The Shoulder. Amsterdam: Elsevier Health Sciences; 2009. p. 1696. [Google Scholar | PubMed]
- 3.Patterson WR. Inferior dislocation of the distal end of the clavicle. A case report. J Bone Joint Surg Am 1967;49:1184-6. [Google Scholar | PubMed]
- 4.Grossi EA, Macedo RA. Acromioclavicular dislocation type VI associated with diaphyseal fracture of the clavicle. Rev Bras Ortop 2013;48:108-10. [Google Scholar | PubMed]
- 5.Canbora KM, Tüzüner T, Yanik SH, Görgeç M. Subcoracoid dislocation of the acromioclavicular joint. Acta Orthop Traumatol Turc 2011;45:463-5. [Google Scholar | PubMed]
- 6.Fenn S, Medlar C, Hatz B, Jarmin M. Subcoracoid acromioclavicular joint dislocation (Rockwood type VI) sustained in motorcycle crash: A case report. Radiol Case Rep 2023;18:1267-71. [Google Scholar | PubMed]
- 7.Gerber C, Rockwood CA Jr. Subcoracoid dislocation of the lateral end of the clavicle. A report of three cases. J Bone Joint Surg Am 1987;69:924-7. [Google Scholar | PubMed]
- 8.McPhee IB. Inferior dislocation of the outer end of the clavicle. J Trauma 1980;20:709-10. [Google Scholar | PubMed]
- 9.Torrens C, Mestre C, Pérez P, Marin M. Subcoracoid dislocation of the distal end of the clavicle. A case report. Clin Orthop Relat Res 1998;348:121-3. [Google Scholar | PubMed]
- 10.Davies EJ, Fagg JA, Stanley D. Subacromial, supracoracoid dislocation of the acromioclavicular joint with ipsilateral clavicle fracture: A case report with review of the literature and classification. JRSM Open 2014;5 (7) [Google Scholar | PubMed]
- 11.Juhn MS, Simonian PT. Type VI acromioclavicular separation with middle-third clavicle fracture in an ice hockey player. Clin J Sport Med 2002;12:315-7. [Google Scholar | PubMed]
- 12.Koka SR, D’Arcy JC. Inferior (subacromial) dislocation of the outer end of the clavicle. Injury 1993;24:210-1. [Google Scholar | PubMed]
- 13.Milchteim C, Doppelt JD, Neviaser RJ. Subacromial dislocation of the acromioclaviclular joint with associated fracture of the clavicle. J Shoulder Elbow Surg 2018;27:e297-9. [Google Scholar | PubMed]
- 14.Kibler WB, Sciascia AD, Grantham WJ. The shoulder joint complex in the throwing motion. J Shoulder Elbow Surg 2024;33:443-9. [Google Scholar | PubMed]