Careful attention to technical aspects, especially the selection of implants and the unique anatomy involved, is crucial in planning for execution of TKR in varus deformity with MHE using standard instrumentation.
Dr Peeyush Belsare, Department of Joint Replacement, Deenanath Mangeshkar Hospital, Erandawane, Pune, Maharashtra, India. E-mail: peeyushbelsare.03@gmail.com
Introduction: Multiple hereditary exostosis (MHE) is a genetic condition inherited in an autosomal dominant manner, resulting from point mutations in exostosin genes. Knee deformities, such as genu valgus, are common in individuals with MHE, often localized to the proximal tibial metaphysis, and occasionally involving the femur. Osteochondromas at the knee can lead to an oblique joint line orientation, contributing to earlier onset arthritis. Increased angulation may also lead to lateral patella subluxation and patellofemoral complaints, necessitating earlier interventions compared to the general population. While total knee arthroplasty (TKA) for osteoarthritis in MHE with varus deformity is rarely reported in the literature, we present a case of a high body mass index (BMI) female with MHE and varus knee deformity successfully treated with TKA using a standard posterior stabilized implant, without additional constraints or extensive releases.
Case Report: A 54-year-old Indian woman, homemaker presented to the clinic due to progressive left knee pain and varus deformity. Her BMI was 40. With no significant family history. The surgery was performed using a tourniquet. Using standard instrumentation for conventional TKA. The angle of bone resection was determined preoperatively through manual radiographic templating. The sizing of femoral component was done precariously since the anatomy of distal femur was altered with no prominent anterolateral ridge and an anterior referencing system was done to avoid notching. Tibial rotational alignment was based on anatomic landmarks. Patellofemoral tracking was excellent and did not require lateral retinacular release.
Conclusion: Careful attention to technical aspects, selection of implants and the unique anatomy involved, is crucial in planning this procedure. Ensuring proper balance of the ligaments tented by the osteochondromas and meticulous sizing of the femur are essential for favorable functional outcomes in such cases.
Keywords: Multiple hereditary exostosis, total knee arthroplasty, osteoarthritis of knee.
Multiple hereditary exostosis (MHE) is a genetic condition inherited in an autosomal dominant manner, resulting from point mutations in exostosin genes [1]. Mutations in exostosin-1 gene are associated with severe clinical outcomes, including an elevated risk of malignancy [2]. The exact prevalence of MHE is challenging to determine due to a significant number of asymptomatic and unreported cases, though it is considered rare, affecting approximately 1 in 50,000 individuals [3]. MHE is characterized by the development of multiple pedunculated or sessile cartilage-capped bony outgrowths, composed of cortex and marrow cavity continuous with the host bone. These growths commonly lead to joint deformities, restricted range of motion (ROM), and early-onset osteoarthritis [3]. Osteochondromas typically arise on the lateral side of active growth plates of long bones, with diagnosis often occurring within the first decade of life in over 80% of cases [3]. Additional features associated with MHE include limb-length discrepancies (10–50%), as well as asymmetry in pectoral and pelvic structures and short stature (37–44%) [4,5]. The knee is the most frequent site affected by exostoses in MHE, with involvement of the distal femur and proximal tibia ranging from 70% to 98%, while the fibula is affected less commonly (30–97%) [5]. Complications associated with MHE encompass aneurysms/pseudoaneurysms, arterial/venous thrombosis, neurovascular compromise, and rarely, malignant transformation [6]. Knee deformities, such as genu valgus, are common in individuals with MHE, often localized to the proximal tibial metaphysis, and occasionally involving the femur. Osteochondromas at the knee can lead to an oblique joint line orientation, contributing to earlier onset arthritis. Increased angulation may also lead to lateral patella subluxation and patellofemoral complaints, necessitating earlier interventions compared to the general population [7,8]. Surgical management of MHE affecting the knee typically includes resection of symptomatic exostoses, correction of joint deformities through osteotomies, and alignment procedures to address limb-length inequalities [5,9]. While total knee arthroplasty (TKA) for osteoarthritis in MHE with varus deformity is rarely reported in the literature, we present a case of a high body mass index (BMI) female with MHE and varus knee deformity successfully treated with TKA using a standard posterior stabilized implant, without additional constraints or extensive releases.
Pre-operative evaluation
A 54-year-old Indian woman, homemaker presented to the clinic due to progressive left knee pain and varus deformity. Her BMI was 40With No significant family history. On thorough physical examination, inspection of the left lower extremity revealed varus deformity of the knee, and no protruding or visible masses because of obesity. Palpation of the left knee elicited pain along the medial joint line. Patellar evaluation failed to reveal hypermobility, but patellofemoral crepitus was present with intact distal neurovascular status. Left knee ROM was 0–90. The varus deformity of the left knee was partially correctable. Pre-operative Knee Society Knee Score was 19.4 and Function Score was 25, for a total Knee Society Score of 69 and Oxford Knee Score of 19 on 48. Radiographic imaging using anteroposterior and lateral views showed grade IV OA Kellgren-Lawrence with 3 radiopaque sessile growths affecting the proximal medial and lateral portions of the left tibia and proximal fibula with 1 pedunculated growth over medial aspect of proximal tibia and 3 sessile and 1 pedunculated growths over distal femur. Given the patient’s clinical presentation, family history, and radiological findings, a clinical diagnosis of MHE was made and TKA was recommended in view of pain not controlled with conservative management.
Surgical technique
The surgery was performed by the senior author using a tourniquet. Using standard instrumentation for conventional TKA, the angle of bone resection, depth of resection, and femoral and tibial rotational alignment were carefully considered. The angle of bone resection was determined preoperatively through manual radiographic templating. We used an anterior midline incision and standard medial para-patellar arthrotomy. The altered anatomy in this case warranted meticulous dissection during the anteromedial-subperiosteal release of deep Medial Collateral Ligament due to the sessile osteochondroma and capsule as well as careful medial retraction to avoid excessive strain on the MCL and avoid fracture of the exostosis. This was followed by preparation of the femoral and tibial components. The distal femoral cut was done at 5 of valgus. The proximal tibia cut was performed using 8 mm from the lateral resection as reference. The extension gap obtained was symmetric. The final measure of the extension gap was 9 mm. The transepicondylar axis and the Whiteside line were used to establish femoral rotation. The sizing of femoral component was done precariously since the anatomy of distal femur was altered with no prominent anterolateral ridge and an anterior referencing system was done to avoid notching all costs. Tibial rotational alignment was based on anatomic landmarks. Flexion-gap balancing required release of the semi-membranosus without excision of peri-articular osteochondromas which were asymptomatic and their excision would need extensive dissection. Trials were performed using standard posterior stabilized polyethylene insert. No instability in extension, mid-flexion, and flexion was encountered. Patellofemoral tracking was excellent using the “no thumb rule” and did not require lateral retinacular release.
Based on the favorable intraoperative findings, a MAXX Meril Opulent knee system was used for implantation. Post-operative Ipsilateral ankle dorsiflexion was comparable to pre-operative ROM. Full extension and 90 of flexion were obtained before discharge, with full weight-bearing walking as tolerated.
Post-operative evaluation
Post-operative evaluation at 1 year revealed correction of the varus deformity left knee ROM was 0–120, and ipsilateral ankle dorsiflexion was equivalent to that observed during pre-operative evaluation. Post-operative radiographic imaging using anteroposterior and lateral views demonstrated proper anatomical alignment and no signs of prosthesis loosening. Post-operative knee society knee score was 68 and functional score was 84 and oxford score was 42/48 and forgotten joint score was 90. There were no post-operative complications, and the patient was able to perform her normal daily activities without difficulty. The patient provided the authors with informed consent to report this case in the literature (Fig. 1-4 and Table 1).



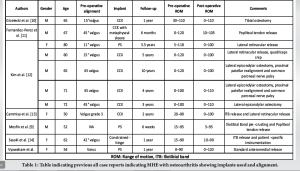
MHE by affecting the long and flat bones often leads to severe deformities hence complicating the surgical management of these patients. The majority of patients with MHE and knee involvement are managed with exostosis removal and deformity correction [8]. TKA for patients with hereditary multiple exostoses has been described only for valgus knees with paucity of literature on surgical management of osteoarthritis of the knee with varus deformity. In the knee, exostoses of the distal femur or proximal tibia can lead to valgus deformity. Valgus deformity can also result from a shortened fibula that further results in valgus angulation of the tibia. Careful pre-operative planning is crucial in such cases of MHE and involves meticulous templating and thorough evaluation of bone dimensions to decide whether custom implants are necessary [12]. Despite the patient being shorter in stature, a larger femoral implant was required in this case, underscoring the importance of having a range of implant sizes available to meet diverse patient needs. Moreover, the surgeon should be prepared for dealing with soft-tissue imbalances which can be caused due to the osteochondromas tenting the ligaments and tendon attachments. In the previous cases of MHE with knee involvement managed with TKA, majority cases required soft-tissue release to obtain adequate ligamentous balancing including iliotibial band and popliteus release. We were able to achieve symmetric extension and flexion gaps with standard posteromedial soft-tissue release and did not require the use of a lateral epicondylar sliding osteotomy or hinge. In the series reported by Kim et al., all five cases of TKA in MHE were in valgus (range 11°–45°), and the authors used lateral epicondyle sliding osteotomies to correct the severe valgus deformities. In their case series, four out of five required Constrained Condylar knee while only one knee would be balanced with standard Posterior Stabilized prosthesis [12]. In the case described by Mesfin et al., standard PS implant was used to manage valgus deformity of the knee in a 52-year-old gentleman with MHE but several exostosis interfering with the placement of the cutting blocks were removed [9]. In our surgical procedure, no exostosis was removed or damaged which helped in a quicker rehabilitation and less post-operative pain. Single case reported by Fernandez-Perez et al., had severe valgus with bone loss and was managed with a constrained implant and metaphyseal sleeve and fluted stem for additional fixation [11]. Grzelecki et al. have described a valgus knee with extra-articular deformity for which they performed one-stage TKA with constrained implant and tibial shaft osteotomy fixed with an intra-medullary tibial stem extension and had obtained with good results [10]. In our reported case of a 54-year-old obese woman with osteoarthritis and varus deformity of the knee without significant bone loss, standard PS knee (Maxx, Freedom) without the need for stem, constrain or augments was sufficient to balance the knee and achieve good functional outcome. Furthermore, tibial stem used during primary TKA in obese patients has not been proven to lower the rate of revision [14]. MHE carry a 0.5–25% risk of chondrosarcoma transformation [5], though it is still lower in adults (1–5%) [4]. In our case, there were no clinical or radiological signs of malignant transformation and hence were not resected. At her most recent follow-up, 1-year-after surgery, she demonstrated independence in ambulation and all daily activities, reported no knee pain, and adhered to her outpatient physical therapy regimen. These outcomes align with those reported in literature, highlighting positive clinical and functional results in the short term. However, the long-term outcomes are influenced by factors such as joint deterioration, the extent of deformity, appropriate implant choice, and effective soft-tissue management [9,12].
TKA is an effective treatment option for addressing knee osteoarthritis in individuals with MHE, providing substantial pain relief and improved functional outcomes. Careful attention to technical aspects, especially the selection of implants and the unique anatomy involved, is crucial in planning for this procedure. Ensuring proper balance of the ligaments tented by the osteochondromas and meticulous sizing of the femur are essential to prevent overstuffing of the patellofemoral joint and to ensure adequate bone coverage, resulting in favorable functional outcomes in such cases.
This is a rare presentation of a MHE with a Varus deformity of the knee which was managed with standard PS implants with careful ligament release and appropriate femoral sizing.
References
- 1.Ofiram E, Eylon S, Porat S. Correction of knee and ankle valgus in hereditary multiple exostoses using the Ilizarov apparatus. J Orthop Traumatol 2008;9:11-5. [Google Scholar | PubMed]
- 2.Jennes I, Pedrini E, Zuntini M, Mordenti M, Balkassmi S, Asteggiano CG, et al. Multiple osteochondromas: Mutation update and description of the multiple osteochondromas mutation database (MOdb). Hum Mutat 2009;30:1620-7. [Google Scholar | PubMed]
- 3.Schmale GA, Conrad EU 3rd, Raskind WH. The natural history of hereditary multiple exostoses. J Bone Joint Surg Am 1994;76:986-92. [Google Scholar | PubMed]
- 4.Bovée JV. Multiple osteochondromas. Orphanet J Rare Dis 2008;3:3. [Google Scholar | PubMed]
- 5.Stieber JR, Dormans JP. Manifestations of hereditary multiple exostoses. J Am Acad Orthop Surg 2005;13:110-20. [Google Scholar | PubMed]
- 6.Delgado MA, Martinez-Domenech G, Sarrion P, Urreizti R, Zecchini L, Robledo HH, et al. A broad spectrum of genomic changes in latinamerican patients with EXT1/EXT2-CDG. Sci Rep 2014;4:6407. [Google Scholar | PubMed]
- 7.Clement ND, Porter DE. Can deformity of the knee and longitudinal growth of the leg be predicted in patients with hereditary multiple exostoses? A cross-sectional study. Knee 2014;21:299-303. [Google Scholar | PubMed]
- 8.D’Ambrosi R, Caldarini C, Ragone V, Facchini RM. Effect of multiple hereditary exostoses on sports activity in children. J Orthop 2018;15:927-30. [Google Scholar | PubMed]
- 9.Mesfin A, Goddard MS, Tuakli-Wosornu YA, Khanuja HS. Total hip and knee arthroplasty in patients with hereditary multiple exostoses. Orthopedics 2012;35:e1807-10. [Google Scholar | PubMed]
- 10.Grzelecki D, Szneider J, Marczak D, Kowalczewski J. Total knee arthroplasty with simultaneous tibial shaft osteotomy in patient with multiple hereditary osteochondromas and multiaxial limb deformity - a case report. BMC Musculoskelet Disord 2020;21:233. [Google Scholar | PubMed]
- 11.Fernandez-Perez SA, Rodriguez JA Jr., Beaton-Comulada D, Colon-Miranda RG, Soler-Salas AH, Otero-Lopez A. Total knee arthroplasty in patients with multiple hereditary exostoses. Arthroplasty Today 2018;4:325-9. [Google Scholar | PubMed]
- 12.Kim RH, Scuderi GR, Dennis DA, Nakano SW. Technical challenges of total knee arthroplasty in skeletal dysplasia. Clin Orthop Relat Res 2011;469:69-75. [Google Scholar | PubMed]
- 13.Cammisa E, Alesi D, Meena A, Lullini G, Zaffagnini S, Maria G, et al. Overcoming the technical challenges of total knee arthroplasty in patients affected by hereditary multiple exostoses: A case report and literature review. SN Compr Clin Med 2022;4:254. [Google Scholar | PubMed]
- 14.Osan JK, Harris IA, Harries D, Peng Y, Yates PJ, Jones CW. Stemmed tibial fixation for primary total knee arthroplasty in obese patients-a national registry study. J Arthroplasty 2024;39:355-62. [Google Scholar | PubMed]










