B/L patellar tendon repair by krackow technique has very good results
Dr. Shakil Ahmad, Department of Orthopaedic Surgery, Sohar Hospital, Oman, PO Box No 987 Postal Code 311, Oman. E-mail: dr.shakilortho@gmail.com
Introduction: Among the cause of extensor mechanism failures, acute patellar tendon ruptures are less frequent than quadriceps tendon ruptures. Moreover, majority occur as unilateral injuries during athletic participation. B/L acute patellar tendon ruptures are extremely rare and only been documented in literature as case reports with majority having predisposing factors such as tendinopathy, steroid abuse systemic lupus erythematosus, and end-stage renal disease (ESRD).
Case Report: We present a case of 34-year-old male patient k/c of G6pd deficient physical therapy (PT) with ESRD on regular hemodialysis thrice a week since 8 years came to A/E with H/O pain and swelling in both knees due to a fall from stairs. Plain X-rays and magnetic resonance imaging confirmed the diagnosis of B/L patellar tendon avulsion from the lower end of patella. PT was operated according to the Krackow technique PT recovered well and we achieved excellent result in both knees.
Conclusion: Since B/L tendon rupture is extremely rare therefore there is always a high chance of missing the diagnosis due to lack of other normal knee for comparison. We want to highlight the relation of comorbidities like G6pd def, ESRD with B/L patellar tendon avulsion, and to have a high degree of suspicion if ESRD PT comes to A/E with B/L knee swelling and pain.
Keywords: Bilateral patellar tendon rupture, chronic renal failure, krackow technique, International Knee Documentation Committee score.
Among the cause of extensor mechanism failures, acute patellar tendon ruptures are less frequent than quadriceps tendon ruptures. Moreover, majority occur as unilateral injuries during athletic participation. B/L acute patellar tendon ruptures are extremely rare and only been documented in literature as case reports with the majority having predisposing factors like tendinopathy, steroid abuse systemic lupus erythematosus (SLE), end-stage renal disease (ESRD). We present a case of 34-year-old male patient k/c of G6pd deficient PT with ESRD on regular hemodialysis thrice a week since 8 years came to A/E with H/O pain and swelling in both knees due to a fall from stairs. Plain X-rays and magnetic resonance imaging (MRI) confirmed the diagnosis of B/L patellar tendon avulsion from the lower end of patella.pt was operated according to the Krackow technique PT recovered well and we achieved excellent result in both knees.
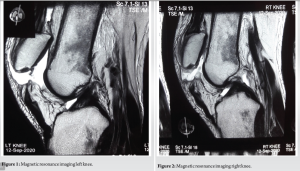
Patient 34-year-old male k/c of ESRD on regular hemodialysis with a failed renal transplant came to A/E with H/O pain and swelling in both knees due to a fall from stairs after being pushed by some person. There was twisting of both knees. On examination, we found conscious patient with B/L knee swelling with inability to flex and extend both knees. Tenderness was there in both knees with more on the right (RT) knee. Patellar tap was positive in both knees with suprapatellar fullness. Palpable infra patellar gap was present in both knees. MacMurray and Lachman tests were not possible due to pain. No distal neurovascular deficit noted in both lower limbs. Blood was aspirated from both knees. Plain X-ray’s was done which shows B/L patella Alta and to confirm the diagnosis B/L MRI was done (Fig. 1 and 2) which showed B/L patellar tendon avulsion from the lower end of patella PT was taken to the operating theatre and surgery was done.
Surgical technique
Under spinal anesthesia and tourniquet surgery of RT knee started first. A midline anterior longitudinal incision was given from 3 cm above to superior pole of the patella to the tibial tuberosity. After careful dissection, inferior pole of the patella was reached, and we found whole patellar tendon to be avulsed from inferior pole of the patella along with the entire retinaculum torn as one sleeve. After thorough washing, the inferior pole of the patella was curetted and a trough was created with fresh cancellous bed visible. 3 drill holes made in the patella along the longitudinal axis of the patella from inferior to superior pole resulting in 3 tunnels. Medial, lateral, and central tunnels patellar tendon sutured by two ethibond no. 5 by standard Krakow’s method on the medial and lateral side of the tendon resulting in four thread ends. Two central threads were passed through the middle tunnel and retrieved at the superior margin of patella. The remaining two peripheral threads were passed through medial and lateral tunnel, respectively (Fig. 3 ortho bullet.com). Tension was applied to the sutures but was only clamped but not tied lateral radiograph was obtained to assess the patellar height in relation the blumensaat line. Suture tension was adjusted and one medial knot made by tightening medial thread and one of the central thread and other lateral knot made by lateral thread and remaining central thread. Strength of construct was tested up to 90° flexion (Fig. 4 and 5). This construct was reinforced by Vicryl no 1. The retinaculum was repaired and the wound was closed in layers.

Same steps repeated for the left (LT) knee, and the findings were exactly the same as of RT knee and so exact same surgical procedure was repeated for LT knee. B/L cylindrical slab was applied in both knees.
Post-operative protocol
Sutures were removed after 2 weeks (Fig. 6) passive range of motion exercises were started at 4 weeks, and by 8 weeks postoperatively active range of motion exercises had been initiated. After that, he was allowed full knee flexion along with the focus on quadriceps and hamstring strengthening exercises. Weight-bearing was gradually started by 2 months while using a walker frame by the 10th post-operative week, the patient achieved a bilateral active complete knee flexion and extension (Figs. 7 and 8) and could walk without crutches in follow-up OPD visits his both knees were evaluated according to International Knee Documentation Committee (IKDC) subjective evaluation form and at 6 months post-operative his IKDC score for both knees was 75.86.

Patellar tendon ruptures are rare, and the majority are in young athletes having patellar tendinopathy (Jumper knee) or other enthesopathies such as Osgood schatlers disease. It is often associated with systemic diseases such as metabolic disorders, anabolic steroid abuse, chronic local steroid injections, long fluoroquinolones, chronic renal failure, SLE, and rheumatoid arthritis. B/L patellar tendon ruptures are extremely uncommon and as per literature, only a few cases reported worldwide. In one published systemic analysis in which they included 32 full-text articles and fourteen studies conducted between 1977 and 2015, only six patients having b/l patellar tendon failure could be identified with none having ESRD with G6pd deficiency [1]. Ours case of B/L patellar tendon rupture associated with ESRD and g6pd deficiency is unique as it is only 1st case as per the literature. Other similar case reported was of 48 years female from Saudi Arabia having isolated ESRD with b/l patellar tendon rupture [2]. Moreover, other reported with ESRD PT with SLE [3]. G6PD deficiency is a genetic disorder that most often affects males. In this disease, there is a defect in the red blood cell (RBC) which carries oxygen from lungs to all tissues. This defect causes RBC to breakdown prematurely leading to hemolytic anemia. Clinical manifestation of this disease is usually paleness, yellowing of skin, shortness of breath, and tachycardia. Musculoskeletal clinical manifestations of G6pd are limited and reported as only fatigue of muscles. Musculoskeletal manifestation of G6pd def is not much studied in the literature. Hence, it needs further research, particularly about any pathological changes at osteotendinous junctions. In chronic renal failure PTs, as kidney function declines, a progressive deterioration in mineral homeostasis occurs resulting in disruption of the balance of normal serum and tissue concentrations of phosphorus, calcium, parathyroid hormone (PTH), and Vitamin D resulting in raised blood level of PTH. It has been proposed that in ESRD PTs this secondary hyperparathyroidism causes increased subperiosteal resorption together with elastosis of connective tissue at the osteotendinous junction favoring tendon avulsion [4]. It is also observed that in ESRD PT on HD, there is an increased blood level of Beta-2 microglobulin which is known as dialysis-related amyloidosis. This beta-2 microglobulin collects at tendon bony junctions resulting in decrease of tendon elasticity and predisposing for easy rupture [5]. Histopathological patterns in the spontaneously ruptured tendons had been studied and most (97%) of the pathological changes were degenerative; they included hypoxic degenerative tendinopathy, mucoid degeneration, tendolipomatosis, and calcifying tendinopathy, either alone or in combination [6-14].
B/L Acute patellar tendon avulsion is rare most ruptures occur at the lower border of patella but can also occur at mid substance or closer to its insertion on tibial tuberosity. Plain X-ray can reveal high-riding patella (patella alta). Apart from X-rays’ ultrasound is also useful and MRI is gold standard as it detects any other important soft tissue structures like anterior cruciate ligament tear and meniscus injury. Surgery is the mainstay and should not be delayed early repair has a satisfactory outcome.
Since B/L tendon rupture is extremely rare therefore there is always a high chance of missing the diagnosis due to the lack of other normal knee for comparison. There should be a high degree of suspicion of B/L patellar tendon avulsion if any patient comes with B/L knee swelling in A/E and there are associated comorbidities such as G6pd def and ESRD.
References
- 1.Camarda L, D’Arienzo A, Morello S, Guarneri M, Balistreri F, D’Arienzoa M. Bilateral ruptures of the extensor mechanism of the knee: A systematic review. J Orthop 2017;14:445-53. [Google Scholar]
- 2.Aloraini LA, Dahduli OS, Alfarhan AM, Alshehri YA, Alsaqry AS. Unique presentation of bilateral patellar tendon rupture in a patient with renal failure: A case report. J Orthop Trauma Surg Relat Res 2018;3(2)5-8. [Google Scholar]
- 3.Tseng HS, Shih HW, Wu CC, Shen HC. Rare case of bilateral patellar tendon rupture in a patient of systemic lupus erythematosus with chronic renal failure. J Med Sci 2020;40:292-5. [Google Scholar]
- 4.De Franco P, Varghese J, Brown WW, Bastani B. Secondary hyperparathyroidism, and not beta 2-microglobulin amyloid, as a cause of spontaneous tendon rupture in patients on chronic hemodialysis. Am J Kidney Dis 1994;24:951-5. [Google Scholar]
- 5.Masonis JL, Frick SL. Bilateral quadriceps tendon rupture as the initial presentation of amyloidosis. Orthopaedics 2001;24:995-6. [Google Scholar]
- 6.Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am 1991;73:1507-25. [Google Scholar]
- 7.Malta LM, Gameiro VS, Sampaio EA, Gouveia ME, Lugon JR. Quadriceps tendon rupture in maintenance haemodialysis patients: Results of surgical treatment and analysis of risk factors. Injury 2014;45:1970-3. [Google Scholar]
- 8.Hannon RJ. Bilateral patellar tendon rupture. Ulster Med J 1990;59:82-3. [Google Scholar]
- 9.Provelegios S, Markakis P, Cambouroglou G. Bilateral, spontaneous and simultaneous rupture of the quadriceps tendon in chronic renal failure and secondary hyperparathyroidism. Report of five cases. Arch Anat Cytol Pathol 1991;39:228-32. [Google Scholar]
- 10.10. Kara A, Sari S, Seker A, Ozturk I. Osteotendinous repair of bilateral spontaneous quadriceps tendon ruptures with the Krackow technique in two patients with chronic renal failure. Acta Orthop Traumatol Turc 2013;47:68-71. [Google Scholar]
- 11.Goldstein ZH, Yi PH, Haughom BD. Bilateral extensor mechanism disruption after total knee arthroplasty in two morbidly obese patients. Orthopedics 2015;38:e443-6. [Google Scholar]
- 12.Seng C, Lim YJ, Pang HN. Spontaneous disruption of the bilateral knee extensor mechanism: A report of two cases. J Orthop Surg 2015;23:262-6. [Google Scholar]
- 13.Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am 1991;73:1507-25. [Google Scholar]
- 14.Jones N, Kjellstrand CM. Spontaneous tendon ruptures in patients on chronic dialysis. Am J Kidney Dis 1996;28:861-6. [Google Scholar]








