A differential diagnosis of tophaceous gout in the knee should be considered in patients presenting with a painful, stiff knee joint accompanied by synovial hypertrophy upon examination.
Dr. Hitarth Gathani, Department of Orthopaedics, Grant Government Medical College and Sir J J Group of Hospitals, Byculla, Mumbai, Maharashtra, India. E-mail: hitarthjgathani@gmail.com
Introduction: Isolated tophaceous gout of the knee is an uncommon presentation, requiring a high degree of clinical suspicion for accurate diagnosis. With prompt and appropriate management, favorable patient outcomes can often be achieved.
Case Report: We present the case of a 32-year-old male clerk with a 2-year history of chronic knee pain and stiffness. Magnetic resonance imaging revealed joint effusion and synovial hypertrophy. Arthroscopic evaluation identified chalky intra-articular deposits confirming isolated tophaceous gout of knee, and histopathological analysis confirmed gross inflammatory synovial hypertrophy. Surgical debridement and synovectomy, followed by medical management, gave good clinical outcomes.
Conclusion: The treating surgeon should recognize this presentation and choose appropriate arthroscopic and medical management, which can lead to favorable outcomes.
Keywords: Knee, arthroscopy, tophaceous, gout, synovial hypertrophy.
Gout is a type of inflammatory arthritis triggered by the crystallization of uric acid within the joints and is often associated with hyperuricemia [1]. Acute gouty arthritis typically presents with the sudden onset of a painful, erythematous, and swollen joint. In contrast, tophaceous gout is a chronic form characterized by the deposition of monosodium urate crystals in the joints and soft tissues, leading to the formation of tophi. This chronic condition typically occurs in patients with a long history of hyperuricemia and recurrent gouty attacks [1]. These tophi can cause significant joint damage, deformities, and functional impairment. Tophaceous deposits may be found in the subcutaneous tissues and the various joints, particularly the first metatarsophalangeal joint, the hand, wrist, or elbow. Tophaceous deposition has been reported in various locations such as finger pads, sacroiliac joint, carpal tunnel, ankle, shoulder, dorsum of the feet, multiple subcutaneous nodules, and axial skeleton [2]. However, isolated tophaceous gout of the knee is relatively rare, with few cases reported in the literature [3]. It is common, however, for the initial diagnosis to be made as an unexpected finding during routine knee arthroscopy, indicated for the treatment of a presumed meniscal or articular cartilage injury or disorder [4]. The management of chronic gout primarily involves medical therapy; however, cases with significant tophus formation often require arthroscopic debridement. This intervention effectively alleviates mechanical symptoms and reduces the risk of acute gout flares by removing the tophi [5]. In this case, we present a 32-year-old male with intra-articular tophaceous gout of the knee, which was managed with arthroscopic debridement and an additional synovectomy due to the presence of gross synovial hypertrophy. This case highlights the importance of considering gout in the differential diagnosis of chronic monoarticular arthritis and demonstrates the effectiveness of combined surgical and medical management in treating advanced cases of tophaceous gout affecting the knee.
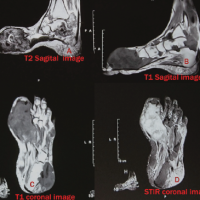
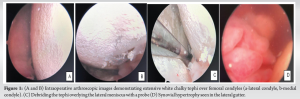
A 32-year-old male presented with chronic left knee pain for 2 years, which had exacerbated in the past 3 months. Along with the pain, the patient experienced stiffness and locking of the knee. On examination, the patient had mild effusion with palpable synovium suggestive of synovial hypertrophy. The knee was stable without laxity in the coronal and sagittal planes, with a range of motion from 0 to 120° which was painful. No other joints were involved and had no palpable gouty lesion over the body. Results of tests for anti-cyclic citrullinated peptide antibodies, rheumatoid factor, and other antibody markers of collagen disease-induced arthritis were all negative. Routine investigations, including radiographs of the knee and an magnetic resonance imaging (MRI), were conducted. The MRI was suggestive of a mucoid anterior cruciate ligament (ACL) and effusion and altered signal over the menisci. Due to the chronicity of the symptoms, the patient was taken up for a diagnostic arthroscopy along with arthroscopic synovectomy. The arthroscopic examination revealed widespread chalky deposits over the cartilage, meniscus, and synovium (Fig. 1a, b, c, d). The synovial fluid was turbid, and there was gross synovial hypertrophy (Fig. 2). Based on the arthroscopic findings, a provisional diagnosis of tophaceous gout was made. Samples of the synovium and synovial fluid were collected for histopathological analysis. The decision was made to proceed with synovectomy and debridement of the urate crystals. Synovectomy was done using an arthroscopic shaver. Debridement was performed with an arthroscopic probe and liberator to erode the tophaceous deposits over the meniscus and cartilage, and the loose bodies then taken out with an arthroscopic grasper. No gross cartilage defects were observed after the debridement. Intra-articular corticosteroid injection was given after the procedure.
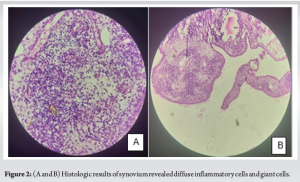
The histopathology of the synovium was suggestive of inflammatory giant cells. Postoperatively, pain and knee extension restriction were dramatically alleviated, and early full weight-bearing was allowed. Post-operative serum uric acid levels were found to be elevated (10.5 mg/dL), and the patient was started on medical management with febuxostat for 3 months [5]. Over 1 month, the symptoms gradually disappeared, and the patient could resume all his daily activities. On further follow-up, the patient was symptom free up to 12 months.
Isolated tophaceous gout of the knee is a rare occurrence, with only a few documented cases in the literature [6,7]. This case highlights the importance of considering gout in the differential diagnosis of chronic knee pain with effusion and synovial hypertrophy, as well as the effectiveness of combined surgical and medical management in treating tophaceous gout. In this case, the radiographic and MRI findings were not particularly informative, as the imaging studies did not provide useful insights for diagnosis. Ko et al. showed that MRI findings of gouty tophi can be non-specific but can have low intermediate signal intensities on T1-weighted images and low intermediate heterogeneous signal intensities on the T2-weighted images [8]. In our case, the MRI was suggestive of a Mucoid ACL, Effusion, intermediate signal over the meniscus, and synovial hypertrophy. Chen et al. showed that such tophaceous deposits present as masses on MRI images with low to intermediate signal intensity on both T1- and T2-weighted images and a characteristic enhancement pattern following intravenous Gd administration [9]. Further management of the case was done with an diagnostic round of arthroscopy followed by arthroscopic synovectomy. According to previous reports, when gouty deposits generally occur on intercondylar notch, suprapatellar bursa, infrapatellar fat pad, lateral and medical gutter, and tibial plateau which was consistent with our findings. We eventually reached a definitive diagnosis based on our arthroscopic findings and the histology of the intraoperative specimens. According to previous case reports, treatment of intra-articular tophaceous gout has been with non-operative and operative management. Chatterjee and Ilaslan reported one case in which the pain was successfully treated with allopurinol therapy alone for 3 months, without arthroscopic surgery [10]. In contrast, Espejo-Baena et al. treated gouty tophi on the surface of the meniscus with arthroscopic resection [11]. Li et al. reported a rare case of intra-articular gouty tophi that resulted in misdiagnosis for 8 years on the basis of the clinical picture and MRI appearance. They stated that a case of gouty tophi is a “great mimic,” given its ability to resemble multiple conditions, although they suggested that persistent mechanical symptoms might be an indication for arthroscopic treatment [12]. Aoki et al. managed an intrameniscal tophi and synovial hypertrophy with partial meniscectomy and synovial hypertrophy in a patient which was previously given antiuremic medication for 4 months [6]. Steinmetz et al. went for arthroscopic surgical debridement with an arthroscopic liberator [13]. In our case, we could not reach any definitive diagnosis preoperatively; hence, we opted for an diagnostic arthroscopy with removal of tophi and synovectomy. After confirming the diagnosis of tophaceous gout by intraoperative findings, histopathology and post-operative serum uric acid levels we started with anti-uremic drugs according at American college of Rheumatology guidelines [5], following which the symptoms and the range of motion of the patient dramatically improved with physiotherapy.
Isolated tophaceous gout of the knee is an uncommon presentation, often requiring a high index of suspicion for accurate diagnosis. This case highlights the importance of considering gout in the differential diagnosis of chronic monoarticular arthritis, especially when associated with synovial hypertrophy. Arthroscopic synovectomy and debridement, combined with targeted medical management, can yield favorable outcomes, significantly improving symptoms and joint function. Early recognition and comprehensive treatment are essential to prevent further joint damage and restore the patient’s quality of life.
Surgical and medical management both have favorable results in cases of tophaceous gout of the knee.
References
- 1.Choi HK, Mount DB, Reginato AM, American College of Physicians, American Physiological Society. Pathogenesis of gout. Ann Intern Med 2005;143:499-516. [Google Scholar | PubMed]
- 2.Ozkan FU, Bilsel K, Turkmen I, Erdil M, Soylemez S, Ozkan K. Tophi gout around the knee joint: An unusual presentation with a soft tissue mass. Int J Case Rep Images 2013;4:593. [Google Scholar | PubMed]
- 3.Weaver AL. Epidemiology of gout. Cleveland Clinic J Med 2008;75 Suppl 5:S9-12. [Google Scholar | PubMed]
- 4.Hussin P, Mawardi M, Nizlan NM. The ‘Chalky Culprit’ of acute locked knee. G Chir 2014;35:239-40. [Google Scholar | PubMed]
- 5.Brook RA, Forsythe A, Smeeding JE, Lawrence Edwards N. Chronic gout: Epidemiology, disease progression, treatment and disease burden. Curr Med Res Opin 2010;26:2813-21. [Google Scholar | PubMed]
- 6.FitzGerald JD, Dalbeth N, Mikuls T, Brignardello-Petersen R, Guyatt G, Abeles AM, et al. 2020 American college of rheumatology guideline for the management of gout. Arthrit Care Res ((Hoboken) 2020;72:744-60. [Google Scholar | PubMed]
- 7.Aoki T, Tensho K, Shimodaira H, Akaoka Y, Takanashi S, Shimojo H, et al. Intrameniscal gouty tophi in the knee: A case report. JBJS Case Connect 2015;5:e74. [Google Scholar | PubMed]
- 8.Ko KH, Hsu YC, Lee HS, Lee CH, Huang GS. Tophaceous gout of the knee: Revisiting MRI patterns in 30 patients. J Clin Rheumatol 2010;16:209-14. [Google Scholar | PubMed]
- 9.Chen CK, Yeh LR, Pan HB, Yang CF, Lu YC, Wang JS, et al. Intra-articular gouty tophi of the knee: CT and MR imaging in 12 patients. Skeletal Radiol 1999;28:75-80. [Google Scholar | PubMed]
- 10.Chatterjee S, Ilaslan H. Painful knee locking caused by gouty tophi successfully treated with allopurinol. Nature clinical practice. Rheumatology 2008;4:675-9. [Google Scholar | PubMed]
- 11.Espejo-Baena A, Coretti SM, Fernandez JM, Garcia-Herrera JM, Del Pino JR. Knee locking due to a single gouty tophus. J Rheumatol 2006;33:193-5. [Google Scholar | PubMed]
- 12.Li TJ, Lue KH, Lin ZI, Lu KH. Arthroscopic treatment for gouty tophi mimicking an intra-articular synovial tumor of the knee. Arthroscopy 2006;22:910.e1-3. [Google Scholar | PubMed]
- 13.Steinmetz RG, Maxted M, Rowles D. Arthroscopic management of intra articular tophaceous gout of the knee: A case report and review of the literature. J Orthop Case Rep 2018;8:86-9. [Google Scholar | PubMed]