Tricortical iliac crest graft used to reconstruct the distal tibia in a case of Aneurysmal Bone Cyst with extension into the joint could be a reliable and cost-effective alternative to ankle joint fusion, especially in young patients.
Dr. Shaswat Mishra, Department of Orthopaedics, Grant Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India. E-mail: shaswatmishra1994@gmail.com
Introduction: Aneurysmal bone cysts (ABC) are known to be largely limited to the metaphysis. Epiphyseal extension of the lesion that too in a skeletally mature patient, has rarely been reported. Further, literature regarding the management of these lesions, where sclerotherapy failed, is scarce. We describe a case of distal tibia ABC with intra-articular extension, managed with curettage and iliac crest allograft auto-graft block reconstruction of the joint with excellent functional outcome.
Case Report: The authors report a case of a 20-year-old lady presenting with swelling and pain in her ankle joint. X-rays and magnetic resonance imaging showed an ABC in the distal tibia with extension to the joint. Biopsy confirmed the diagnosis which was followed by sclerotherapy, but the lesion recurred in a year. Surgery in the form of excision, curettage, and joint reconstruction using tricortical iliac crest bone autograft block was done which was fixed with plate osteosynthesis.
Result and Discussion: The patient under follow-up at 3 years shows excellent clinical outcome, no evidence of recurrence, able to perform out carry out her personal and professional activities with no restrictions. Addressing such a case is a difficult task, and in a financially constrained patient scenario such as ours, brings its own set of challenges. Such cases of joint involvement in ABCs are very rare, and literature on the management of such lesions is even more scarce. Therefore, they need reporting to help formulating better treatment protocols in such difficult scenarios.
Conclusion: The reconstructive of the ankle joint with tricortical iliac crest bone grafting in ABC of distal tibia with joint involvement can provide excellent clinical and radiological outcomes.
Keywords: Aneurysmal bone cyst, intra-articular extension, ankle joint reconstruction, iliac crest tri-cortical bone graft, joint preservation.
Aneurysmal bone cysts (ABCs) are benign, aggressive bone tumors that frequently develop in the metaphysis of long bones, particularly the femur (6.9%), tibia (10.5%), and humerus (7%), as well as the posterior elements of the spine (3.5%) [1,2]. These tumors are more prevalent in the 1st 2 decades of life, before skeletal maturation [1]. ABCs can exist as primary lesions (approximately 70% of cases) or as secondary bone lesions (about 30% of cases), depending on whether a pre-existing osseous lesion can be identified [3]. Theories on the pathophysiology of ABCs range from genetically pre-disposed bone malignancies to post-traumatic, reactive vascular malformations. ABCs have been compared to “blood-filled sponges” due to their composition of blood-filled, anastomosing cavernomatous areas separated by cyst-like walls made of large cells resembling osteoclasts, fibroblasts, myofibroblasts, osteoid, and woven bone. A distinctive reticulated, lacy, chondroid-like substance, sometimes referred to as a calcified matrix with a chondroid aura, is observed in approximately one-third of cases [4]. The most frequently acknowledged pathogenetic process for ABCs involves a local circulatory disturbance causing a considerable rise in venous pressure and the development of a dilated and expanded vascular bed within the affected bone region. However, recent identification of recurring chromosomal abnormalities has cast doubt on this conventional wisdom [1,4]. Although ABCs most frequently affect the metaphysis, expansion into the epiphysis is possible due to the condition’s locally aggressive nature, which can cause pre-mature closure of the growth plate and result in deformity [5]. Primary epiphyseal ABC, however, is a very rare condition, especially in skeletally mature individuals [6].
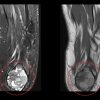
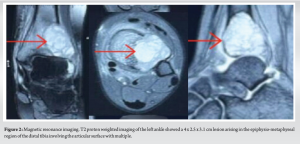
A 20-year-old female patient presented to our outpatient department with complaints of pain and progressive swelling around her left ankle over the preceding 8 months. She had no history of trauma, fever, or constitutional symptoms, and no systemic involvement. On presentation, she had a 4 x 3 cm swelling over the anterior aspect of the ankle, which was firm in consistency, tender, and had crackling on pressure. The range of motion was essentially unhindered but painful at the extremes of movement and weight-bearing. There was no evidence of inflammation or infection on the overlying skin and no neurovascular deficit. Upon presentation, the American Foot and Ankle Score was 67 [6]. Plain radiographs (Fig. 1) revealed an eccentric expansile lytic lesion in the epiphysio-metaphyseal region of the distal tibia. The lesion involved the lateral aspect of the distal tibia; the margins were not clearly demarcated. However, the fibula, medial malleolar region, rest of the tibia, and talus appeared normal. Magnetic resonance imaging (MRI) of the ankle joint (Fig. 2) revealed an expansile, eccentric lesion (4 x 2.5 x 3.1 cm) arising in the epiphysio-metaphyseal region of the distal tibia, involving the articular surface with multiple septations and blood-fluid levels, and cortical break involving the inferior and lateral aspects of the distal tibia, with expansion into the soft tissues. A provisional diagnosis of ABC was made based on MRI reporting. Histopathological examination, performed through computed tomography (CT)-guided biopsy, confirmed the diagnosis of ABC.

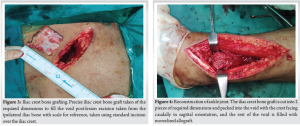
Sclerotherapy was initially chosen as the treatment modality, but the lesion recurred at the 1-year follow-up. Subsequently, a decision was made to opt for operative management. Feeding arteries to the ABC, namely the anterior tibial artery, posterior tibial artery, and peroneal artery were embolized by the Interventional Radiology team 1 day before surgery to minimize intraoperative blood loss [7]. Surgical intervention was planned in the form of curettage and reconstruction. The tumor was exposed through an anterolateral approach and separated from the bed of normal tissue through meticulous dissection. The walls of the lesion were curetted. For reconstruction of the ankle joint, a combination of autograft and allograft was used. Ipsilateral side iliac crest bone graft (Fig. 3) was harvested to reconstruct the gap left after excision. 2 block grafts measuring 4 x 3 x 1.5 cm were finessed to match the contour of the defect, aligned anteroposteriorly and upside down (Fig. 4). Drill holes were made on the tables of the iliac crest and were opposed to each other, and the graft was placed in a position where the crest was facing the articular surface. The rest of the void was filled with morselized allograft and the joint stabilized with 7-hole titanium distal tibia anterolateral plate osteosynthesis (Fig. 5). Homeostasis was achieved and the wound closed in layers.
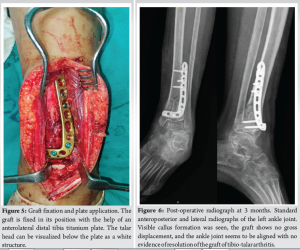

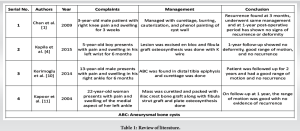
Ankle range of motion exercises were initiated from post-operative day 1. Toe touch weight bearing was started at 8 weeks and full weight bearing at 3 months (Fig. 6). The Patient is now under follow-up for 3 years (Fig. 7) with good clinical results (Fig. 8), no evidence of recurrence and resumption of her personal and professional activities, and had an American Foot and Ankle Score of 93 at final follow-up. The National Library of Medicine of the Institutes of Health’s PubMed search engine (http://www.ncbi.nlm.nih.gov/pubmed) was used to conduct a thorough literature search. The following keyword combinations were used: “Aneurysmal bone cyst,” “ABC,” “Epiphysis,” and “Distal tibia.” The search was restricted to articles in English with no date restrictions (Table 1).
Although Jaffe and Leichstein initially characterized it in 1942, the actual etiology of ABCs remains a mystery [8]. ABCs are unique among osseous tumors in that their name is derived from radiographic characteristics rather than histologic characteristics. However, this is misleading, as the histologic appearance of an ABC is neither similar to that of an aneurysm nor that of a cyst [9]. Radiographically, ABCs appear as subperiosteal, metaphyseal eccentric lesions with elevation and inflation of the periosteum and gradual erosion of the cortex in long bones. CT or MRI is the best way to evaluate ABCs, revealing noticeable thinning of the cortex over the lesion with only minor periosteal reaction [10]. ABC extending into the epiphysis are extremely rare; we found only three such case reports in the literature, involving the distal ulna [4], proximal tibia [1], and distal tibia [10]. Notably, all these cases involved skeletally immature patients, whereas our case involved a skeletally mature individual. Recent studies suggest that some ABCs may harbor specific chromosomal abnormalities, most frequently translocations. There have also been reports of malignant transformation into osteosarcoma. One study demonstrated that somatic mutations influence ABC formation and identified genes on bands 16q22 and 17p13 as potentially crucial to this process. Furthermore, this translocation can be considered pathognomonic for ABC [11]. Campanna classified these tumors based on their radiographic appearance [12]. Dabska and Buraczewski initially described the histopathology of ABCs as cavernous vascular tumors with intralesional communication cavitations but no blood clots. Microscopic examination of ABCs often reveals hemorrhagic tissue with cavitary gaps divided by fibrous septa, comprising mostly spindle cells, inflammatory cells, and a limited number of giant cells. Osteoid development with or without osteoblastic rimming may also be observed [13]. Curettage with bone grafting has been the mainstay for the treatment of ABCs for a long. Bone cement polymethylmethacrylate has shown promising results in preventing recurrence [14]. Sclerotherapy has also shown promising results in many literatures [15]. There have been reports of unsuccessful treatments that involved puncturing the bone wall with cannulated needles and injecting methylprednisolone acetate into the cyst [16]. Radiation therapy was effective in causing cyst ossification, but there is a chance that it will also cause sarcoma, growth arrest, and limb-length discrepancy. This process has now been nullified [17]. Lesions that are not active can just be observed and not treated. Sometimes, these lesions respond to only a curettage and resolve without recurring [17]. All methods described in the literature are pertinent to metaphyseal lesions, which have no joint involvement. The patient described in our report had a lesion of the distal tibia epiphysio-metaphyseal junction, and since the tumor had breached and eroded the articular surface, the conventional methods described above would not have done justice, since it was a weight-bearing joint and would have caused further complications. For this reason, we had to improvise and come out with this novel approach of using the tricortical iliac crest autograft with morselized allograft, augmented with a plate, which salvaged the joint function of this young lady and also provided a good functional outcome. This novel technique of using a tricortical iliac crest graft shows a promising prospect in preserving joint function in benign tumors with intra-articular extensions, in financially constrained patient scenarios where arthroplasty is not feasible. However, being a one-off case, this needs further validation with case series of similar nature.
Heeding to the extensive research of our authors, this is the only case of epiphyseal extension of an ABC in a skeletally mature patient with tibio-talar joint destruction. This was successfully managed with curettage and reconstruction with Iliac Crest Autograft and morselized allograft with plate osteosynthesis. The main highlight was preserving the joint function in a financially constrained set-up, where arthroplasty wasn’t an option. This technique proved to be cost-effective and provided excellent long-term results.
This case emphasizes the importance of considering a tricortical iliac crest graft to reconstruct ankle mortise in lesions of the distal tibia affecting the joint. Our described technique shows a reliable and cost-effective way of addressing these challenging scenarios, offering a practical alternative to ankle joint fusion and should be considered especially in young patients.
References
- 1.Chan G, Arkader A, Kleposki R, Dormans JP. Case report: Primary aneurysmal bone cyst of the epiphysis. Clin Orthop Relat Res 2010;468:1168-72. [Google Scholar | PubMed]
- 2.Mendenhall WM, Zlotecki RA, Gibbs CP, Reith JD, Scarborough MT, Mendenhall NP. Aneurysmal bone cyst. Am J Clin Oncol 2006;29:311-5. [Google Scholar | PubMed]
- 3.Cottalorda J, Bourelle S. Modern concepts of primary aneurysmal bone cyst. Arch Orthop Trauma Surg 2007;127:105-14. [Google Scholar | PubMed]
- 4.Kapila R, Sharma R, Sohal YS, Singh D, Singh S. Primary epiphyseal aneurysmal bone cyst of distal ulna. J Orthop Case Rep 2015;5:85-7. [Google Scholar | PubMed]
- 5.Parvizi J. High Yield Orthopaedics E-Book. Netherlands: Elsevier Health Sciences; 2010. [Google Scholar | PubMed]
- 6.Mani SB, Brown HC, Nair P, Chen L, Do HT, Lyman S, et al. Validation of the Foot and Ankle Outcome Score in adult acquired flatfoot deformity. Foot Ankle Int 2013;34:1140-6. [Google Scholar | PubMed]
- 7.Green JA, Bellemore MC, Marsden FW. Embolization in the treatment of aneurysmal bone cysts. J Pediatr Orthop 1997;17:440-3. [Google Scholar | PubMed]
- 8.Mohaidat ZM, Al-Gharaibeh SR, Aljararhih ON, Nusairat MT, Al-Omari AA. Challenges in the diagnosis and treatment of aneurysmal bone cyst in patients with unusual features. Adv Orthop 2019;2019:2905671. [Google Scholar | PubMed]
- 9.Goss LR, Walter JH. Pediatric aneurysmal bone cyst of the distal tibia. J Am Podiatr Med Assoc 1997;87:136-40. [Google Scholar | PubMed]
- 10.Kerimoglu S, Çitlak A, Kerimoglu G, Turgutalp H. Primary aneurysmal bone cyst of the distal tibial epiphysis: A case report. J Pediatr Orthop B 2014;23:266-9. [Google Scholar | PubMed]
- 11.Kapoor H, Singh D, Bhatia N, Chaudhary D, Singh AK. Distal tibial aneurysmal bone cyst treatment by using a proximal fibular autologous bone graft: A case report. J Foot Ankle Surg 2004;43:179-84. [Google Scholar | PubMed]
- 12.Campanacci M, Capanna R, Picci P. Unicameral and aneurysmal bone cysts. Clin Orthop Relat Res 1986;204:25-36. [Google Scholar | PubMed]
- 13.Dabska M, Buraczewski J. Aneurysmal bone cyst. Pathology, clinical course and radiologic appearances. Cancer 1969;23:371-89. [Google Scholar | PubMed]
- 14.Marcove RC, Sheth DS, Takemoto S, Healey JH. The treatment of aneurysmal bone cyst. Clin Orthop Relat Res 1995;311:157-63. [Google Scholar | PubMed]
- 15.Dubois J, Chigot V, Grimard G, Isler M, Garel L. Sclerotherapy in aneurysmal bone cysts in children: A review of 17 cases. Pediatr Radiol 2003;33:365-72. [Google Scholar | PubMed]
- 16.Scaglietti O, Marchetti PG, Bartolozzi P. Final results obtained in the treatment of bone cysts with methylprednisolone acetate (depo-medrol) and a discussion of results achieved in other bone lesions. Clin Orthop Relat Res 1982;165:33-42. [Google Scholar | PubMed]
- 17.Clough JR, Price CH. Aneurysmal bone cyst: Pathogenesis and long term results of treatment. Clin Orthop Relat Res 1973;97:52-63. [Google Scholar | PubMed]