We underline the importance of hybrid external fixation in articular fractures with vascular com-promise.
Dr. Mariangela Di Già, Department of Traumatology and General Orthopedics, Careggi University Hospital, Florence, 50100, Italy. E-mail: mariangela.digia@gmail.com
Introduction: Coral reef aorta (CRA) is a calcifying stenotic disease of the distal aorta that can result in hypoperfusion and thromboembolic episodes of both internal organs and lower limbs. Only case reports of this extremely rare condition are described in the literature. Our report is the first article about fracture management and healing in this anomaly.
Case Report: A 58-year-old woman with an alcohol abuse story presented to our emergency de-partment after a fall from height. She reported a 43-C3 Gustilo I open leg fracture treated in an emergency with a damage control orthopedic approach. As an incidental finding, a CRA anomaly was found during an abdomen computer tomography scan. Considering the fracture pattern and the patient factors, hybrid external fixation was chosen as the definitive treatment. Complete bone healing and a good functional recovery 4 months after surgery were assessed.
Conclusion: External fixation and percutaneous techniques must be considered in complex articu-lar fractures with vascular compromise. A minimally invasive approach with early motion and weight bearing allowed for a complete fracture healing without deficits or additional soft tissue damage.
Keywords: Distal tibial plafond fractures, pilon fractures, coral reef aorta, vascular stenosis, hy-brid external fixation.
Coral reef aorta (CRA) is a rare calcifying stenotic disease of the juxta and suprarenal aorta that may cause luminal obstruction of the vessel. Qvarfordt et al. first identified this rare condition in 1984 as an “eccentric, heavily calcified polypoid lesion originating from the posterior surface of the suprarenal aorta” [1].The etiology of this condition is still uncertain: the calcification of a fibrin-platelet thrombus at the site of an initial injury to the aortic endothelium may result in this lesion. In literature, these internally irregular protruding calcifications are described, such as hyperplastic bone without serum calcium anomalies [2]. Only case reports exist, except for a series of more than 80 patients collected by Sagban et al. [3]. Clinically patients may present with visceral ischemia, renovascular hypertension, visceral compromise, or arterial insufficiency of the lower extremities, depending on the segment of the aorta involved. The current mainstay of treatment for extensive lesions in hemodynamically significant symptomatic patients is operative, typically involving transaortic endarterectomy [4]. Endovascular and laparoscopic surgical interventions are described in the literature for the elderly or patients with multiple comorbidities [4,5]. There is no literature about fracture healing in CRA-patients. Our case is the first described report.
Presenting concerns
A 58-year-old female patient presented to our emergency department after a fall from height due to alcohol abuse.
The woman fell from 10 m onto the ground.
She was airlifted to our hospital.
Clinical findings
At presentation, the patient was hemodynamically stable with Glasgow Coma Scale 15 and retrograde post-traumatic amnesia. She had a history of alcoholism and smoking.
The orthopedic assessment in the emergency room showed a clear deformity of the left distal leg with a Gustilo I grade exposure. No clinical evidence of dorsalis pedis and posterior tibial pulses in a warm rose foot. After a close reduction procedure, there was no evidence of pulse recovery. The neurologic and sensory examination was not evaluable (an ultrasound-guided antalgic femoral block was performed in the emergency room before an orthopedic evaluation). A proper antibiotic prophylaxis was administered (Piperacillin/Tazobactam).
Diagnostic focus and assessment
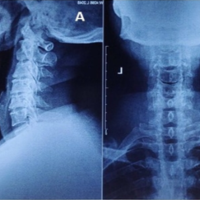
The total-body computer tomography (CT) performed in emergency showed left pulmonary contusion and pleural effusion, VI-XI left rib fractures and a millimetric basal left pneumothorax on the thoracic scans. The abdomen was suggestive for the incidental finding of an atheromatous calcific sub-occlusive stenosis (90%) of the thoracoabdominal aorta with severe involvement of the right renal artery, the celiac trunk, and the superior mesenteric artery (Fig. 1, 2).

The patient was evaluated by a multidisciplinary trauma team.
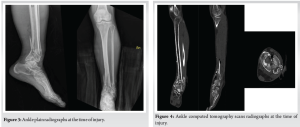
The X-ray and CT of the left leg and ankle showed a comminuted tibial plafond fracture with an associated comminuted fracture of the distal fibula that was classified as 43-C3 according to the AO Foundation (AO)/ fracture classification system [6]. The patient was evaluated by the vascular surgeon who performed both venous and arterial eco-color doppler of the inferior limbs with evidence of good blood-perfusion, high risk of vascular complications, and no indication to emergency surgery. The urologist suggested a wait-and-see approach with clinical monitoring and a 24-h CT control to evaluate the renal ischemia.
Timeline
The day of injury was April 05, 2022.
The patient had initial provisional external fixation in an emergency with irrigation of the fracture wound and sterile dressing. Appropriate antibiotic prophylaxis was started in the Emergency Department. A joint-bridging triangular construct was made. The patient returned to surgery on April 21, 2022. A definitive conversion into hybrid external fixation was performed. The temporary triangular frame was removed and a percutaneous approach to the distal tibia was performed. Under fluoroscopic check, the articular surface of the distal tibia was reduced and fixed with two cannulated screws. A percutaneous wiring of the fibula, to restore axis, length, and rotation, was then made. At last, a hybrid external fixator was applied. A single distal ring was connected to four wires to reduce and fix the tibial surface and an olive wire was applied to restore the normal syndesmotic space. Three 6 mm hydroxyapatite-coated pins were used to connect the ex-fix body to the distal ring and an additional 3 mm pin was added on the first metatarsal base. On May 27, 2022, the first metatarsal pin was removed. The patient started a partial weight bearing on the left leg and the active ankle mobilization. Three months after the definitive external fixation surgery, the patient was advanced to weight-bearing as tolerated gait. The clinical assessment showed no peripheral neurovascular injuries and a complete distal range of motion. The final follow-up in August 2022 showed complete bone healing with an indication to external fixator removal. It was performed on August 25, 2022. The patient had no pain, no deficit, and a complete return to normal independent activities.
Therapeutic focus and assessment
Plain radiographs and CT scans were obtained at the time of injury (Fig. 3, 4). Radiographic images were obtained during both emergency and definitive external fixator applications (Fig. 5, 6). Intraoperative fluoroscopy was used during the surgical procedures.

Plain X-rays were used during follow-up visits to assess fracture healing.
Follow-up and outcomes
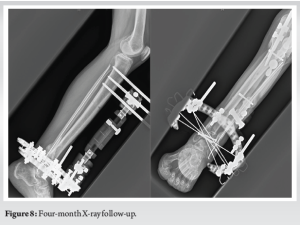
The patient follow-up lasted approximately 4 months after the definitive treatment: Three months after definitive external fixation the fractures appeared nearly consolidated on plain radiographs and complete weight-bearing was allowed (Fig. 7).
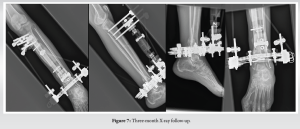
Four months after surgery (Fig. 8), the patient removed the external fixator with evidence of complete healing.
The management of articular distal tibial fractures is a challenge. The articular involvement and the poor functional outcomes after conservative treatment or external fixation required the AO at the beginning of 1960 to develop some guidelines for the operative treatment of those lesions. This gold standard treatment was open reduction and rigid internal fixation. As described by Babis et al. [7] the outcome of surgical management of tibial pilon fracture is affected by the clinical type of the fracture, the quality of reduction achieved at surgery, and the specific surgical procedure. Soft tissue status and recovery have an important role in distal tibial fracture healing especially in high-energy trauma lesions. High-energy pilon injuries resulted in a high incidence of complication rates such as skin breakage, infection, malunion, non-union, arthrodesis, and even amputations when treated with open reduction and internal fixation [8]. External fixation minimizes soft tissue complications and allows for early joint motion while providing stability even in distal articular fractures [9]. Diabetes, peripheral vascular disease, peripheral neuropathy, poor bone quality, and poor patient compliance are risk factors for wound complications and poor bone healing potential. The patients affected by all those conditions require accurate post-operative wound care, close follow-up and prolonged immobilization when treated with open reduction and internal fixation to minimize possible complications, second surgeries, and amputation [10-14]. External fixation has gained popularity in the past decades to treat ankle fractures associated with high-energy trauma, diabetes, peripheral vascular insufficiency, and neuropathy. A variety of methods and constructs has been proposed with the aim to re-establish anatomic alignment and compression at the fracture sites, minimizing soft tissue damage, immobilization, and weight-bearing restrictions [15]. The AO/ASIF classification of distal tibial fractures [16] distinguishes between extra-articular (type A), partly intra-articular (type B), and complete articular fractures (type C). Subgroups describe the degree of comminution. Ruedi and Allgower [17] suggested a simple distinction between non-displaced fractures (type 1), simple displaced fractures (type 2), and fractures with joint surface comminution, impaction, or both topics (type 3). In AO/ASIF type B/C or Ruedi and Allgower type 3 fractures external fixation combined with limited internal fixation addresses joint reconstruction and axial alignment of the tibia with minimal additional soft tissue damage and dissection. In this scenario, definitive treatment with circular and hybrid external fixators ensure high mechanical stability and consent early motion of foot and ankle minimizing post-surgical stiffness [18,19].
CRA is a rare vascular abnormality that can result in hypoperfusion and thromboembolic episodes of both internal organs and lower limbs. In this complex case, the vascular status was complicated by alcoholism and initial-stage cirrhosis. The concerning general history of this patient and the complex fracture pattern guided our decision to make external fixation the final treatment for this distal tibial fracture. Hybrid external fixation must be considered in articular open fractures, distal tibial fractures with soft tissue damage, and complex patients. In those cases, the canonic open reduction and internal fixation could be risky and detrimental, with higher infection and complication rates. Both early weight bearing and ankle motion were very important factors to be considered in this compromised vascular picture, allowing better circulation of the lower limbs with a lower risk of thromboembolism.
External fixation and percutaneous techniques must be considered in complex articular fractures with vascular compromise. A minimally invasive approach with early motion and weight-bearing allowed for a complete fracture healing without deficits or additional soft tissue damage.
References
- 1.Qvarfordt PG, Reilly LM, Sedwitz MM, Ehrenfeld WK, Stoney RJ. “Coral reef” athero-sclerosis of the suprarenal aorta: Unique clinical entity. J Vasc Surg 1984;1:903-9. [Google Scholar | PubMed]
- 2.Schulte KM, Reiher L, Grabitz L, Sandmann W. Coral reef aorta: A long-term study of 21 patients. Ann Vasc Surg 2000;14:626-33. [Google Scholar | PubMed]
- 3.Sagban AT, Grotemeyer D, Rehbein H, Sandmann W, Duran M, Balzer KM, et al. Occlu-sive aortic disease as coral reef aorta: Experience in 80 cases. Zentralbl Chir 2010;135:438-44. [Google Scholar | PubMed]
- 4.Holfeld J, Gottardi R, Zimpfer D, Dorfmeister M, Dumfarth J, Funovics M, et al. Treat-ment of symptomatic coral reef aorta by endovascular stent-graft placement. Ann Thorac Surg 2008;85:1817-9. [Google Scholar | PubMed]
- 5.Di Centa I, Coggia M, Javerliat I, Alfonsi P, Maury JM, Kitzis M, et al. Total laparoscopic suprarenal aortic coral reef removal. J Vasc Surg 2006;44:194-7. [Google Scholar | PubMed]
- 6.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classi-fication compendium 2018. J Orthop Trauma 2018;32 Suppl 1:S1-170. [Google Scholar | PubMed]
- 7.Babis GC, Vayanos ED, Papaioannou N, Pantazopoulos T. Results of surgical treatment of tibial plafond fractures. Clin Orthop Relat Res 1997;341:99-105. [Google Scholar | PubMed]
- 8.Dillin L, Slabaugh P. Delayed wound healing, infection, and nonunion following open re-duction and internal fixation of tibial plafond fractures. J Trauma 1986;26:1116-9. [Google Scholar | PubMed]
- 9.El-Shazly M, Dalby-Ball J, Burton M, Saleh M. The use of trans-articular and extra-articular external fixation for management of distal tibial intra-articular fractures. Injury 2001;32 Suppl 4:SD99-106. [Google Scholar | PubMed]
- 10.Costigan W, Thordarson DB, Debnath UK. Operative management of ankle fractures in pa-tients with diabetes mellitus. Foot Ankle Int 2007;28:32-7. [Google Scholar | PubMed]
- 11.Jones KB, Maiers-Yelden KA, Marsh JL, Zimmerman MB, Estin M, Saltzman CL. Ankle fractures in patients with diabetes mellitus. J Bone Joint Surg Br 2005;87:489-95. [Google Scholar | PubMed]
- 12.Kristiansen B. Results of surgical treatment of malleolar fractures in patients with diabetes mellitus. Dan Med Bull 1983;30:272-4. [Google Scholar | PubMed]
- 13.McCormack RG, Leith JM. Ankle fractures in diabetics: Complications of surgical man-agement. J Bone Joint Surg Br 1998;80:689-92. [Google Scholar | PubMed]
- 14.Di Domenico LA, Brown D, Zgonis T. The use of Ilizarov technique as a definitive percu-taneous reduction for ankle fractures in patients who have diabetes mellitus and peripheral vascular disease. Clin Podiatr Med Surg 2009;26:141-8. [Google Scholar | PubMed]
- 15.Rammelt S, Endres T, Grass R, Zwipp H. The role of external fixation in acute ankle trau-ma. Foot Ankle Clin 2004;9:455-74, vii-viii. [Google Scholar | PubMed]
- 16.Muller ME, Nazarian S, Koch P, Schatzker J. The Comprehensive Classification of Frac-tures of the Long Bones. Berlin, Germany: Springer Verlag; 1990. [Google Scholar | PubMed]
- 17.Ruedi T, Allgower M. Fractures of the lower end of the tibia into the ankle joint. Injury 1969;1:92-108. [Google Scholar | PubMed]
- 18.Salter RB, Simmonds DF, Malcolm BW, Rumble EJ, MacMichael D, Clements ND. The biological effect of continuous passive motion on the healing of full-thickness defects in articular cartilage. An experimental investigation in the rabbit. J Bone Joint Surg Am 1980;62:1232-51. [Google Scholar | PubMed]
- 19.Galante VN, Vicenti G, Corina G, Mori C, Abate A, Picca G, et al. Hybrid external fixation in the treatment of tibial pilon fractures: A retrospective analysis of 162 fractures. Injury 2016;47 Suppl 4:S131-7. [Google Scholar | PubMed]