This study aimed to explore the challenges associated with managing wound breakdown following radiotherapy
Dr. Tito Brambullo, Department of Neurosciences, Plastic Surgery Unit, University of Padua, via N. Giustiniani 2, 35128, Padua, Italy. E-mail: tito.brambullo@unipd.it
Introduction: Radiodermatitis is a common complication experienced by patients undergoing radiation therapy. Its severity can vary from mild erythema to more serious conditions, including desquamation, ulceration, and, in extreme cases, necrosis. In addition, it is widely acknowledged that radiotherapy (RT) itself carries oncogenic risks, potentially causing cellular mutations that may lead to the development of neoplasms, sometimes years after treatment. Diagnostic and staging tools such as magnetic resonance imaging, computed tomography, and positron emission tomography scans are crucial in these cases, with biopsy serving as the definitive method for histological confirmation. However, large excisions often required in these situations necessitate complex reconstructive procedures and are associated with a high risk of local complications, including wound dehiscence and infection.
Case Report: We present three cases of radiodermatitis that developed following radiation therapy to the shoulder. These cases highlight the need to consider radiodermatitis as a differential diagnosis for skin changes occurring after RT, especially in patients with a history of cancer.
Conclusion: The misdiagnosis or delayed diagnosis of radiodermatitis can substantially increase patient morbidity. Greater awareness of this potential complication underscores the importance of closely monitoring for skin-related issues in patients receiving RT.
Keywords: Anterolateral flap, latissimus dorsi flap, radiotherapy, sarcoma, shoulder.
Presently, the gold standard curative therapy for soft tissue sarcoma and advanced squamous cell carcinoma arising from the shoulder region entails tumor surgery with negative margins; however, the multimodal strategy of combining this approach with perioperative radiotherapy (RT) has demonstrated a reduction in the rate of local recurrence. Positive margins, tumor size exceeding 5 cm, deep tumor locations, and high grades emerged as the most notable factors indicating potential benefits from radiation therapy, particularly in enhancing local control [1]. Previously, external radiation therapy was frequently employed in the treatment of shoulder degenerative arthrosis [2], which is particularly prevalent among hand workers and carpenters. However, in recent years, there have been reports of a growing number of patients who have developed radiation-induced skin cancer several years after being exposed to radiation therapy [3]. While RT is an effective treatment modality, it also carries the risk of complications that have the potential to limit functional abilities and significantly impact on the overall quality of life (QoL) for patients. Undergoing RT, they may experience acute side effects, such as skin reactions and edema [4-6], as well as long-term effects such as fractures or fibrosis. Other complications related to RT include various types of wound issues such as infections, wound dehiscence, hematomas, and seromas, as well as problems with blood vessels such as insufficiency and nerve damage [7]. Approximately, 95% of cancer patients undergoing radiation therapy will experience some degree of radiodermatitis, characterized by symptoms such as erythema, dry desquamation, and moist desquamation [4,6]. Chronic radiodermatitis frequently manifests several months to years after the completion of radiation therapy and can lead to the development of radiation-induced morphea, which is often mistaken for other dermatological conditions or recurrent malignancy due to its atypical appearance [4]. Chronic damage, or chronic radiation-induced fibrosis (RIF), is characterized by the development of skin structural changes that occur months after radiation therapy [4,6]. All the typical features of healthy skin, such as elasticity, pliability, and trophism, are lost, with a progressive substitution of the subcutaneous tissue by dense fibrous tissue. The skin becomes pre-disposed to breakdown and ulcer formation due to permanent ischemia of the subcutaneous layer. Chronic fragility impacts the envelope, which is prone to rupture even for light injuries that are normally well tolerated, and the wound healing process seems delayed or not completely effective [4,8]. Sometimes, local pain and discomfort persist in RIF patients, for whom definite treatment is still to be found. Furthermore, it is widely recognized that RT can have oncogenic properties, causing cellular mutations and potentially triggering the development of neoplasms even several years after treatment [9,10]. The cumulative risk of skin cancer development within the radiation field appears to increase with time. RT appears to be implicated in activating suppressor genes and promoting oncogenes [11]. RT has been proven to be associated with basal cell carcinoma, with an estimated incidence of 2% [12], but there is less evidence for squamous cell carcinoma (SCC) and melanoma [13]. However, cases of SCC arising from a body area that underwent adjuvant RT are well documented in the literature [14-16]. Thus, the pathogenesis of a chronic ulcer arising from a radiation field after years of RT administration may be extremely difficult to determine clinically. This issue may lead to incorrect therapies and overtreatment.
Case #1
An 83-year-old male patient came to our attention in December 2017 due to chronic skin ulceration at the left deltopectoral sulcus developed following RT. He had indeed undergone RT in 1999 after the resection of a left subclavian myxofibrosarcoma, which later recurred, leading to further surgery in 2004 involving the removal of the pectoralis major muscle and partial resection of the deltoid muscle. The patient had been treated with a total dose of 55 Gy of hypofractionated RT. The gadolinium-enhanced magnetic resonance imaging (MRI) performed in February 2018 described a solid nodular formation of 1.5 cm compatible with enchondroma, which orthopedic colleagues advised to monitor with radiographic follow-up. On physical examination, a chronic ulcerated lesion within atrophic and dyschromic skin involving the left upper hemithorax was noted, unresponsive to conservative therapy with advanced dressings. The patient was then subjected to surgical excision en bloc of the entire left upper hemithoracic region where the ulcerated lesion was located, which was sent for histological examination. The repair was carried out using a pedunculated rotation flap of the latissimus dorsi muscle and coverage of the flap with a dermo-epidermal graft taken from the left trochanteric region (Fig. 1).
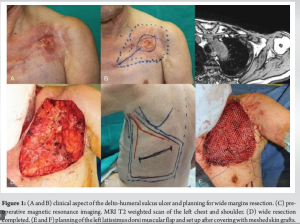
Histological examination did not reveal neoplastic residues, but only dermal alteration consistent with radiodermatitis. The patient has completed the scheduled follow-up and there are currently no signs of tumor relapse. At present, the affected shoulder exhibits mild stiffness; however, the patient has not experienced significant impairment in daily activities or pain, despite a limited abduction of the left upper limb of approximately 100°. Currently, the patient undergoes regular physical therapy, demonstrating gradual improvement in range of motion. This progress indicates that the intervention has facilitated a satisfactory QoL for the patient.
Case #2
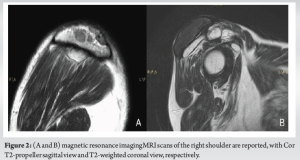
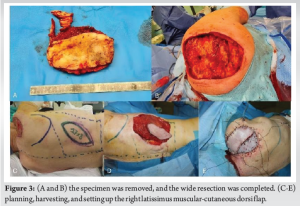
A 70-year-old male patient was admitted to our clinic in August 2023 for the appearance of multiple swellings in the right shoulder following previous removal of a G1 myxoid liposarcoma and then subjected to adjuvant RT in 2003. Furthermore, in this case, the total dose applied was 55 Gy of hypofractionated RT. Physical examination showed skin on the right shoulder with signs of post-actinic dermatitis and several inflammatory-like lesions interposed with non-hyperemic skin. The clinical picture did not appear to be of unequivocal interpretation. Imaging evaluation through gadolinium-enhanced MRI of the right upper extremity performed in April 2023 (Fig. 2) showed a fluid-filled swelling under the right supraglenoid subcutaneous tissue, subsequently subjected to cytological examination with fine needle aspiration and microbiological examination, both resulted inconclusive. The patient underwent a demolition excisional biopsy of the lesion in August 2023 (Fig. 3a and b). The result of the histological examination highlighted skin and subcutis alterations with no tumor relapse. A first reconstructive surgery using a pedicled latissimus dorsi flap was attempted in November 2023 (Fig. 3c, d, e). The apical portion of the flap underwent suffering and necrosis (Fig. 4a), consequently, demolition surgery and application of negative pressure wound therapy with instillation therapy (NPWTi-d) was performed in January 2024. A second microsurgical reconstructive procedure using the anterolateral thigh flap was then performed in February 2024 (Fig. 4b, c, d). The healing process was uneventful, and the patient is currently under clinical follow-up. Currently, the patient has regained only a limited range of motion in the upper limb due to frozen shoulder syndrome that developed following the initial surgical intervention. The patient is currently undergoing orthopedic and physiatrist evaluations to ascertain whether surgical intervention through shock wave therapy, arthroscopic capsular release, or non-invasive manipulation under cervical nerve root block is necessary to enhance mobility.

Case #3
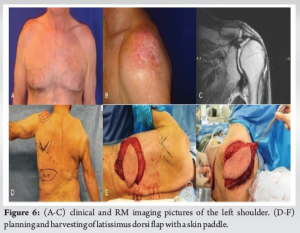
A 78-year-old male was admitted to our clinic in October 2013 for chronic radiodystrophy of both shoulders, which developed after a cycle of RT for degenerative arthrosis that took place 7 years prior. The patient received hypofractionated RT with a total dose of 60 Gy. The patient underwent fat grafting on the right shoulder in February and August 2014, and a diagnostic incisional biopsy was performed. The histological examination revealed dermal fibrohyalinosis in the skin flap. The clinical picture was more severe in the right shoulder, with repeated episodes of skin ulceration. Therefore, in September 2015, an excisional biopsy of the lesion and repair using a latissimus dorsi myocutaneous flap and skin graft were performed (Fig. 5a, b, c, d, e, f). The histological examination showed a picture consistent with radiation damage. In the early post-operative period, a minor surgical revision was required because of the wound’s partial breakdown. The patient’s left shoulder underwent two fat grafting surgeries in October 2015 and January 2017; however, the clinical picture continued to deteriorate, leading to the development of skin ulcers. In November 2017, a second surgery was performed to excise the ulcerative lesions en bloc, and the ipsilateral pedicled latissimus dorsi musculocutaneous flap was harvested and transposed to the shoulder for definitive repair (Fig. 6a, b, c, d, e, f). Histological examination revealed moderately differentiated squamous carcinoma infiltrating the superficial dermis, which was associated with skin atrophy compatible with radiodystrophy. After the past procedure, the wound healing proceeded uneventfully. Regarding shoulder mobility, the latest MRI revealed a complete tear of the rotator cuff, with retraction of the supraspinatus tendon, and a partial lesion of the subscapularis. These findings do not represent a novel occurrence but had originated before the patient’s presentation for evaluation. At this juncture, surgical intervention is deemed unfeasible. This condition limits the overall abduction of both upper extremities to <90°.

After a 3-month period, physical therapy was discontinued due to the limited achievable outcomes. Notwithstanding these limitations, the patient resides independently and is capable of managing activities of daily living with some difficulties, albeit without requiring external assistance.
The skin changes resulting from radiation treatment can lead to severe symptoms, including skin breakdown, itching, flushing, permanent discoloration, sunburn-like rashes, and more, depending on the radiation dose [4,5,6,17]. This issue is concerning for both patients, who worry about its impact on their QoL, and clinicians, who are concerned about the potential for tumor recurrence or degeneration, particularly in SCC [15,16,18]. In case #1, the MRI performed pre-operatively was reassuring about a local recurrence of the myxofibrosarcoma, given its propensity to grow as a thick and solid nodule or mass that was not noticeable in scans of the cancer field. However, the atrophic ulcer of about 7 × 6 cm, which emerged 18 years after the RT administration, posed a concrete risk of skin cancer development. In this case, we decided not to perform an incisional biopsy of the ulcer, because even if it would have resulted in a non-tumor lesion, the need for a wide resection of all the dermatitis area was necessary to warrant stable healing. The presence of supra liquid seroma above the glenohumeral joint was previously recognized as a side effect of post-radiant surgery but was never thought to be a potential sign of local sarcoma relapse in case #2. Recently, the appearance of the overlying skin underwent dramatic changes, with the formation of several fistulas and irregularities in the subcutaneous layer, suggesting the presence of a multinodular mass [19].
Even though the pre-operative imaging did not reveal any concrete sign of subcutaneous proliferation, the marked alteration of the skin surface has led us to wide resection for histologic examination. In this case, the reconstruction was planned only after obtaining the pathology response. We attempted the most effective and reliable surgery to close the wound, but the flap failure complicated the healing process and forced us to perform a much more demanding surgery, a microsurgical reconstruction. In both instances, skin changes were the main factors that led us to perform wide resection. In case #3, the patient had to undergo surgery after attempting to address the skin instability with a regenerative medicine procedure through fat transfer, which is less aggressive than the traditional excisional approach. However, despite this less invasive approach, the patient’s shoulder skin developed chronic ulcers, which necessitated surgery. It is noteworthy that when the specimen from the shoulder that was most clinically affected was examined, no evidence of cancer was found. Conversely, the contralateral shoulder, which had been treated later due to its less compromised condition, was found to have developed SCC. This case highlights the limitations of physical examination and even of the gold standard imaging techniques, as they may not always be able to detect the early signs of cancer or local recurrence with 100% accuracy, especially when there is tumoral degeneration present.
Assuming that non-melanoma skin cancer represents the most significant potential risk arising from this condition, and given that such risk is unlikely to diminish over time, as suggested in the literature, an examination of an affected large skin surface, even when conducted with utmost thoroughness and precision using advanced imaging and diagnostic tools [20], will inevitably result in a higher rate of false-negative and false-positive results. This inherent diagnostic challenge is further complicated by the potential for multiple lesions to develop simultaneously or in close succession, making comprehensive monitoring even more challenging. Moreover, the dynamic nature of skin changes over time, influenced by factors such as aging, sun exposure, and hormonal fluctuations, can further obscure the early signs of malignancy. Consequently, a multifaceted approach combining regular screenings, patient education on self-examination, and advanced technological solutions may be necessary to mitigate the increased risk of misdiagnosis.
Some may argue that a diagnostic incisional biopsy can resolve any doubt about the nature of the problem, providing essential information to decide the viable options for treatment. However, histological tissue assessment has several limitations. First, there is debate about exactly where the biopsy should be taken within the irradiated area, suggesting that different physicians may have varying opinions on the most appropriate or effective spot to excise tissue samples. As a consequence of inadequate tissue resection, pathologists can struggle to detect isolated cells or limited masses of the tumor if the tissue is collected from a hypertrophic scar or desquamated ulcer border [3]. Second, performing multiple biopsies in patients with skin fragility or capillary deficiency poses significant challenges and risks. The compromised structural integrity of the skin, coupled with inadequate blood supply, creates an environment in which even minor interventions can lead to complications. In these cases, the healing process is already impaired due to the underlying conditions, making it difficult for the body to repair and regenerate tissue effectively. Consequently, what might typically be a small and easily manageable biopsy site can potentially develop into an extensive wound. Finally, even if cancer is not found, the risk of future degeneration remains [4], which requires close follow-up. This persistent uncertainty can significantly affect an individual’s mental health and overall QoL. Ongoing worry and anxiety associated with a potential cancer diagnosis can lead to stress, depression, and other psychological challenges that severely impact the patient’s QoL.
The gold standard approach to sarcoma typically involves a multidisciplinary strategy incorporating surgery, radiation therapy, and chemotherapy, tailored to the individual patient’s disease stage, tumor characteristics, and overall health status. However, RT could lead to various cutaneous complications, including the development of radiodermatitis with skin rashes, changes in skin color and texture, skin ulcerations, and subsequent development of cutaneous carcinomas. Given the evident challenge in distinguishing between the malignancy and benign nature of such lesions, it is necessary to evaluate each case individually and thoroughly inform the patient about the pros and cons of surgical treatment, which in some cases may require extensive resections and major procedures. The comprehensive understanding of the potential complications of RT underscores the importance of close monitoring and proactive management of cutaneous issues in patients undergoing this treatment modality.
After therapeutic or adjuvant RT, the shoulder may develop swelling, skin ulceration, and radiation-induced cancer. In this scenario, a wide excision is often required to achieve a diagnosis with functional and stable healing. Therefore, a full comprehension of surgical management may be crucial for supporting the best reconstructive strategy.
References
- 1.Lebas A, Le F vre C, Waissi W, Chambrelant I, Brinkert D, Noël G. Prognostic factors in extremity soft tissue sarcomas treated with radiotherapy: Systematic review of the literature. Cancers (Basel) 2023;15:4486. [Google Scholar]
- 2.Weissmann T, Rmckert M, Putz F, Donaubauer AJ, Hecht M, Schnellhardt S, et al. Low-dose radiotherapy of osteoarthritis: From biological findings to clinical effects-challenges for future studies. Strahlenther Onkol 2023;199:1164-72. [Google Scholar]
- 3.Malakoutikhah Z, Mohaghegh F, Derakhshan M, Mehdizadeh MJ. RadioMJ. Radioadiodeh MJ. Radiolopment of squamous cell carcinoma and undifferentiated pleomorphic sarcoma of scalp. Clin Case Rep 2022;10:e6058. [Google Scholar]
- 4.Singh M, Alavi A, Wong R, Akita S. Radiodermatitis: A review of our current understanding. Am J Clin Dermatol 2016;17:277-92. [Google Scholar]
- 5.Yang X, Ren H, Guo X, Hu C, Fu J. Radiation-induced skin injury: Pathogenesis, treatment, and management. Aging (Albany NY) 2020;12:23379-93. [Google Scholar]
- 6.Borrelli MR, Shen AH, Lee GK, Momeni A, Longaker MT, Wan DC. Radiation-induced skin fibrosis: Pathogenesis, current treatment options, and emerging therapeutics. Ann Plast Surg 2019;83(4S Suppl 1):S59-64. [Google Scholar]
- 7.Callegaro D, Gronchi A. Radiotherapy in retroperitoneal liposarcoma: Are we looking for an answer in the wrong place? Ann Surg Oncol 2023;30:675-7. [Google Scholar]
- 8.Mendelsohn FA, Divino CM, Reis ED, Kerstein MD. Wound care after radiation therapy. Adv Skin Wound Care 2002;15:216-24. [Google Scholar]
- 9.Kumar PP, Newland JR. Radiation oncogenesis. J Natl Med Assoc 1980;72:687-90. [Google Scholar]
- 10.Nepon H, Safran T, Reece EM, Murphy AM, Vorstenbosch J, Davison PG. Radiation-induced tissue damage: Clinical consequences and current treatment options. Semin Plast Surg 2021;35:181-8. [Google Scholar]
- 11.Najafi M, Motevaseli E, Shirazi A, Geraily G, Rezaeyan A, Norouzi F, et al. Mechanisms of inflammatory responses to radiation and normal tissues toxicity: Clinical implications. Int J Radiat Biol 2018;94:335-56. [Google Scholar]
- 12.Cuperus E, Leguit R, Albregts M, Toonstra J. Post radiation skin tumors: Basal cell carcinomas, squamous cell carcinomas and angiosarcomas. A review of this late effect of radiotherapy. Eur J Dermatol 2013;23:749-57. [Google Scholar]
- 13.Shore RE. Radiation13.2106cell carcinomas and ang. Med Pediatr Oncol 2001;36:549-54. [Google Scholar]
- 14.Kuwahara M, Yurugi S, Ando J, Takeuchi M, Miyata R, Harada M, et al. Squamous cell carcinoma developed in a chronic radiation-induced chest wall ulcer that is difficult to undergo thorough preoperative histological examination. Int J Surg Case Rep 2020;72:467-70. [Google Scholar]
- 15.Landthaler M, Hagspiel HJ, Braun-Falco O. Late irradiation damage to the skin caused by soft X-ray radiation therapy of cutaneous tumors. Arch Dermatol 1995;131:182-6. [Google Scholar]
- 16.Yokota T, Roppongi T, Kanno K, Tsutsumi H, Sakamoto I, Fujii T. Radiation-induced squamous cell carcinoma of the chest wall seven years after adjuvant radiotherapy following the surgery of breast cancer: A case report. Kyobu Geka 2000;53:1133-6. [Google Scholar]
- 17.Yahyapour R, Motevaseli E, Rezaeyan A, Abdollahi H, Farhood B, Cheki M, et al. Mechanisms of radiation bystander and non-targeted effects: Implications to radiation carcinogenesis and radiotherapy. Curr Radiopharm 2018;11:34-45. [Google Scholar]
- 18.Bazalińazali0.Przybek-Mita J, Barańska B, Więch P. Marjolin’s ulcer in chronic wounds - review of available literature. Contemp Oncol (Pozn) 2017;21:197-202. [Google Scholar]
- 19.Abatzoglou S, Turcotte RE, Adoubali A, Isler MH, Roberge D. Local recurrence after initial multidisciplinary management of soft tissue sarcoma: Is there a way out? Clin Orthop Relat Res 2010;468:3012-8. [Google Scholar]
- 20.Badiu IM, Korecka K, Orzan AO, Spadafora M, Longo C, Forsea AM, et al. A review of non-invasive skin imaging in merkel cell carcinoma: Diagnostic utility and clinical implications. Cancers (Basel) 2024;16:3586. [Google Scholar]











