Atraumatic bilateral patellar tendon ruptures though unusual presentation, early diagnosis, and prompt surgical repair are essential for restoring knee function and achieving optimal functional outcomes
Dr. Venkata Vinay Atluri, Department of Orthopaedics, Mamata Academy of Medical Sciences, Hyderabad, Telangana, India. E-mail: vinayatluri.ortho@gmail.com
Introduction: Bilateral patellar tendon rupture is an uncommon reason for extensor mechanism dysfunction. Various predisposing factors, including systemic diseases and the use of steroids or antibiotics, can elevate the risk. The patient typically presents with an inability to extend the knee, generalized pain and swelling, and a high-riding patella observed on lateral radiographs.
Case Report: We report a case involving a 44-year-old man with no underlying risk factors or systemic disease who sustained a bilateral patellar tendon rupture following minor trauma. The patient was treated with bilateral primary transosseous end-to-end tendon repair, followed by a brief period of immobilization and an intensive rehabilitation program. Six months post-surgery, he could walk unassisted without pain, regain full range of motion in both knees, and carry out daily activities without limitations.
Conclusion: Timely diagnosis and immediate surgical intervention are crucial to preventing complications related to extensor mechanism failure and ensuring favorable functional outcomes.
Keywords: Patellar tendon injury, spontaneous tendon rupture, extensor mechanism, trauma, knee.
The patellar tendon comprises large collagen fibers, consisting of approximately 90% type I collagen and <10% type III collagen [1]. The remaining tendon matrix includes elastin, proteoglycans, and other non-collagen glycoproteins [1]. Its vascular supply is derived from the infrapatellar fat and the retinaculum, while both ligament attachments are relatively avascular and consist of fibrocartilage [2]. With a sagittal thickness of 4–7 mm, the patellar tendon is a robust structure that typically does not rupture under normal physiological conditions [1]. A healthy patellar tendon requires a force equivalent to 17.5 times the body weight to rupture [3]. When the patellar tendon ruptures, it disrupts the extensor mechanism, leading to significant functional impairment and gait abnormalities [4,5]. Bilateral patellar tendon rupture without significant trauma is an infrequent injury, even when predisposing factors are present. This report presents a bilateral spontaneous patellar tendon rupture without predisposing risk factors.
We present the case of a 44-year-old male with a body mass index of 24.9 kg/m², no significant personal or family medical history, no history of rheumatoid disease, and no recent use of antibiotics, steroids, or other medications. The patient visited the outpatient department complaining of a bilateral popping sensation, followed by anterior knee pain and an inability to walk, which occurred while he was on his way to the washroom in the middle of the night. As he attempted to prevent himself from falling backward, he felt immediate pain and a tearing sensation in his right anterior knee. He shifted his weight to his flexed left knee to stabilize himself, where he experienced another “pop” and pain. His knees then buckled, causing him to fall to the ground, and he could not stand or extend his legs at the knee joint. On physical examination, there was bilateral joint effusion, an infrapatellar gap, and a complete loss of active knee extension on both sides. He was unable to bear weight on either leg. There were no signs of neurovascular deficits in either knee.
Investigations
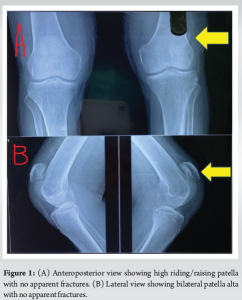
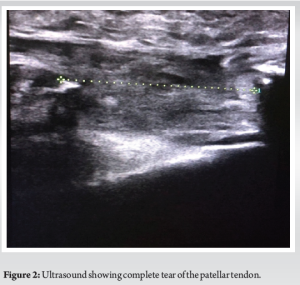
The patient underwent bilateral anteroposterior and lateral radiographs of the knees, which revealed bilateral patella alta and anterior soft-tissue swelling without any visible fractures (Fig. 1a, b). An ultrasound was performed on both knees to evaluate the injury further, confirming a complete bilateral patellar tendon tear at the inferior pole of patella (Fig. 2). Additional laboratory tests, including a screen for connective tissue disease, rheumatoid factor, and anti-cyclic citrullinated peptide antibody, were all within normal limits, ruling out underlying systemic conditions that could have contributed to the injury.
Surgery
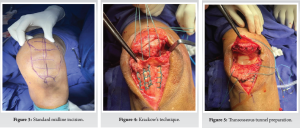
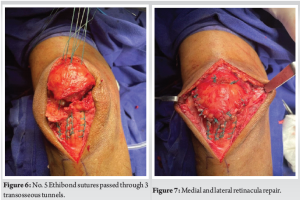
The patient consented to bilateral patellar tendon repair as the tear was recent, and there were no associated risk factors indicating morphological changes in the tendon structure. A standard midline incision exposed both knees (Fig. 3). During the procedure, both tendons were found to be torn in their substance near the inferior patellar pole, with disruption of the medial and lateral retinaculum. The tendons were repaired using Krackow’s technique (Fig. 4) and transosseous tunnels (Fig. 5). The inferior pole of the patella was prepared and curetted before a guide pin for the anterior cruciate ligament was passed longitudinally through the patella to guide No. 5 Ethibond sutures through three transosseous tunnels (Fig. 6). This was further reinforced with interrupted sutures. The medial and lateral retinacula were repaired using No. 1 Vicryl, an absorbable suture (Fig. 7).
Post-operative examination under anesthesia showed that both knees were stable against varus/valgus stress, and the anterior and posterior cruciate ligaments were intact. The wound was closed in layers, and meticulous hemostasis was achieved. A post-operative X-ray showed the bilateral patellae in a good position (Fig. 8). The patient was immobilized in a bilateral range of motion (ROM) knee brace, locked in extension. Weight-bearing was allowed as tolerated and supervised rehabilitation began immediately. ROM was gradually increased: 30° at 2 weeks, 60° at 4 weeks, and 90° at 6 weeks bilaterally. At 8 weeks, unrestricted ROM in the brace was permitted, and the braces were slowly weaned off, starting at 10 weeks post-surgery. At the 3-month follow-up, the patient had full active ROM of 0–120° in both knees and was mobilizing without limitations. By 6 months post-operative, the patient returned to his office job with good quadriceps strength and ROM (Fig. 9 and 10).
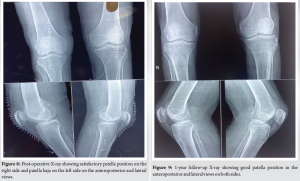

At the 1-year follow-up, a physical examination revealed well-healed scars, no ligamentous instability, or pain on palpation of the patellar tendons, with bilateral ROM from 0 to 130°. An X-ray confirmed that the patellae were in a satisfactory position (Fig. 9).
The knee extensor mechanism consists of the quadriceps muscle and tendon, the medial and lateral patellar retinacula, the patella, the patellar tendon, and the tibial tubercle [6]. The medial and lateral patellar retinacula stabilize the joint on either side of the patella [6]. The patellar tendon is a robust structure requiring a force of 17.5 times body weight to rupture [3]. Daily activities like climbing stairs generate approximately 3.3 times body weight, while athletic activities such as acceleration, deceleration, and jumping produce forces of 7–8 times body weight [7]. Patellar tendon rupture usually results from underlying weaknesses or conditions, including connective tissue disorders, autoimmune diseases, steroid or fluoroquinolone use, and systemic illnesses such as systemic lupus erythematosus, inflammatory polyarthralgia, and chronic renal failure [8-11]. Our patient had no known risk factors for patellar tendon rupture. Diagnosis can be challenging, with 38% of cases missed on initial examination [12]. Early diagnosis and treatment are crucial, as delaying surgery beyond 6 weeks can lead to prolonged rehabilitation and poorer outcomes due to quadriceps atrophy [13]. Various repair techniques have been described, including end-to-end repairs [10], repairs protected with tension band wiring [8], allograft repairs [14], and augmented repairs using autografts from the semitendinosus and gracilis muscles [11,15,16]. For purely traumatic injuries, primary repair through direct sutures or transosseous reinsertion is generally sufficient, while chronic degeneration or predisposing factors may necessitate suture reinforcement or augmentation. In this case, we performed a primary repair using No. 5 Ethibond through a transosseous technique. Despite the generally good outcomes following acute repair, re-rupture rates can be as high as 50%. Nevertheless, strong repair, minimal bracing, and early controlled mobilization can effectively prevent quadriceps atrophy and re-rupture. Rehabilitation protocols vary [17] and should be adapted based on the stability of the intraoperative repair. We immobilized the knee in full extension for 2 weeks, initiated static quadriceps strengthening exercises postoperatively, and increased the ROM by 30° bi-weekly, with the brace fully weaned off by 8–10 weeks. The patient returned to pre-injury status within 6 months without the need for augmentations, grafts, reinforcements, or internal devices, demonstrating a cost-effective approach to managing acute traumatic bilateral patellar tendon ruptures.
We present a case of bilateral patellar tendon rupture without any risk factors. The bilateral nature of the injury can complicate rehabilitation. We attribute the excellent and prompt functional outcomes to several factors: early tendon repair, proper suture tension and strength, minimal immobilization time, an intensive and controlled physiotherapy program, and the patient’s strong commitment to the recovery process.
- These injuries typically show a bimodal distribution, primarily affecting individuals aged 20–30 and 40–50.
- When bilateral extensor mechanism injuries are clinically suspected, a thorough examination and radiographs of both knees should be conducted.
- A suitable rehabilitation protocol for patients without risk factors involves early weight-bearing with a gradual return to full ROM over 6–8 weeks.
References
- 1.Sousa HC, Choupina B, Ventura M, Pereira RS, Costa A, Carvalho PJ. Bilateral patellar tendon rupture: A case report. Int J Res Orthop 2022;8:251-5. [Google Scholar | PubMed]
- 2.Pang J, Shen S, Pan WR, Jones IR, Rozen WM, Taylor GI. The arterial supply of the patellar tendon: Anatomical study with clinical implications for knee surgery. Clin Anat 2009;22:371-6. [Google Scholar | PubMed]
- 3.Zernicke RF, Garhammer J, Jobe FW. Human patellar-tendon rupture. J Bone Joint Surg Am 1977;59:179-83. [Google Scholar | PubMed]
- 4.Pengas IP, Assiotis A, Khan W. Adult native knee extensor mechanism ruptures. Injury 2016;47:2065-70. [Google Scholar | PubMed]
- 5.Savarese E, Bisicchia S, Amendola A. Bilateral spontaneous concurrent rupture of the patellar tendon in a healthy man: Case report and review of the literature. Musculoskelet Surg 2010;94:81-8. [Google Scholar | PubMed]
- 6.Murphy SM, McAleese T, Elghobashy O, Walsh J. Bilateral patellar tendon rupture following low-energy trauma in a young patient without predisposing risk factors. Trauma Case Rep 2022;40:100643. [Google Scholar | PubMed]
- 7.Nordin M, Frankel VH. Biomechanics of the knee. In: Nordin M, Frankel VH, editors. Basic Biomechanics of the Musculoskeletal System. 2nd ed. Philadelphia, PA: Lea and Febiger; 1989. p. 115-34. [Google Scholar | PubMed]
- 8.Mencia M, Edwards A, Ali T. Spontaneous bilateral patellar tendon ruptures in a patient with chronic renal failure: A case report. Intern J Emerg Med 2012;7:1-4. [Google Scholar | PubMed]
- 9.Clark SC, Jones MW, Choudhury RR, Smith E. Bilateral patellar tendon rupture secondary to repeated local steroid injections. J Accid Emerg Med 1995;12:300-1. [Google Scholar | PubMed]
- 10.Cooney LM Jr., Aversa JM, Newman JH. Insidious bilateral infrapatellar tendon rupture in a patient with systemic lupus erythematosus. Ann Rheum Dis 1980;39:592-5. [Google Scholar | PubMed]
- 11.Juliato RH, Boschi LH, Juliato RF, de Freitas AP, França AF, Bottura LB. Bilateral atraumatic patellar ligament rupture-case report. Rev Bras Ortop (Sao Paulo) 2019;54:223-7. [Google Scholar | PubMed]
- 12.Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am 1981;63:932-7. [Google Scholar | PubMed]
- 13.Ecker ML, Lotke PA, Glazer RM. Late reconstruction of the patellar tendon. J Bone Joint Surg Am 1979;61:884-6. [Google Scholar | PubMed]
- 14.Seng C, Lim YJ, Pang HN. Spontaneous disruption of the bilateral knee extensor mechanism: A report of two cases. J Orthop Surg (Hong Kong) 2015;23:262-6. [Google Scholar | PubMed]
- 15.Espregueira-Mendes J, Andrade R, Michael MJ, Sarmento A, Sevivas N, Rocha R, et al. Augmentation of patellar tendon repair with autologous semitendinosus graft-Porto technique. Arthrosc Tech 2017;6:e2271-6. [Google Scholar | PubMed]
- 16.Takazawa Y, Ikeda H, Ishijima M, Kubota M, Saita Y, Kaneko H, et al. Reconstruction of a ruptured patellar tendon using ipsilateral semitendinosus and gracilis tendons with preserved distal insertions: Two case reports. BMC Res Notes 2013;6:361. [Google Scholar | PubMed]
- 17.Noteboom JT, Lester MN. Bilateral simultaneous infrapatellar tendon ruptures: A case study. J Orthop Sports Phys Ther 1994;20:166-70. [Google Scholar | PubMed]









