Neglected flexor pollicis longus tendon lacerations in children can be successfully managed with single-stage tendon reconstruction without the use of grafts.
Dr Dimitrios Giotis, Department of Orthopaedic, General Hospital of Ioannina “G. Hatzikosta”, 60 Stratigou Makrigianni Avenue, 45445. Ioannina, Greece. E-mail: dimitris.p.giotis@gmail.com
Introduction: Lacerations of the flexor pollicis longus (FPL) tendon are rare in children and should be treated promptly. This study aims to present a rare case of a neglected FPL tendon laceration in a child, successfully managed with single-stage reconstruction without the use of grafts.
Case Report: A 12-year-old patient was admitted to our hospital with an inability to flex the interphalangeal joint of the right thumb following an injury sustained 2 months earlier. Clinical examination revealed a neglected FPL tendon laceration in zone II. Intraoperatively, it was observed that the distal stump of the tendon measured approximately 1 cm, while the proximal stump was attached to the A1 pulley. In addition, the oblique pulley was narrowed, obstructing the passage of the tendon. To address this, a Z-plasty of the oblique pulley was performed. Following tendon debridement, a 2-cm-long tendon deficit was identified. A carpal tunnel release was conducted to facilitate further tendon mobilization. The distal stump was sutured, and a Z-plasty lengthening of the tendon by 1.5 cm was performed after assessing the “tenodesis effect.” An extension block cast was applied after skin closure. Three weeks later, the patient was encouraged to perform active flexion-extension movements to the neutral position. By 6 weeks postoperatively, the patient was advised to perform full active range-of-motion exercises and physiotherapy. Four months after surgery, the patient had fully resumed pre-injury activities exhibiting full active flexion and a 10° extension deficit at the IP joint of the thumb.
Conclusion: In cases of neglected pediatric flexor tendon lacerations, single-stage tendon reconstruction without grafting can be a viable option to avoid complex surgical procedures and potentially unpredictable outcomes.
Keywords: Single-stage reconstruction, flexor pollicis longus tendon, neglected laceration, rupture, pediatric, Z-plasty, zone II
Flexor tendon injuries in children are uncommon, with an incidence of <4 new cases per 100,000 people annually [1]. Knife and glass lacerations are the primary causes, predominantly resulting in zone II and V injuries involving the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) tendons [2]. Notably, the little finger is the most frequently injured, while the thumb is rarely affected, which explains the scarcity of reported cases of pediatric flexor pollicis longus (FPL) tendon lacerations in the literature [1,3,4]. Neglected FPL tendon lacerations are even rarer, typically resulting from overlooked hand injuries in young children, particularly during the pre-school years when physical examinations can be challenging due to non-cooperation [5]. Consequently, such cases often present late, posing significant challenges for hand surgeons [6]. As with flexor tendon injuries in adults, primary repair remains the gold-standard treatment for pediatric lacerations if performed within 4 weeks of the initial trauma [6,7]. However, when timely repair is not feasible, as in neglected cases, alternatives such as arthrodesis, tendon transfer, or tendon reconstruction using grafts may be necessary [6,7]. Post-operative rehabilitation in pediatric patients presents an additional challenge, as young children may struggle to adhere to mobilization protocols. Consequently, rehabilitation approaches vary widely, with complete immobilization being preferred in some cases to protect the repaired tendon [7]. The purpose of the present study is to present a rare case of a neglected FPL tendon laceration in a child, successfully managed with single-stage reconstruction without the use of grafts. The post-operative management that was followed is also highlighted.
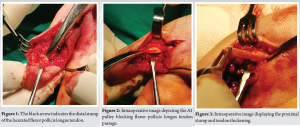
A right-handed 12-year-old patient presented to the emergency department with an inability to flex the interphalangeal (IP) joint of the right thumb following a knife injury sustained two months earlier. He had not sought medical care until this presentation. Clinical examination revealed a neglected FPL tendon laceration in zone II, with a visible scar. The IP joint displayed a full passive range of motion without any contracture. Neurovascular assessment of the thumb, including the Allen and pinprick tests, showed no compromise. The patient was admitted for surgical exploration and treatment. In the operating room, under general anesthesia and with tourniquet application, a Bruner incision was made encompassing the pre-existing scar. Surgical exploration revealed that the distal stump of the tendon was slightly longer than 1 cm, while the proximal stump was adherent to the A1 pulley (Fig. 1). A thickening of the proximal stump was identified, which hindered its passage through the A1 pulley; therefore, the pulley was sacrificed (Fig. 2 and 3). Further, examination revealed narrowing of the oblique pulley, which was addressed by performing a Z-plasty using 3-0 polyglactin suture to widen the tunnel and facilitate tendon gliding (Fig. 4). Debridement of the tendon was then performed, resulting in a 2-cm-long tendon deficit.
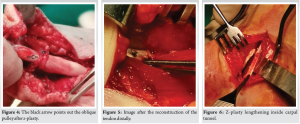
A carpal tunnel release was undertaken to mobilize the proximal tendon further, resolving adhesions and vinculae. A long Z incision was performed to facilitate the distal repair of the tendon. End-to-end repair of the tendon was achieved distally using a two-strand modified Kessler technique for the core suture and a simple running technique for the epitenon suture, utilizing 3-0 and 6-0 polypropylene sutures, respectively (Fig. 5). Side-to-side repair with 4-0 nylon suture was used for tendon Z-plasty lengthening achieving an additional 1.5 cm of length after evaluating the “tenodesis effect” (Fig. 6). Skin closure was completed with nylon suture, and an extension block cast was applied with the wrist in 30° of flexion. The patient was discharged on the 1st post-operative day, and passive flexion of the IP joint was initiated on the 3rd post-operative day. Three weeks postoperatively (post-op), active flexion-extension movement to the neutral position was encouraged using a new extension block cast. Six weeks after surgery, the patient was advised to perform full active range-of-motion exercises and begin physiotherapy to accelerate recovery and regain strength (Fig. 7).
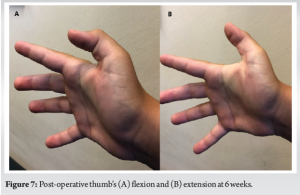
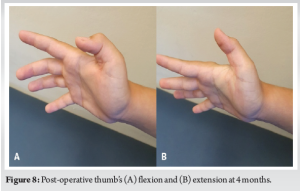
Four months post-operative, the patient demonstrated full active flexion with an extension deficit of approximately 10° at the IP joint of the thumb. However, he had fully returned to his pre-injury activities (Fig. 8). One year after the tendon reconstruction, the extension deficit remained unchanged, despite the absence of functional limitations.
Few studies in the literature focus on pediatric FPL tendon lacerations, as they are far less common than FDS and FDP tendons injuries [3,4]. Interestingly, FPL tendon repair tends to yield better outcomes compared to FDS and FDP repairs [3]. This difference may stem from the simpler anatomy of the thumb, with its single tendon and less complex fibro-osseous tunnel consisting of just three pulleys [3,4]. Neglected FPL tendon lacerations in pediatric patients are extremely rare [7]. The critical role of the thumb in hand function often compels patients or caregivers to seek medical attention promptly following an FPL laceration [5]. However, in young children, limited cooperation, concealment of injuries, or unawareness of hand disability can delay diagnosis and treatment [2]. Oka documented three cases of neglected FPL lacerations during infancy that remained untreated for over 10 years [5]. In our case, although the patient initially underestimated the severity of the injury, medical advice was sought within 2 months. Diagnosis of the neglected FPL tendon rupture in our patient was straightforward, based on the mechanism and pattern of injury. Thus, radiological imaging was deemed unnecessary. However, in cases with unclear histories or mechanisms of injury, diagnosis can be challenging [5]. The hand surgeon must consider congenital anomalies such as absent FPL, trigger thumb, or anomalous FPL insertion, which can mimic FPL lacerations by limiting IP joint flexion [8]. Diagnostic tools like sonography can confirm tendon rupture, while radiographs may reveal thumb hypoplasia indicative of congenital anomalies [8]. MRI provides high-resolution imaging of soft tissue, aiding both diagnosis and pre-operative planning [9]. When managing pediatric flexor tendon injuries, anatomical differences during growth must be considered [2]. Although pulley positions and characteristics in children resemble those of adults, pediatric tendons are thinner and narrower, necessitating tailored surgical techniques [2]. Pediatric flexor tendon injuries are often categorized by age group: preschoolers (<5 years), children (5–10 years), and teenagers (11–15 years) [10]. In preschoolers, with a thin tendon, only a two-strand Modified Kessler core repair with fine sutures may be feasible [2]. In older children, a six-strand repair using the figure-of-eight technique is recommended by Al-Qattan due to its simplicity of application and greater resistance to failure during early mobilization compared to the Modified Kessler technique [11]. For our teenage patient, we opted to avoid the bulky figure-of-eight repair due to its potential to generate adhesions and hinter tendon gliding, especially considering his neglected rupture and narrowed pulley system. Primary repair is the gold standard for flexor tendon injuries treated within 4 weeks of trauma [12]. Beyond this window, or in cases involving severe soft-tissue damage, alternative options include arthrodesis or tendon reconstruction with one- or two-stage grafting [7]. Plantaris and palmaris longus tendons are commonly used for one-stage grafting in pediatric cases, yielding favorable outcomes in patients with intact neurovascular bundles with no excessive scarring or joint contracture [13]. In cases of severe scarring, injured pulley systems, or neurovascular compromise, two-stage grafting should be considered, although guidelines remain controversial in the literature [7,13]. Two-stage grafting procedures include the standard two-stage flexor tendon reconstruction by Valenti and Gilbert, as well as the Paneva-Holevich technique [2]. These are highly demanding operations that require significant technical expertise from the surgeon and are associated with high complication rates [13]. In our patient, we ruled out IP arthrodesis due to its impact on thumb function [14]. In addition, tendon reconstruction with grafting was unnecessary given the mild to moderate scarring, absence of joint contracture, and the concern for donor-site morbidity in a young patient. Instead, single-stage reconstruction with Z-plasty lengthening was selected. This single-stage technique, involving step-cut lengthening along the proximal tendon stump, was successfully applied by Chong and Chen in an adult patient with a neglected FPL tendon laceration and tendon loss up to 2 cm [14]. Although we were initially reluctant to implement it in our case, as pediatric tendons are biologically smaller and thinner, making the compromise of the tendon’s overall integrity a primary concern, we proceeded successfully with this single-stage method. To the best of our knowledge, this is the only reported case in the literature of a single-stage reconstruction following a neglected FPL tendon laceration in a pediatric patient without the use of tendon grafting or tendon transfer. Another major concern for hand surgeons is the rehabilitation following a pediatric flexor tendon injury [13]. While early mobilization is favored in adults for superior functional outcomes, it is often contraindicated in younger children due to the risk of tendon rupture [15]. Rehabilitation protocols vary by age [2]. Preschoolers are the most challenging group to manage postoperatively; thus, immobilization with an above-elbow cast for three to 4 weeks is recommended to prevent re-rupture, as they are less prone to adhesion formation compared to adults [2,7,15]. In older children and teenagers, early passive mobilization is generally safe, especially following tendon reconstruction with grafting [7,15]. Several therapeutic protocols are described in the literature, including the Duran and Kleinert methods, which focus on early passive motion [15]. In specific cases where the patient is cooperative and the biomechanically more durable figure-of-eight technique has been used, early protected active mobilization may also be initiated [2]. In our patient, early passive motion was commenced immediately postoperatively, as complete immobilization could be detrimental to the functional outcome, particularly after a neglected laceration with pre-existing adhesions.
Neglected pediatric flexor tendon lacerations are extremely rare injuries that pose a significant challenge to hand surgeons, since primary repair is often no longer feasible. Under those circumstances, single-stage tendon reconstruction without grafting can be a viable, though highly demanding, option. Early medical intervention would be essential to prevent the need for complex procedures with potentially unpredictable outcomes.
In pediatric cases of neglected FPL tendon lacerations, single-stage reconstruction techniques, including tendon lengthening, and carpal tunnel release, can effectively address tendon deficits and obstructions. This avoids the need for grafts and complex multi-stage procedures while enabling good functional recovery with appropriate rehabilitation.
References
- 1.Huynh MN, Ghumman A, Agarwal A, Malic C. Outcomes after flexor tendon injuries in the pediatric population: A 10-year retrospective review. Hand (N Y) 2022;17:278-84. [Google Scholar | PubMed]
- 2.Al-Qattan MM. Flexor tendon injuries in the child. J Hand Surg Eur Vol 2014;39:46-53. [Google Scholar | PubMed]
- 3.Grobbelaar AO, Hudson DA. Flexor pollicis longus tendon injuries in children. Ann R Coll Surg Engl 1995;77:135-7. [Google Scholar | PubMed]
- 4.Orhun E, Polatkan S, Polatkan O, Nuzumlali E, Kantarci U. Repair of zone 2 flexor pollicis longus lacerations in children. J Hand Surg Br 1999;24:54-5. [Google Scholar | PubMed]
- 5.Oka Y. Reconstruction of the flexor pollicis longus tendon ruptured, but untreated, during infancy. Tokai J Exp Clin Med 2000;25:23-6. [Google Scholar | PubMed]
- 6.Reito A, Manninen M, Karjalainen T. The effect of delay to surgery on major complications after primary flexor tendon repair. J Hand Surg Asian Pac Vol 2019;24:161-8. [Google Scholar | PubMed]
- 7.Yamazaki H, Kato H, Uchiyama S, Iwasaki N, Ishikura H, Minami A. Long term results of early active extension and passive flexion mobilization following one-stage tendon grafting for neglected injuries of the flexor digitorum profundus in children. J Hand Surg Eur Vol 2011;36:303-7. [Google Scholar | PubMed]
- 8.Yavari M, Farzam R, Riyahi A. Tendon transfer in congenital deficiency of flexor pollicis longus. World J Plast Surg 2017;6:123-4. [Google Scholar | PubMed]
- 9.Demirseren ME, Afandiyer K, Durgan M, Kilicarslan K, Yorubulut M. Congenital absence of flexor pollicis longus tendon without associated anomalies of thumb hypoplasia: A case report and review of the literature. J Hand (N Y) 2007;2:184-7. [Google Scholar | PubMed]
- 10.Moehrien U, Mazzone L, Bieli C, Weber DM. Early mobilization after flexor tendon repair in children. Eur J Pediatr Surg 2009;19:83-6. [Google Scholar | PubMed]
- 11.Al-Qattan MM, Al-Turaiki TM. Flexor tendon repair in zone 2 using a six-strand ‘figure of eight’ suture. J Hand Surg Eur Vol 2009;34:322-8. [Google Scholar | PubMed]
- 12.Osterman AL, Bozentka DJ. Flexor injuries in children. In: Balderson RA, editor. Operative Techniques in Orthopaedics. Baltimore: W. B. Saunders; 1993. p. 283-5. [Google Scholar | PubMed]
- 13.Courvoisier A, Pradel P, Dautel G. Surgical outcome of one-stage and two-stage flexor tendon grafting in children. J Pediatr Orthop 2009;29:792-6. [Google Scholar | PubMed]
- 14.Chong CW, Chen SH. Step cut lengthening: A technique for treatment of flexor pollicis longus tendon rupture. Ann Plast Surg 2018;80:353-5. [Google Scholar | PubMed]
- 15.Sikora S, Lai M, Arneja JS. Pediatric flexor tendon injuries: A 10-year outcome analysis. Can J Plast Surg 2013;21:181-5. [Google Scholar | PubMed]











