Distal femoral nail (DFN) is a cost-effective alternative to TTC nail, enabling stability, early mobilization, and functional recovery in elderly patients
Dr. Pawan Kumar, Department of Orthopaedics, All India Institute of Medical Sciences, Deoghar, Jharkhand, India. E-mail: reachpawankumar@gmail.com
Introduction: Ankle fracture non-union in elderly patients is challenging due to osteoporotic bone, comorbidities, and risks associated with open reduction and internal fixation (ORIF). Tibiotalocalcaneal (TTC) nail fixation enables early weight-bearing but is costly and not widely available in resource-limited settings.
Case Report: We present an 83-year-old male with a painful, deformed left ankle and non-union of a bimalleolar fracture treated conservatively. Comorbidities included diabetes mellitus and hypertension. Due to fragile skin and high ORIF-associated risks, a distal femoral nail (DFN) was used as a substitute for a TTC nail. A minimally invasive technique was performed, including joint preparation and medial malleolar bone grafting. Weight-bearing was initiated postoperatively.
Conclusion: DFN offered comparable fixation with reduced cost and acceptable complications. This case highlights DFN’s utility as a TTC nail substitute in elderly patients, ensuring stability, early mobilization, and functional recovery in low-resource settings.
Keywords: Distal femur nail, ankle arthrodesis, osteoporotic fracture
Treating ankle non-union in elderly patients presents significant challenges due to osteoporotic bone and the high risk of complications associated with open reduction and internal fixation (ORIF), such as wound dehiscence, implant failure, and infection, with no assurance of fracture healing [1-3]. A major limitation of ORIF is the requirement for prolonged non-weight-bearing mobilization. This is particularly problematic in elderly patients, who often have balance issues and may struggle to adhere to weight-bearing restrictions, increasing the risk of falls and further injuries [4]. Given these challenges, tibiotalocalcaneal (TTC) nail fixation offers a compelling alternative for low-demand elderly patients. This approach prioritizes achieving satisfactory joint alignment and stability, enabling effective pain relief. Unlike ORIF, TTC nail fixation allows for immediate post-operative weight-bearing, significantly improving mobility and reducing the risk of complications. Thus, TTC nail fixation provides a viable solution tailored to the unique needs of elderly patients with ankle non-union.
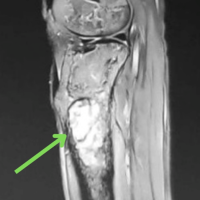
An 83-year-old male presented to our outpatient clinic with a painful and severe varus deformity of the left ankle joint (Fig. 1). He had a limping gait and a history of a left bimalleolar ankle fracture sustained 5 months earlier, which was treated conservatively with a plaster cast at another facility. The fracture had failed to unite, resulting in non-union with deformity, osteopenia, and ankle varus, as confirmed by radiographs (Fig. 2). The patient had a medical history of uncontrolled type 2 diabetes mellitus and hypertension but was independently mobile before the injury. On clinical examination, the sensation over the ankle was intact, but the skin was fragile. Considering the high risk of complications with ORIF, we opted for minimally invasive TTC nailing. However, due to the unavailability of TTC nails in our geographical region in India, a more cost-effective alternative – a distal femoral nail (DFN) – was used for the procedure.

Operative technique
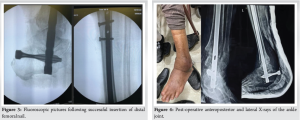
The patient was positioned supine on a radiolucent table. A small, curved incision was made over the medial malleolus, where the non-united fragment was at risk of breaking through the skin. The medial malleolar fragment was excised. Through the same incision, a sliver of cartilage was removed, and the talar dome was flattened using a saw. Drill holes were created in the sclerotic subchondral bone with a 2.5 mm drill bit, and the excised medial malleolar bone was prepared and placed into the joint as a bone graft. The subtalar joint was not opened, nor was any preparation done for it. The ankle was positioned in neutral dorsiflexion with 5° of hindfoot valgus and slightly more external rotation than the contralateral foot. The anterior cortex of the distal tibia was aligned with the anterior edge of the talar dome. Temporary transfixation was achieved using 2.5 mm Kirschner wires placed away from the planned nail path. A small incision was made over the plantar surface of the calcaneum, in line with the fourth metatarsal. A DFN guidewire was inserted and its position was verified under fluoroscopy. A 13 mm cannulated drill was used to open the calcaneum, talus, and tibial metaphysis. The tibial diaphysis was reamed sequentially to 10 mm. A 9 mm DFN was assembled and inserted, ensuring the guidewire did not perforate the calcaneocuboid joint. The nail was locked proximally with two screws under fluoroscopic guidance (Fig. 3a and b). Post-operative radiographs confirmed appropriate alignment (Fig. 4). The wound was closed with 3–0 nylon sutures, and a soft dressing with a below-knee back slab was applied for 2 weeks. The patient was allowed weight-bearing as tolerated. Monthly clinical and radiological follow-ups were conducted until union.
TTC nails are relatively new implants in India, often costly and not widely available, particularly in our geographical area. While tibial nails, which feature a Herzog bend, are an alternative, their smaller screw diameter limits firm fixation in the calcaneus. The DFN, however, shares similarities with TTC nails – it is a straight implant, and its helical blade provides superior fixation in the calcaneus. DFNs are more affordable and widely available, making them a viable option for low-socioeconomic patients. The management of displaced ankle fractures, particularly non-unions in elderly patients, is challenging and lacks a standardized consensus. TTC nails present a promising alternative, as traditional ORIF with bone grafting is associated with complications, including wound breakdown, poor healing, and an inability to ensure prolonged non-weight-bearing periods, which elderly patients often struggle to maintain [3]. Our literature search did not identify studies utilizing DFN as a TTC nail. However, one randomized controlled trial compared conventional TTC nails with ORIF. TTC nail complications include hardware failure, periprosthetic fractures (0–9.6%) [9], screw loosening or breakage (up to 9.6%) [7], and deep infections (0–11%) [5,6]. Nail breakage and periprosthetic fractures are more frequent with shorter nails, emphasizing the importance of using longer nails, as in our case [8,9]. Reoperation rates for TTC nails range from 0 to 27%, with a complication rate as high as 47% in some studies [9-11]. Non-union rates with TTC nails range from 0 to 12%, particularly in diabetic patients [5]. Elderly patients generally do not require formal tibiotalar or subtalar joint preparation duringTTC nail procedures [12]. However, in our case, the impending skin breakdown over the non-united medial malleolus warranted excision, joint preparation, and utilization of the fragment as a bone graft. Literature suggests that reaming, compression, and reduced joint motion stimulate fusion without increasing joint arthritis or hardware failure, especially in low-demand elderly populations [13,14]. In geriatric patients, ORIF and non-operative treatments (e.g., manipulation and casting) are associated with high complication rates. ORIF complication rates reach 20%, doubling with comorbidities such as diabetes or peripheral vascular disease [8,15,16], while non-operative treatment can result in malunion or non-union in up to 73% of cases [17]. TTC nails offer better functional outcomes, with return-to-pre-injury activity levels ranging from 75% to 93% [8,10,14]. This improved functionality is attributed to earlier weight-bearing, as allowed by TTC nails, compared to ORIF or plaster cast treatment. Pre-injury activity level remains a significant predictor of recovery [14].
Utilizing a DFN as a substitute for a TTC nail in geriatric patients with ankle fractures or non-unions offers a viable and cost-effective solution. This approach facilitates early weight-bearing, preserves mobility, and minimizes wound complications. Moreover, the overall complication rates are acceptable, making DFN a practical alternative, especially in regions where TTC nails are unavailable or economically unfeasible.
A DFN for geriatric ankle fractures or non-unions offers a viable, cost-effective alternative to the costly. TTC nail. This approach supports early weight-bearing, preserves mobility, and reduces wound complications. The complication rates are acceptable, making DFN a practical option where TTC nails are unavailable or costly.
References
- 1.Hsu RY, Lee Y, Hayda R, DiGiovanni CW, Mor V, Bariteau JT. Morbidity and mortality associated with geriatric ankle fractures: A medicare part A claims database analysis. J Bone Joint Surg Am 2015;97:1748-55. [Google Scholar | PubMed]
- 2.Seeley DG, Kelsey J, Jergas M, Nevitt MC. Predictors of ankle and foot fractures in older women. The study of osteoporotic fractures research group. J Bone Miner Res 1996;11:1347-55. [Google Scholar | PubMed]
- 3.Ziegler P, Bahrs C, Konrads C, Hemmann P, Ahrend MD. Ankle fractures of the geriatric patient: A narrative review. EFORT Open Rev 2023;8:1-10. [Google Scholar | PubMed]
- 4.Osoba MY, Rao AK, Agrawal SK, Lalwani AK. Balance and gait in the elderly: A contemporary review. Laryngoscope Investig Otolaryngol 2019;4:143-53. [Google Scholar | PubMed]
- 5.Dimitroulias A. Ankle tibiotalocalcaneal nailing in elderly ankle fractures as an alternative to open reduction internal fixation: Technique and literature review. OTA Int 2022;5:e183. [Google Scholar | PubMed]
- 6.Ou C, Baker JF. Hindfoot nailing for displaced ankle fractures in the elderly: A case-control analysis. Injury 2023;54:110921. [Google Scholar | PubMed]
- 7.Caravaggi C, Cimmino M, Caruso S, Dalla Noce S. Intramedullary compressive nail fixation for the treatment of severe charcot deformity of the ankle and rear foot. J Foot Ankle Surg 2006;45:20-4. [Google Scholar | PubMed]
- 8.Jonas SC, Young AF, Curwen CH, McCann PA. Functional outcome following tibio-talar-calcaneal nailing for unstable osteoporotic ankle fractures. Injury 2013;44:994-7. [Google Scholar | PubMed]
- 9.Thur CK, Edgren G, Jansson KÅ, Wretenberg P. Epidemiology of adult ankle fractures in Sweden between 1987 and 2004: A population-based study of 91,410 Swedish inpatients. Acta Orthop 2012;83:276-81. [Google Scholar | PubMed]
- 10.Georgiannos D, Lampridis V, Bisbinas I. Fragility fractures of the ankle in the elderly: Open reduction and internal fixation versus tibio-talo-calcaneal nailing: Short-term results of a prospective randomized-controlled study. Injury 2017;48:519-24. [Google Scholar | PubMed]
- 11.Tan YY, Nambiar M, Onggo JR, Hickey BA, Babazadeh S, Tay WH, et al. Tibio-talar-calcaneal nail fixation for ankle fractures: A systematic review and meta-analysis. J Foot Ankle Surg 2022;61:1325-33. [Google Scholar | PubMed]
- 12.Al-Nammari SS, Dawson-Bowling S, Amin A, Nielsen D. Fragility fractures of the ankle in the frail elderly patient: Treatment with a long calcaneotalotibial nail. Bone Joint J 2014;96:817-22. [Google Scholar | PubMed]
- 13.Childress HM. Vertical transarticular pin fixation for unstable ankle fractures: Impressions after 16 years of experience. Clin Orthop Relat Res 1976;120:164-71. [Google Scholar | PubMed]
- 14.Lemon M, Somayaji HS, Khaleel A, Elliott DS. Fragility fractures of the ankle: Stabilisation with an expandable calcaneotalotibial nail. J Bone Joint Surg Br 2005;87:809-13. [Google Scholar | PubMed]
- 15.Culpan P, Le Strat V, Piriou P, Judet T. Arthrodesis after failed total ankle replacement. J Bone Joint Surg Br 2007;89:1178-83. . [Google Scholar | PubMed]
- 16.Houshian S, Bajaj SK, Mohammed AM. Salvage of osteoporotic ankle fractures after failed primary fixation with an ankle arthrodesis nail: A report on four cases. Injury 2006;37:791-4. [Google Scholar | PubMed]
- 17.Buckingham RA, Hepple S, Winson IG. Outcome of ankle fractures in the elderly. Foot Ankle Surg 2000;6:175-8 [Google Scholar | PubMed]