In this case series of five patients, we used intra-articular dexamethasone in patients suffering from cervicogenic headache secondary to cervical trauma or rheumatoid arthritis involvement of the atlantoaxial joint.
Dr. Rampal Singh, Department Anaesthesiology, 4th Floor A-Block OT Complex, All India Institute of Medical Sciences, GE Road, Tati Bandh, Raipur - 492099, Chhattisgarh, India. E-mail: lautikasingh@gmail.com
Introduction: The International Headache Society divides headaches into primary (vascular and muscular) and secondary (inflammatory). Secondary headaches include headaches secondary to inflammation caused by injuries to the head and neck. Cervicogenic headache (CGH) is thought to be referred pain arising from irritation caused by cervical structures innervated by spinal nerves C1, C2, and C3; therefore, any structure innervated by the C1–C3 spinal nerves could be the source of a CGH. Pain from the lateral atlanto-axial joint (AAJ) is one of several causes of CGH. The pain is perceived in the upper neck and can be referred to the occiput, ear, vertex, and forehead.
Case Report: Patients who attended our pain clinic were presented with complaints of pain in the upper cervical, occipital, and sometimes periorbital and retro-orbital area and around the post-auricular area. On the numerical rating pain scale, patients had pain score of 8–9/10. Three patients had a history of trauma to the cervical region and 2 had a history of rheumatoid arthritis (RA). Patients suffering from RA also had pain in bilateral wrist joints along with neck pain. On examination, there was tenderness along the facet joint line on both sides, when the site of maximum tenderness was checked under the C-Arm machine, it was found at the AAJ on both sides. Patients having a history of trauma first had conservative treatment with analgesics while rheumatoid patients with analgesics and disease-modifying anti-rheumatoid drugs. When patients had no satisfactory pain relief with conservative treatment then patients were considered for fluoroscopy (C-Arm) and 0.5–1 mL Iohexol 300 guided AAJ steroid injection with dexamethasone. After steroid injection, all patients had good-to-excellent results and were followed up for 4 months. Trauma patients got complete relief whereas patients having a history of RA had only mild pain.
Conclusion: AAJ steroid injection with dexamethasone is an effective pain-relieving procedure for acute pain relief in patients having severe pain due to cervical trauma or due to RA involving AAJ.
Keywords: Atlantoaxial steroid injection, cervical trauma, headache, cervicogenic headache, occipital headache and neck pain.
The International Headache Society divides headaches into primary (vascular and muscular) and secondary (inflammatory). Cluster and migraine headaches have been included under the category of vascular while tension-type headaches as the muscular origin of primary headaches. In contrast, secondary headaches include headaches secondary to inflammation caused by injuries to the head and neck [1]. In 1983, Norwegian physician Sjaastad et al. coined the term, “cervicogenic headache” (CGH) by recognising a sub-group of headache patients with simultaneous head and neck pain; therefore, CGH is considered “secondary headaches [2].” Globally, headache disorders affect approximately 40%–52.0% [3, 4] of the population, or 3.1 billion people in 2021, and are more common in females compared to males [3]. In India, a 1-year study found, 63.9% of people had a headache, with women being more likely to experience headaches than men [5]. A CGH is a rare chronic headache most common in people 30–44 years old. Its prevalence among patients with headaches is 0.4%–4% [6]. CGH is thought to be referred pain arising from irritation caused by cervical structures innervated by spinal nerves C1, C2, and C3; therefore, any structure innervated by the C1–C3 spinal nerves could be the source of a CGH [7-9]. Pain from the lateral atlantoaxial joint (AAJ) is one of the several causes of CGH [8, 10]. The pain is perceived in the upper neck and can be referred to the occiput, ear, vertex, and forehead [11]. The innervation of the AAJ is primarily by the branches of the second cervical spinal nerve [12]. There are some common causes of AAJ dysfunction which include trauma, congenital (down syndrome, skeletal dysplasia, and congenital abnormalities) and inflammatory conditions like rheumatoid arthritis (RA) [13]. Rheumatoid primarily affects small peripheral joints, but the second most commonly involved region is the cervical spine [14,15]. There is a highly different prevalence of cervical spine involvement is reported in RA patients, ranging between 25 and 88% [16]. Patients presenting with atlantoaxial instability can suffer from a spectrum of clinical signs and symptoms [17] such as neck pain, restricted neck movements, pyramidal signs and myelopathy, lower cranial nerve palsies, respiratory failure, vertebral artery dissection, quadriplegia, and even death [18] has been documented. We encountered 5 patients in our pain clinic suffering from neck pain and limited joint mobility to some extent. Two of them had a history of RA and the rest of the three had a history of trauma.
Case 1
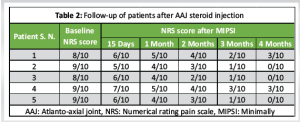
A 55-year-old male patient attended our pain clinic with complaints of headache, and bilateral neck pain (upper cervical region), occipital region, parietal and periorbital region in the month of mid-August 2022. He also complained of joint pain in the wrist, metacarpophalangeal and proximal interphalangeal joints for 2½ years. Pain usually increases with rest and decreases with physical activity with morning stiffness (30–45 min). Stiffness usually subsides after physical activity. The patient had an irregular history of treatment and was on paracetamol 650 mg on a need basis and methyl-prednisolone (Tablet Medrol 4 mg twice a day) (Table 1). He was receiving treatment from a local doctor and went to a physician only once or twice and there was no record of any treatment except current treatment. Blood investigations were done after physical examination (Table 2). The patient was followed up at 15 days, 1, 2, 3, and 4 months to analyse the pain using the numerical rating pain scale (NRS) (Table 3).
Case 2
A 40-year-old female patient attended our pain clinic in the month of late October 2022 with complaints of pain at the base of the neck and occiput referring to the vertex, parietal and periorbital area on both sides for 2 years. The patient said that she wakes up fresh in the morning but as the day passes pain intensity increases. The patient had a history of sudden jerks when riding on the bike (Table 1). On examination, there was tenderness over the area at the base of the neck on both sides. Her side-to-side neck movements were restricted. When tenderness was confirmed under a fluoroscope, the area corresponded to the atlanto occipital joint on both sides. All necessary blood investigations were done (Table 2) and the patient was followed up for 15 days, 1, 2, 3, and 4 months for analysing pain by NRS (Table 3).
Case 3
A 25-year-old male patient presented to our pain clinic with chief complaints of pain in the upper cervical region to the middle of the neck for 2 years in the month of mid-December 2022. Laterally, it referred to the retro-auricular area on both sides and anteriorly to the frontal, retro and peri-orbital area (Table 1). The pain was aggravated by side-to-side movement with restricted neck movement to some degree. Pain was dull aching and continuous, usually relieved by taking analgesic medications. As told by the patient he was not on contentious medication and visited the physician once or twice. After that, he was taking medication on a need basis. When his pain was not relived then some other patient referred him to us. After physical examination, the patient was advised for relevant haematological investigations (Table 2) and after completion of procedure patient was regularly followed up first at 15 days and then every month for 4 months for evaluation his pain by NRS score (Table 3).
Case 4
A 45-year-old female patient attended our pain clinic in the month of starting of February 2023 with chief complaints of pain in the upper cervical area extending to bilateral auricular areas, suboccipital, vertex, frontal, periorbital and retro-orbital areas on both sides for the last 3 years. The pain was aggravated by side to side and flexion and extension movement of the head and change in weather (pain usually increased in cold weather and was relieved in the summer season). As told by her, there was morning stiffness for 30–45 min in the neck which was slowly relieved by body warming with light exercises, physical activities, and daily routine activities. Along with neck pain, the patient also had pain in her wrist, metacarpophalangeal and proximal interphalangeal joints. The patient was taking acetaminophen (650 mg) and hydroxychloroquine (HCQS) 200 mg twice a day (Table 1). She was not on regular medication and had on and off medication history as told by an attendant. During history taking, she said that her mother is suffering from RA (in local language called as Gathia). After taking history and physical examination diagnosis of RA was made which was confirmed by investigations (Table 2). The patient had regular follow-up first at 15 days and then every month till 4 months to evaluate her pain by NRS (Table 3).
Case 5
A young boy 35-year-old male patient presented to us in mid of July 2023 with chief complaints of pain in the upper region of the neck, and headache with frontal and peri-orbital areas on both sides of the face and bilateral peri and retro auricular area (Table 1). As told by the patient, he had a jerk in his neck when sudden breaks were applied to the bike. He took treatment from a local doctor. Pain was relieved for some time but again occurred. As he said that he took treatment for at least 1 year but his pain was not relieved. After that, he took over-the-counter analgesics. The pain was continuous, dull, and achy in the neck and suboccipital region which increased with physical activities and was relieved with rest and painkillers. On physical examination, there was tenderness at the base of the neck at the level of both ears, and there were tender points at superior nuchal lines on both sides which were tender to touch. Side-to-side neck movements were restricted to some extent, but flexion and extension of the head were normal. After taking a proper history and doing a physical examination blood investigations were advised (Table 2). The patient had regular visit after having minimally invasive pain and spine intervention (MIPSI), AAJ steroid injection first at 15 days and then every month till 4 months for evaluation of her pain by numerical rating pain score scale (Table 3). In patients, suffering from RA, the diagnosis was made with proper history, physical examination, and investigation. The patients were switched over to disease-modifying anti-rheumatoid (DMARD) drugs like methotrexate (MTX, 7.5 mg once a week), Folic acid 5 mg 1 day after MTX, HCQS 200 mg twice a day along with non-steroidal anti-inflammatory drugs (NSAIDs)/acetaminophen. Disease-modifying drugs were only started after getting the baseline value of the liver function test and found within the normal range (Patient no. 1 and 4). All the patients received MIPSI (Minimally Invasive Pain and Spine Intervention) procedure after receiving conservative treatment for a certain period. Patients were followed up for 3–4 months after MIPSI.
Method of AAJ injection
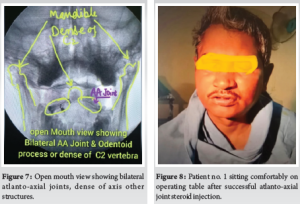
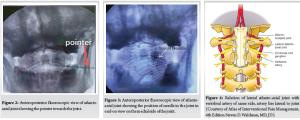
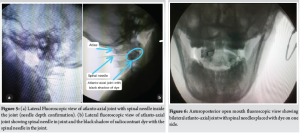
The night before the procedure patients were advised nil by mouth for 6 hours for solid, 3 hours for clear fluid and 0.5 mg of alprazolam in the bedtime 1/2 hour before meal and at 6:00 am with sips of water to decrease anxiety. In the morning patients were shifted to the operation theatre and allowed to lie down on the C-arm compatible operation table. All necessary monitors such as 12 lead ECG (electrocardiogram) electrodes, heart rate, pulse oximetry (SpO2), and temperature were attached to the patients. A twenty-gauge intravenous cannula was inserted into a nondominant hand to deal with any emergency and maintenance (per hour fluid requirement, mL/hour) of fluid usually Ringer’s Lactate based on the Holliday Segar formula. After this, patients were allowed to lie prone on the operation table with one pillow under the chest and one head ring under the forehead. Patients were advised to shave their hairs over the occiput and upper neck corresponding to the site of interest (Figure. 1). Patients received oxygen (1–2 L/min) by nasal cannula attached near the external nares. Under all aseptic precautions painting with chlorhexidine solution, sprit and 5% betadine (allowed to dry) and draping, fluoroscopic scanning was done in anteroposterior and lateral view, and the area of interest was marked. The skin was anaesthetised with 1–2 mL of 2% lignocaine without adrenaline. After 2–3 min a 22 G spinal needle was inserted under C-Arm guidance toward the AAJ (Figure. 2 and 3). At the level of the AAJ vertebral artery lies laterally and medially to the atlanto-occipital joint so we have to be the medial side of the AAJ (Figure. 3 and 4). The depth of the needle was confirmed in the lateral position at frequent intervals. As the joint is small, some manipulation was needed to go inside the joint. As soon as the needle penetrated the joint capsule, a pop was felt and depth of needle confirmed in lateral fluoroscopic view (Figure. 5a). After confirming needle position in anteroposterior (Figure. 1b, 3 and 6) and lateral fluoroscopic view, 0.5–1 mL of iohexol 300 was injected into the joint capsule and again confirmed with anteroposterior (Figures. 1b, 3, 6) and lateral fluoroscopic views (Figure 1b and c, 5b and 6). After confirmation of the intra-articular position of the needle in anteroposterior and lateral view, dye was aspirated and 0.5–1 mL (2–4 mg) of dexamethasone (non-particulate steroid) was injected with desired volume which could be accommodated easily without any force. The same procedure was repeated on the other side if needed. To perform an AAJ steroid injection, the patient has to be prone on the fluoroscopy-compatible operation table (Figure. 1a), and while doing the procedure he or she is advised to open-mouth to view the joint (open mouth view) (Figure. 7). Patients received light sedation with 1 mg of Midazolam by intravenous route. All types of equipment and drugs were kept ready to deal with any emergency during or after the procedure. Drugs that were used, were tested for skin sensitivity. Half an hour before procedure, patients received injectable antibiotics like ceftriaxone 1 g (after skin testing). Throughout the procedure, patients were monitored and continuously conversed and none of the patients had any adverse event during or after the procedure. Patients were comfortable after the procedure (Fig. 8). After the procedure patients were monitored in the post-procedure room for at least 2 h.
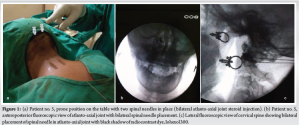
Brain parenchyma does not have nociceptors, and headache is typically the result of pain originating in surrounding structures, such as blood vessels, meninges, muscle fibres, facial structures, and cranial or spinal nerves. It has been suggested that stretching, dilatation, constriction, or any nociceptor stimulation within these structures can result in the perception of headache [19]. Globally, headache affects around 40–52% of the general population among which CGH though carries a small percentage (0.4–4%) [5], the important cause, which is a secondary type of headache [1]. Common causes of AAJ dysfunction include high-energy trauma such as motor vehicle accidents [13], spontaneous hyperaemic dislocation, nasopharyngeal torticollis, also known as Grisel syndrome, RA, trisomy 21, Morquio syndrome, and Marfan syndrome [20, 21]. In our case series, we also had 3 patients with a history of cervical trauma (Patients no. 2, 3, and 5) and 2 patients with a history of RA. Patients usually present with pain in the upper cervical neck commonly unilateral [22, 23] but we found bilateral in our patients as we had two patients suffering from RA. Pain occurs in the occipital, parietal skull and sometimes even to the eye of the involved side, with audible crepitation with head rotation [24, 25] and around the ear. Limited range of motion is due to spasm in the neck muscles, especially in the plane of C1-C2 [24, 26] as we also encountered in patients who attended our pain clinic. Pain is usually over the occipital region but it may refer to the parietal and frontal region of the skull and to the periauricular laterally. As we found in our patients, this may be due to the development of trigger points [27] in the muscles around the joint and their referred pain to other areas such as parietal, frontal, and periorbital areas. Another mechanism responsible for referred pain is spasms of muscles that lead to compression of nerves passing between muscle planes [28]. Many treatment options have been described in literature such as physical therapy, cervical traction, NSAIDs, trigger point injections, activity modification, and massage therapy [29]. Many authors have described surgical C1-C2 trans articular screw fixation and arthrodesis (for pain relief in pain and CGH) of AAJ damage due to different causes [27, 29-31]. RA and trauma patients who attended to us had inflammatory changes and RA patients did not have secondary arthritis changes. So, we decided to go for an intraarticular AAJ steroid (dexamethasone) injection. In a randomised control trial authors performed AAJ intra-articular 20 mg of triamcinolone injection and found a significant reduction (>50%) in the Visual Analog Score and overall neck disability index in patients receiving intraarticular injection as compared to systemic steroids (oral route) at 1, 2 and 3 months post-procedure [32]. Chevrot et al. found Cl-2 arthrography and intraarticular injection efficient and safe technique for the treatment of upper cervical pain due to Cl-2 articular disorders [33]. Although the above studies had been performed with triamcinolone (particulate steroid) we used dexamethasone (non-particulate steroid). In our case series, patients were followed up fortnightly and then monthly for 4 months. There was good pain relief at first follow-up in all patients including RA patients (Patients no. 1 and 4) and patients having a history of neck injury or trauma (Patients no. 2, 3 and 5) (NRS 5–7/10). All patients got even more relief and had NRS 4–5/10, 2–3/10, 1–2/10 and 0–2/10 at 1, 2, 3 and 4 months respectively. Patients having a history of trauma got almost complete pain relief (NRS 0/10) at 4 months but patients having RA had NRS of 2/10. The reason for incomplete pain relief in rheumatoid patients might be the inflammatory process in other cervical facet joints, intervertebral disc, vertebral end plates, and apophyseal joints [34] and the possibility of the presence of trigger points in the occipital or upper cervical region. CGH is usually a unilateral entity but in this case series, all patients had bilateral involvement. et al. described another type of bilateral pain disorder associated with head-and-neck pain, aggravated by neck positions and specific occupations [35].
CGH is a secondary type of headache, thought to be due to irritation caused by inflammation or trauma of cervical structures innervated by spinal nerves C1–C3. An inflammatory process like RA has a significant involvement of AAJ involvement and on the other hand cervical trauma makes joint prone to involvement. Both are significant causes of joint involvement, leading to CGH. Patients with acute pain not responding to conservative treatment with analgesics (in cervical trauma) and DMARD drugs benefit from AAJ steroid injection. C-Arm and radiocontrast guidance help in placing needle placement and exclusion of intravascular placement of needle tip. The vertebral artery lies lateral to the AAJ and variations in the positions of the vertebral artery are also present. Hence, one must have expertise before attempting intra-articular AAJ steroid injection.
CGH is an important clinical entity which disturbs a patient’s daily activity. AAJ inflammation either due to inflammatory disease or cervical trauma is important causes out of several. AAJ steroid injection provides good to excellent pain relief over conservative treatment when performed under fluoroscopy and radiocontrast guidance.
References
- 1.Headache Classification Subcommittee of the International Headache Society. The International classification of headache disorders: 2nd edition. Cephalalgia 2004;24:9-160. [Google Scholar]
- 2.Sjaastad O, Saunte C, Hovdahl H, Breivik H, Grønbaek E. “Cervicogenic” headache. An hypothesis. Cephalalgia 1983;3:249-56. [Google Scholar]
- 3.World Health Organization (WHO). Migraine and Other Headache Disorders: Migraine and Other Headache Disorders. Geneva, Switzerland: World Health Organisation; 2024. Available from: https://www.who.int/news-room/fact-sheets/detail/headache-disorders#:~:text=globally%2c%20headache%20disorders%20affect%20approximately,in%20females%20compared%20to%20males [Last accessed on 2024 Sep 23]. [Google Scholar]
- 4.Stovner LJ, Hagen K, Linde M, Steiner TJ. The global prevalence of headache: An update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain 2022;23:34. [Google Scholar]
- 5.Kulkarni GB, Rao GN, Gururaj G, Stovner LJ, Steiner TJ. Headache disorders and public ill-health in India: Prevalence estimates in Karnataka State. J Headache Pain 2015;16:67. [Google Scholar]
- 6.Al Khalili Y, Ly N, Murphy PB. Cervicogenic headache. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507862 [Last accessed on 2022 Oct 03]. [Google Scholar]
- 7.Silverberg ND, Martin P, Panenka WJ. Headache trigger sensitivity and avoidance after mild traumatic brain injury. J Neurotrauma 2019;36:1544-50. [Google Scholar]
- 8.Bogduk N, Govind J. Cervicogenic headache: An assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol 2009;8:959-68. [Google Scholar]
- 9.Lane R, Davies P. Post traumatic headache (PTH) in a cohort of UK compensation claimants. Cephalalgia 2019;39:641-7. [Google Scholar]
- 10.Govind J, Bogduk N. Sources of cervicogenic headache among the upper cervical synovial joints. Pain Med 2022;23:1059-65. [Google Scholar]
- 11.Cooper G, Bailey B, Bogduk N. Cervical zygapophysial joint pain maps. Pain Med 2007;8:344-53. [Google Scholar]
- 12.Forbes J, Das JM. Anatomy, head and neck: Atlantoaxial joint. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563271 [Last accessed on 2023 Aug 28]. [Google Scholar]
- 13.Lacy J, Bajaj J, Gillis CC. Atlantoaxial instability. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519563 [Last accessed on 2023 Jun 12]. [Google Scholar]
- 14.Gillick JL, Wainwright J, Das K. Rheumatoid arthritis and the cervical spine: A review on the role of surgery. Int J Rheumatol 2015;2015:252456. [Google Scholar]
- 15.Drosos AA, Pelechas E, Georgiadis AN, Voulgari PV. A not-to-miss cause of severe cervical spine pain in a patient with rheumatoid arthritis: A case-based review. Mediterr J Rheumatol 2021;32:256-63. [Google Scholar]
- 16.Di Muzio C, Conforti A, Bruno F, Currado D, Berardicurti O, Navarini L, et al. The assessment of atlantoaxial joint involvement in patients with rheumatoid arthritis, results from an observational “real-life” study. Sci Rep 2023;13:20146. [Google Scholar]
- 17.Lyons C, Ross M, Elliott R, Tall M. Atlantoaxial instability in a patient with neck pain and ankylosing spondylitis. Mil Med 2018;183:e654-7. [Google Scholar]
- 18.Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang S, Passias PG. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J 2014;4:197-210. [Google Scholar]
- 19.Gaul C, Meßlinger K, Holle-Lee D, Neeb L. Pathophysiology of headaches. Dtsch Med Wochenschr 2017;142:402-8. [Google Scholar]
- 20.Lisitskiy IY, Kiselev AM, Kiselev SE. Rheumatoid atlanto-axial dislocation: A surgical approach. Zh Vopr Neirokhir Im N N Burdenko 2018;82:41-7. [Google Scholar]
- 21.Allegrini D, Autelitano A, Nocerino E, Fogagnolo P, De Cillà S, Rossetti L. Grisel’s syndrome, a rare cause of anomalous head posture in children: A case report. BMC Ophthalmol 2016;16:21. [Google Scholar]
- 22.Betsch MW, Blizzard SR, Shinseki MS, Yoo JU. Prevalence of degenerative changes of the atlanto-axial joints. Spine J 2015;15:275-80. [Google Scholar]
- 23.Badve SA, Bhojraj S, Nene A, Raut A, Ramakanthan R. Occipito-atlanto-axial osteoarthritis: A cross sectional clinico-radiological prevalence study in high risk and general population. Spine (Phila Pa 1976) 2010;35:434-8. [Google Scholar]
- 24.Yu H, Hou S, Wu W, He X. Upper cervical manipulation combined with mobilization for the treatment of atlantoaxial osteoarthritis: A report of 10 cases. J Manipulative Physiol Ther 2011;34:131-7. [Google Scholar]
- 25.Schaeren S, Jeanneret B. Atlantoaxial osteoarthritis: Case series and review of the literature. Eur Spine J 2005;14:501-6. [Google Scholar]
- 26.Sutbeyaz ST, Sezer N, Koseoglu BF. The effect of pulsed electromagnetic fields in the treatment of cervical osteoarthritis: A randomized, double-blind, sham-controlled trial. Rheumatol Int 2006;26:320-4. [Google Scholar]
- 27.Page P. Cervicogenic headaches: An evidence-led approach to clinical management. Int J Sports Phys Ther 2011;6:254-66. [Google Scholar]
- 28.Florman JE, Cushing DA, England EC, White E. How to transect the C2 root for C1 lateral mass screw placement: Case series and review of an underappreciated variable in outcome. World Neurosurg 2019;127:e1210-4. [Google Scholar]
- 29.Neal MT, Gibbs W, Lyons MK. Atlantoaxial osteoarthritis: A well-established entity that remains frequently overlooked. Turk Neurosurg 2022;32:336-40. [Google Scholar]
- 30.Ferch RD, Zhang T, Bogduk N. Athrodesis of the lateral atlanto-axial joint for the relief of neck pain and cervicogenic headache. Pain Med 2024;25:203-10. [Google Scholar]
- 31.Tominaga H, MacDowall A, Olerud C. Surgical treatment of the severely damaged atlantoaxial joint with C1-C2 facet spacers: Three case reports. Medicine (Baltimore) 2019;98:e15827. [Google Scholar]
- 32.Hetta DF, Elawamy AM, Hassanein MM, Aljohi AS, Hasan RA, Mohammed NA, et al. Efficacy of atlantoaxial joint glucocorticoid injection in patients with rheumatoid arthritis: A randomized trial. Pain Physician 2019;22:E295-302. [Google Scholar]
- 33.Chevrot A, Cermakova E, Vallée C, Chancelier MD, Chemla N, Rousselin B, et al. C1-2 arthrography. Skeletal Radiol 1995;24:425-9. [Google Scholar]
- 34.Sharp J, Purser DW, Lawrence JS. Rheumatoid arthritis of the cervical spine in the adult. Ann Rheum Dis 1958;17:303-13. [Google Scholar]
- 35.Page P. Cervicogenic headaches: an evidence-led approach to clinical management. Int J Sports Phys Ther. 2011 Sep;6(3):254-66. PMID: 22034615; PMCID: PMC3201065. [Google Scholar]