Distal femur fracture fixation in today’s landscape has morphed into sophisticated procedures through nuanced procedural advancements and multifaceted approaches. Nail-plate combinations, dual-plate constructs, and distal femoral replacements are positioned to be front-runners in a market increasingly valuing precision and efficacy. Biological considerations in augmenting fixation are seemingly setting the direction for future trends to follow.
Dr. Rohan Jayaram, Department of Orthopaedics, Dr. D.Y. Patil Medical College and Hospital, Navi Mumbai, Maharashtra, India. E-mail: drrohanjayaram@gmail.com
Introduction: Recent advancements in the treatment of distal femoral fractures have significantly shifted toward more advanced fixation techniques and approaches. The variety of fracture patterns across different age groups complicates the establishment of a standardized treatment protocol upon presentation, thus making it difficult to establish defined protocols to follow in routine clinical practice.
Materials And Methods: This review analyzes existing literature and research studies on traditional methods, such as plating, intramedullary nailing, and distal femoral replacement, alongside emerging techniques, such as nail-plate combinations, dual-plate constructs, and non-conventional approaches in patients presenting with distal femoral fractures
Conclusion: A total of 3,880 patients treated for distal femoral fractures were included across 40 publications, aiming to provide a narrative of future management strategies that potentially end in significantly better outcomes.
Keywords: Distal femur fracture, nail plate combination, dual plate construct, distal femoral replacement, biologics, osteoporotic fractures.
Recent trends in the management of distal femoral fractures are shifting away from conventional practices as advancements in fixation and replacement procedures gain prominence. This shift reflects the growing preference among patients, especially within the geriatric demographic, for methods that promote faster recovery and reduce complications. A comprehensive analysis of 40 publications, encompassing 3,880 patients treated for distal femoral fractures with various modalities, was conducted to establish a guideline for future management techniques that incorporate minimally invasive smart implant technologies, showing superior outcomes.
Recent trends indicate several changes in the choice of modalities for treating distal femoral fractures:
- Closed reduction and internal fixation using intramedullary interlocking nailing have increased from 6.8% to 8.4% of fixations [1]
- Open reduction and internal fixation have declined from 89.9% to 76.6% [2]
- Distal femoral replacement has seen a notable rise from 3.3% to 14.9% [3].
These shifts highlight the preference for advanced fixation techniques and arthroplasty procedures, particularly in elderly patients with complex fracture patterns.
Retrograde intramedullary nailing (RIN)
Current studies comparing RIN with distal femoral plating indicate significant advantages for RIN, including faster union times and reduced post-operative infection rates. This explains the growing preference for RIN in suitable cases [4].
Nail-plate combinations
Geriatric distal femoral fractures are comparable to proximal femoral fractures, necessitating prompt surgical intervention with stable fixation that allows for immediate weight-bearing. Various fixation options are available, including limb plating (LP), rigid internal metallic nailing (rIMN), or a combination of implants such as nail plate (NP) or distal femur replacement. NP constructs combine the load-bearing and load-sharing capabilities of LP and rIMN, respectively, facilitating weight-bearing sooner and minimizing the risks of hardware failure and non-union. Though the current literature is limited, it suggests promising results for NP fixation in both native and periprosthetic fractures. In all instances, patients achieved bone union and were able to bear weight sooner than those undergoing standalone implant fixations. Geriatric, osteoporotic, and obese patients may particularly benefit from double implant fixation to promote early mobilization and reduce the risk of non-union. In addition, periprosthetic fractures, fractures with medial comminution, and those involving the metaphysis may indicate NP fixation suitability. Further research is needed to assess the cost implications of nail and plate fixation, while larger randomized controlled trials will provide definitive evidence for its superiority over other treatments [5,6] (Fig. 1).
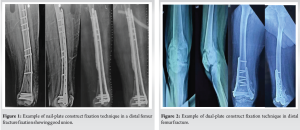
Dual-plate constructs
The double plate technique offers significant advantages in achieving reliable and rigid fixation, allowing for immediate weight bearing. This method mitigates the risk of fixation failure by preserving the neutral axis of the femur. Although preliminary studies have produced encouraging results, there remains a necessity for larger comparative studies, accompanied by supportive biomechanical and finite element analyses, to validate these findings [7] Fig. 2.
Distal femoral replacement
The distal femoral replacement has demonstrated beneficial evidence with favorable outcomes, particularly in elderly patients and cases involving complex fractures. When compared to surgical fixation and conservative management, distal femoral replacement is associated with shorter hospital stays and expedited functional recovery, alongside reduced rates of readmission. Notably, it exhibits similar mortality and reoperation rates as internal fixation methods. The distal femoral replacement may be more dependable in complex fracture patterns where achieving adequate fixation poses challenges [8-10] Fig. 3.

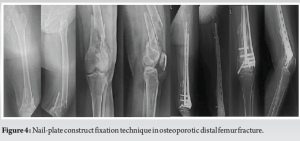
Ensuring stable internal fixation for fractures in the osteoporotic intra-articular distal femur is a challenging endeavor due to the presence of thin cortices, a wide medullary canal, diminished bone stock, and fracture comminution. Currently, no singular therapeutic approach has proven completely effective in addressing all facets of this injury. The integration of anatomical plates with locking mechanisms and intramedullary interlocking nailing appears promising for the secure stabilization and fixation of osteoporotic distal femur fractures, potentially facilitating a more rapid recovery process [11] Fig. 4.
Periprosthetic Fractures
Management of periprosthetic fractures presents significant challenges regarding planning, recovery, and the rate of complications. Treatment selection should be informed by patient age, fracture displacement and morphology, bone quality, overall health, and the status of the prosthetic components, whether loose, unstable, or misaligned. Operative treatment has been shown to provide superior results as a treatment modality. Prompt mobilization and post-operative physiotherapy are critical to the recovery process, aiding in functional restoration and minimizing complication risks. Continuous monitoring for potential complications is essential to facilitate timely interventions [12] Fig. 5 and 6.


The treatment of distal femoral non-unions necessitates a comprehensive metabolic and nutritional evaluation to identify modifiable systemic factors contributing to the initial non-union. Following identification, these deficiencies should be addressed. Allograft struts, whether employed intramedullary or as cortical onlay, play a crucial role in enhancing fixation around distal femoral non-unions. Furthermore, the use of autografts or allografts supplemented with osteoinductive agents, such as bone morphogenetic proteins or demineralized bone matrix, proves beneficial in fostering local union. Through extensive pre-operative assessment and meticulous operative techniques, including the utilization of osteobiologics, a majority of these patients can be effectively treated with a low incidence of conversion to distal femoral replacement [13] Fig. 7.

Minimally Invasive Approaches
The adoption of minimally invasive procedures is increasingly prominent in the management of distal femoral fractures. This approach aims to improve patient outcomes by addressing systemic health while ensuring stable fixation through minimized disruption of existing soft tissue conditions and simplified implant placement [14].
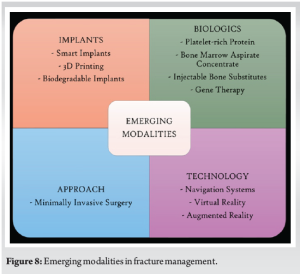
The future of advancements in implant technology may lie in the development of smart implants tailored for optimal clinical outcomes within the framework of precision medicine. The capacity to customize treatment options for individual patients, combined with real-time monitoring capabilities, heralds innovative approaches in fracture fixation management [15] Fig. 8.
The management of distal femur fractures is evolving toward a sophisticated, multifaceted approach characterized by nuanced procedural advancements. The emergence of nail-plate combinations, dual-plate constructs, and a growing emphasis on distal femoral replacement procedures position these modalities as front-runners in a market that increasingly values precision and efficacy. Furthermore, biological considerations are anticipated to influence future trends and inform the development of emerging markets forward.
Treatment selection in distal femur fractures should be uniquely tailored to each patient, depending on age, fracture displacement and morphology, bone quality, and their overall health status. Operative treatment often provides superior results. Prompt mobilization and post-operative physiotherapy are crucial to functional restoration, with concurrent monitoring for potential complications and facilitating timely interventions.
References
- 1.DeKeyser G, Thorne T, Martin BI, Haller JM. Changing epidemiology of distal femur fractures: Increase in geriatric fractures and rates of distal femur replacement. J Am Acad Orthop Surg 2024;32:e1289-98. [Google Scholar | PubMed]
- 2.Elsoe R, Ceccotti AA, Larsen P. Population-based epidemiology and incidence of distal femur fractures. Int Orthop 2018;42:191-6. [Google Scholar | PubMed]
- 3.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury 2006;37:691-7. [Google Scholar | PubMed]
- 4.Kim HS, Yoon YC, Lee SJ, Sim JA. Which fixation produces the best outcome for distal femoral fractures? Meta-analysis and systematic review of retrograde nailing versus distal femoral plating in 2432 patients and 33 studies. Eur J Trauma Emerg Surg 2024;50:763-80. [Google Scholar | PubMed]
- 5.Kontakis MG, Giannoudis PV. Nail plate combination in fractures of the distal femur in the elderly: A new paradigm for optimum fixation and early mobilization? Injury 2023;54:288-91. [Google Scholar | PubMed]
- 6.Pfister B, Wilson A, Drobetz H. Best of both worlds? Fixation of distal femur fractures with the nail-plate construct. Orthop Surg 2023;15:3326-34. [Google Scholar | PubMed]
- 7.Liporace FA, Aneja A, Carroll EA, Yoon RS. Maintaining the neutral axis in the treatment of distal femur fractures via dual plate or nail plate combination technique: When and How? J Orthop Trauma 2021;35 Suppl 5:S38-40. [Google Scholar | PubMed]
- 8.Routledge JC, Bashir O, Elbeshbeshy M, Saber AY, Aqil A. Management of distal femur fractures: Replacement versus surgical fixation versus conservative management. Cureus 2023;15:e45333. [Google Scholar | PubMed]
- 9.Garabano G, Pereira S, Juri A, Bidolegui F, Pesciallo CA. Distal femur fractures in elderly treated with internal fixation or distal femoral replacement - retrospective cohort study on 75 patients assessing functional outcomes, reoperations, and mortality. Eur J Orthop Surg Traumatol 2024;34:3775-82. [Google Scholar | PubMed]
- 10.Lex JR, Di Michele J, Sepehri A, Chuang TC, Backstein DJ, Kreder HJ. Distal femoral replacement or internal fixation for management of periprosthetic distal femur fractures: A systematic review. Knee 2022;37:121-3. [Google Scholar | PubMed]
- 11.Kale S, Dhar S, Chaudhari P, Mehta N, Das S, Modi R Integrated nail and plate fixation with allograft in the management of osteoporotic intra-articular distal femur fracture - A case report. J Orthop Case Rep 2024;14:93-7. [Google Scholar | PubMed]
- 12.Thukral R, Marya S, Singh C. Management of distal femoral periprosthetic fractures by distal femoral locking plate: A retrospective study. Indian J Orthop 2015;49:199-207. [Google Scholar | PubMed]
- 13.Nauth A, Haller J, Augat P, Anderson DD, McKee MD, Shearer D, et al. Distal femur fractures: Basic science and international perspectives. OTA Int 2024;7 2 Suppl:e320. [Google Scholar | PubMed]
- 14.Nester M, Borrelli J Jr. Distal femur fractures management and evolution in the last century. Int Orthop 2023;47:2125-35. [Google Scholar | PubMed]
- 15.Babhulkar S, Trikha V, Babhulkar S, Gavaskar AS. Current concepts in management of distal femur fractures. Injury 2024;55 Suppl 2:111357. [Google Scholar | PubMed]











