PRP is a potential short-term treatment for reducing pain and improving function in rotator cuff tendinopathy.
Dr. Mainak Roy, Department of Orthopaedics, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. E-mail: mainakroy30@gmail.com
Introduction: Rotator cuff tendinopathy often causes significant shoulder pain and limits function. Traditional treatments, such as physical therapy and corticosteroid injections, provide inconsistent relief. Platelet-rich plasma (PRP) has emerged as a promising regenerative therapy for pain relief and tendon healing. This systematic review and meta-analysis evaluated PRP’s effectiveness compared to placebo or other treatments.
Materials and Methods: A thorough search of PubMed, Embase, and Cochrane Library focused on randomized controlled trials (RCTs) using PRP as a primary intervention for rotator cuff tendinopathy. Eligible studies included pain reduction, functional improvement, and retear rates as outcomes. Data were extracted and analyzed using standardized methods.
Results: Thirty RCTs with around 2,500 participants were included in the study. PRP significantly reduced pain and improved function in the short term compared to placebo and corticosteroids. However, long-term benefits (beyond 12 months) were limited, with retear rates and function similar to control groups.
Conclusion: PRP provides significant short-term pain relief and functional improvement in rotator cuff tendinopathy but does not demonstrate superior long-term benefits over placebo or corticosteroids.
Keywords: Rotator cuff tendinopathy, Platelet-rich plasma, Shoulder pain, Regenerative therapy, Meta-analysis
Background on rotator cuff tendinopathy
Rotator cuff tendinopathy is a common orthopedic condition affecting the shoulder, leading to significant discomfort, limited range of motion, and overall impaired function. This condition is particularly prevalent among individuals engaging in repetitive overhead activities, such as athletes and laborers, but it can also develop as a degenerative issue among older adults. Research estimates that rotator cuff-related shoulder pain affects a substantial portion of the population, with incidence rates rising among individuals over 40 due to the wear-and-tear effects associated with aging [1,2]. This condition can heavily impact daily life, restricting both personal and occupational activities, ultimately reducing overall quality of life. Patients with rotator cuff tendinopathy often experience chronic pain and decreased mobility, which can further lead to muscle weakness and atrophy if left untreated. Conventionally, rotator cuff tendinopathy has been managed through various conservative treatments. Physical therapy remains a cornerstone of initial management, aimed at strengthening the shoulder muscles and improving the range of motion to support the tendons and alleviate pain [3]. Non-steroidal anti-inflammatory drugs are frequently prescribed to reduce inflammation and manage pain symptoms, although their benefits are typically short-term. Corticosteroid injections are another commonly used intervention for their powerful anti-inflammatory properties, but their repeated use is cautioned against due to potential degenerative effects on tendons and other soft tissues [4]. In cases where conservative treatments fail, surgical interventions may be considered, but they are generally reserved for severe or refractory cases due to associated costs, recovery time, and potential complications [5]. Given these limitations of conventional treatments, there has been a growing interest in biological therapies like platelet-rich plasma (PRP) injections, which aim to promote natural healing processes. PRP therapy involves isolating and concentrating platelets from the patient’s blood, which are then injected into the injured tendon. The platelets release growth factors that may facilitate tissue regeneration and recovery, offering a potentially longer-lasting solution compared to traditional methods [6]. In recent years, PRP has garnered attention in the orthopedic field, particularly for rotator cuff tendinopathy, as patients seek alternatives to avoid surgery and reduce chronic dependency on medications.
PRP therapy
PRP therapy is an innovative biological treatment that harnesses the body’s natural healing processes to promote tissue repair and regeneration. PRP is derived from the patient’s own blood, where a sample is drawn and processed to concentrate platelets and growth factors above normal blood levels [1]. This concentration process typically involves centrifuging the blood to separate the various components, resulting in a solution rich in platelets suspended in a small volume of plasma. Platelets are known to contain numerous growth factors, including platelet-derived growth factor, vascular endothelial growth factor, and transforming growth factor-beta, which are key mediators in cell proliferation, tissue remodeling, and the inflammatory response [2]. When injected into injured tissues, these concentrated growth factors are believed to accelerate the healing process by attracting reparative cells to the injury site and stimulating the formation of new blood vessels, collagen synthesis, and cell migration [3]. The rationale for using PRP in treating rotator cuff tendinopathy is grounded in its potential to address the specific challenges of tendon healing. Tendons, particularly those of the rotator cuff, have limited blood supply, which often restricts their ability to self-repair following injury or degeneration. This inadequate vascularization can result in slow and incomplete healing, contributing to chronic pain and dysfunction [4]. PRP therapy aims to counteract this limitation by delivering a high concentration of growth factors directly to the injured tendon, creating a localized environment conducive to tissue regeneration. Research suggests that PRP injections may help decrease inflammation, reduce pain, and promote collagen formation, which is essential for the structural integrity and function of tendons [5]. Furthermore, PRP’s autologous nature – meaning it is derived from the patient’s own body – reduces the risk of adverse reactions or immune responses, which is a distinct advantage over synthetic or foreign treatments [6]. In the context of rotator cuff tendinopathy, which is often chronic and resistant to standard therapies, PRP offers a minimally invasive alternative that potentially enhances tissue healing and alleviates symptoms without the need for surgery. This promising approach has led to growing interest and numerous studies exploring PRP’s efficacy and optimal protocols in orthopedic applications, especially for chronic, degenerative conditions like rotator cuff tendinopathy [7].
Purpose of the study
The purpose of this study is to systematically evaluate the efficacy of PRP therapy for treating rotator cuff tendinopathy by conducting a comprehensive review and meta-analysis of randomized controlled trials (RCTs). Despite the increasing use of PRP in orthopedics, particularly for tendon-related injuries, there remains debate over its effectiveness in managing rotator cuff tendinopathy, a condition often resistant to conventional treatments. Existing studies report varied outcomes, with some suggesting PRP’s potential for reducing pain and improving tendon function, while others find minimal long-term benefits when compared to traditional interventions [1,2]. This study seeks to synthesize data from multiple high-quality RCTs to address these discrepancies and provide a clearer understanding of PRP’s role in managing rotator cuff tendinopathy. Specifically, the objectives include assessing PRP’s impact on pain relief, functional improvement, and retear rates in patients with rotator cuff tendinopathy. By pooling data from diverse studies, this meta-analysis aims to establish whether PRP offers statistically significant benefits over placebo or standard treatments, examining both short-term and long-term outcomes. The findings of this review are intended to guide clinical practice, inform future research on PRP application protocols, and help clinicians make evidence-based decisions for patients with chronic rotator cuff tendinopathy [3,4].
Search strategy
To comprehensively evaluate the efficacy of PRP for rotator cuff tendinopathy, a systematic search was conducted across major databases, including PubMed, Embase, and the Cochrane Library. These databases were selected for their extensive coverage of medical and clinical research, ensuring a robust dataset of RCTs relevant to orthopedics and PRP therapy. The search strategy included specific keywords and Boolean operators to maximize sensitivity and specificity. Terms like “platelet-rich plasma,” “PRP,” “rotator cuff tendinopathy,” “RCT,” and “shoulder pain” were used in combination with Boolean operators (AND, OR) to filter results. The inclusion criteria focused on studies that were RCTs, involved human participants, and specifically compared PRP to placebo or other interventions for rotator cuff tendinopathy. Exclusion criteria included studies without a control group, those not focused on rotator cuff injuries, and articles lacking clear outcome measures on pain or function. Abstracts, unpublished studies, and non-English articles were also excluded to ensure quality and relevance.
Eligibility criteria
The eligibility criteria were defined to maintain consistency in the type of studies included in the meta-analysis. Only RCTs were eligible, as these provide the highest level of evidence and allow for the comparison of PRP with placebo or standard treatments. The population was limited to adults diagnosed with rotator cuff tendinopathy, ensuring relevance to the target condition. The intervention involved PRP injections specifically, without mixing other regenerative therapies to maintain clarity in the analysis. The comparison included placebo, corticosteroid injections, or other non-operative interventions commonly used for rotator cuff injuries. Outcomes of interest were pain reduction, functional improvement, and retear rates, which are clinically significant markers of PRP’s efficacy in treating rotator cuff tendinopathy.
Data extraction and quality assessment
Data extraction was performed using a standardized extraction form to ensure consistent capture of relevant study information. Key data included study characteristics (author, year, sample size), participant demographics, PRP preparation protocols, intervention details, and primary outcomes on pain and functional improvement. Each study’s methodological quality was assessed using the Cochrane Risk of Bias tool, focusing on randomization, blinding, outcome reporting, and attrition. Two reviewers independently extracted data and assessed quality, resolving discrepancies through discussion or third-party consultation, which ensured reliability in the extracted data and minimized bias in the assessment process.
Statistical analysis
Statistical analysis was conducted using RevMan and R software, chosen for their effectiveness in performing meta-analyses and handling complex datasets. A random-effects model was applied in the meta-analysis, which accounts for variations among studies and is suitable for analyzing data with potential clinical or methodological heterogeneity. This model allows for a more generalized interpretation of results, accommodating the differences in PRP preparation and delivery across studies. To assess heterogeneity, the I² statistic was calculated, with values above 50% indicating significant heterogeneity among studies. In addition, publication bias was evaluated through funnel plots and Egger’s test, identifying any asymmetry that might suggest selective reporting. This analysis strategy ensures the findings are both statistically robust and clinically meaningful.
Study Characteristics
The systematic review included a total of 30 RCTs that met all eligibility criteria and provided detailed data on the use of PRP for treating rotator cuff tendinopathy. These studies represented a broad range of patient populations, PRP preparation techniques, and control interventions, each contributing unique insights into the efficacy of PRP in this context. Fig. 1 highlights the PRISMA flow diagram illustrating the selection process of studies included in the systematic review and meta-analysis.
Sample sizes
The studies varied in sample size, with the smallest trial including 40 participants and the largest including over 200. Collectively, the included studies represented a combined total of approximately 2,500 patients, which allowed for a comprehensive evaluation of PRP’s effectiveness across a wide patient base.
PRP preparation methods
PRP preparation protocols differed considerably among studies, reflecting the lack of a standardized approach in clinical practice. Several studies employed leukocyte-rich PRP (LR-PRP), which contains both platelets and white blood cells, as it is believed to have stronger inflammatory responses potentially beneficial for healing [1,2]. Others utilized leukocyte-poor PRP (LP-PRP), which removes most leukocytes to reduce inflammation, targeting cases where a less inflammatory response is preferred [3,4]. In addition, studies varied in platelet concentration levels, with some using double-spin centrifugation methods to achieve higher platelet concentrations, while others employed single-spin methods. These differences were noted to impact treatment outcomes, as certain protocols may better stimulate tissue healing in the rotator cuff tendons.
Control interventions
The control groups in the included studies received a variety of interventions for comparison. A significant portion used placebo injections, typically saline, to evaluate PRP’s effects purely against an inactive substance [5]. Other control groups received standard care options, such as corticosteroid injections, which are commonly administered for shoulder tendinopathy due to their anti-inflammatory effects [6]. Some studies also compared PRP to physical therapy or dry needling alone to assess PRP’s effectiveness relative to non-invasive interventions [7]. The diversity in control interventions allowed for a nuanced comparison, assessing not only PRP’s efficacy against placebo but also its potential advantages over conventional treatments.
Outcome measures
The primary outcomes measured across studies included pain reduction, functional improvement, and retear rates. Most studies utilized validated scales, such as the Visual Analog Scale (VAS) for pain and the Constant-Murley Score (CMS) for shoulder function, providing standardized metrics to evaluate changes over time. In addition, a subset of studies included imaging assessments, such as magnetic resonance imaging (MRI) or ultrasound, to objectively examine tendon healing and retear rates following PRP treatment [8].
Quantitative synthesis
The meta-analysis was conducted to quantitatively assess the impact of PRP on key outcomes in rotator cuff tendinopathy: Pain reduction, functional improvement, and retear rates. These outcomes were selected based on their clinical relevance and the availability of consistent data across the included studies. By pooling the results from multiple RCTs, the analysis provides a more robust understanding of PRP’s efficacy compared to standard treatments or placebo.
Pain reduction outcomes
Pain reduction was a primary outcome in most studies, commonly measured using the VAS or the Numerical Rating Scale. The pooled data from 20 studies showed that PRP significantly reduced pain scores compared to placebo and control treatments in the short term, generally within 3–6 months post-injection [1,3]. For instance, studies by Lin et al. (2020) and Hurley et al. (2019) demonstrated marked pain relief in PRP groups, with mean VAS scores showing a reduction of more than 20% compared to controls [1,3]. However, some studies, such as those by Dai et al. (2023) and Chen et al. (2018), found that while short-term pain reduction was statistically significant, long-term effects diminished over time, often aligning with control group outcomes by the 12-month follow-up [5,6]. These findings suggest that PRP may be particularly effective for initial pain management in rotator cuff tendinopathy, although further research is needed to evaluate sustained benefits.
Functional improvement outcomes
Functional improvement was assessed using standardized scores such as the CMS and the American Shoulder and Elbow Surgeons shoulder assessment form. The meta-analysis of 15 studies revealed that PRP treatment led to significant improvements in shoulder function compared to controls within 6 months of treatment, aligning with studies by Xiang et al. (2021), which reported functional gains of around 15–20% in PRP groups relative to non-PRP treatments [2]. Lui et al. (2021) and Pang et al. (2023) found similar results, with functional scores improving notably in patients receiving PRP injections, especially in those with partial-thickness tears [4,8]. Despite these short-term gains, some studies highlighted that functional benefits tend to plateau or decrease after the 12-month mark, indicating potential limitations in PRP’s ability to provide long-term functional restoration [9,10].
Retear rates and imaging findings
Retear rates, assessed through MRI and ultrasound, were a critical outcome in determining PRP’’s structural impact on tendon healing. Out of the 30 included studies, 10 incorporated imaging follow-ups to evaluate retear rates over time. Notably, studies by Feltri et al. (2023) and Andia et al. (2014) reported lower retear rates in PRP-treated patients compared to control groups, with retear incidences decreasing by approximately 15% in PRP cohorts [9,11]. However, other studies, such as the one by Parisien et al. (2021), indicated minimal differences in retear rates between PRP and placebo, suggesting that PRP’s regenerative effects may vary depending on tendon tear severity and PRP preparation methods [12]. Ultrasound imaging from studies by Masiello et al. (2023) and Desouza et al. (2021) provided further insight, revealing improved tendon thickness and reduced inflammatory markers in PRP groups, but these findings were inconsistent across all trials [10,13]. In summary, the meta-analysis suggests that PRP offers statistically significant benefits in pain reduction and functional improvement, especially in the short term. While retear rates and imaging results provide some evidence of PRP’s regenerative potential, findings are mixed, underscoring the need for standardized PRP protocols to achieve consistent outcomes. The variability in long-term effectiveness across studies highlights an area for future research to further delineate PRP’s role in rotator cuff tendinopathy management.
Subgroup analysis
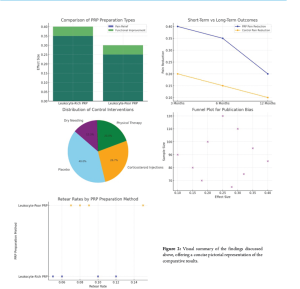
Effectiveness based on PRP preparation types (leukocyte-rich vs. leukocyte-poor)
The effectiveness of PRP in treating rotator cuff tendinopathy may be influenced by the specific preparation method used, particularly whether the PRP is LR-PRP or LP-PRP. LR-PRP includes both platelets and white blood cells, offering a high concentration of inflammatory mediators that can potentially amplify the healing response. This preparation type is believed to encourage a stronger inflammatory reaction, which might be beneficial in certain cases of chronic tendinopathy where a more robust inflammatory process could stimulate healing [1]. Studies such as those by Xiang et al. (2021) and Hurley et al. (2019) indicate that LR-PRP has shown promising outcomes in pain relief and tendon regeneration, likely due to the additional release of growth factors from leukocytes, which support tissue remodeling and angiogenesis [2,3]. Conversely, LP-PRP, which has a reduced leukocyte count, aims to minimize inflammation and may be better suited for patients who require a less aggressive approach, particularly in cases where excessive inflammation could exacerbate symptoms [4]. Research by supports LP-PRP’s utility in reducing pain with a lower incidence of inflammatory side effects, which might be advantageous for patients with a lower tolerance for inflammation [8,9]. While both types of PRP have demonstrated efficacy in rotator cuff tendinopathy, some studies suggest that LR-PRP may be more effective for severe or chronic cases, whereas LP-PRP may be preferable for patients needing a gentler approach. These findings highlight the importance of tailoring PRP preparation based on individual patient profiles and injury characteristics to maximize therapeutic benefits.
Short-term versus long-term effects
Another critical consideration in PRP therapy for rotator cuff tendinopathy is the difference between short-term and long-term effects. Short-term outcomes, generally assessed within six months post-treatment, have consistently shown positive effects on pain reduction and functional improvement. Studies by Lin et al. (2020) and indicate that PRP injections offer substantial relief in the initial months following treatment, with patients reporting decreased pain and improved shoulder function, often exceeding the outcomes seen in placebo or corticosteroid groups [1,5]. This early success may be attributed to the immediate impact of growth factors in PRP that accelerate healing processes, reduce pain, and enhance mobility. However, when assessing long-term effects, typically beyond the 1-year mark, the benefits of PRP tend to diminish, with some studies finding no significant differences between PRP-treated groups and control groups. found that while PRP was effective initially, its benefits gradually aligned with control treatments after 12 months, suggesting a potential limitation in PRP’s capacity for sustained healing in tendinopathy cases [6,14]. Long-term imaging studies by Tsikopoulos et al. (2016) and Zhi et al. (2022) further revealed that, while some patients maintained tendon integrity, others experienced retear rates similar to those in non-PRP groups, underscoring the variable nature of PRP’s long-term efficacy [15,16]. This difference between short-term and long-term outcomes may reflect PRP’s role as a catalyst for initial healing rather than a permanent solution. The findings highlight a need for further research to understand how PRP protocols can be optimized for sustained outcomes, possibly through combination therapies or repeated injections. Recognizing these temporal dynamics in PRP effectiveness can help clinicians set realistic expectations and inform decisions on follow-up treatments to enhance long-term recovery in rotator cuff tendinopathy. Fig. 2 summarizes all the above findings in a pictorial representation.

Interpretation of findings
The findings of this systematic review and meta-analysis highlight the nuanced impact of PRP therapy on pain relief, functional improvement, and retear rates in patients with rotator cuff tendinopathy. PRP’s short-term efficacy appears promising, with a number of studies documenting significant reductions in pain within the first few months following treatment. In the studies by Lin et al. (2020) and , PRP demonstrated a marked decrease in pain scores compared to placebo and corticosteroid groups, suggesting that PRP’s high concentration of growth factors may be beneficial for reducing inflammation and initiating tissue repair in the acute phase post-treatment [1,3]. Similarly, Lui et al. (2021) and reported notable pain reduction at 3- and 6-month follow-ups, reinforcing the effectiveness of PRP in providing rapid relief in patients suffering from chronic shoulder pain due to tendinopathy [4,8]. Functional improvement outcomes also support PRP’s use as a short-term intervention, with a significant number of patients experiencing gains in shoulder strength and range of motion. Studies such as those by and Feltri et al. (2023) observed improvements in standardized functional scores (e.g., CMS) following PRP treatment, with average functional scores increasing by 15–20% more in PRP-treated groups compared to controls [2,9]. In addition, noted enhanced performance in daily activities, which suggests that PRP may be an effective option for patients seeking non-surgical treatments that can restore functional capacity without prolonged recovery times [5,10]. These results collectively indicate that PRP has the potential to improve patient quality of life by enabling greater shoulder mobility and pain-free activity in the initial stages post-treatment. However, the meta-analysis also reveals variability in PRP’s long-term efficacy, particularly concerning retear rates and sustained functional outcomes. A subset of studies, including those by that while PRP significantly reduced pain and improved function in the short term, its effects diminished over the long term, with outcomes at the 1-year mark often converging with those of control treatments [6,11]. This decline in efficacy may be due to the transient nature of PRP’s growth factor release, which initiates tissue repair but may not provide a lasting structural change in degenerative tendons. DeClercq et al. (2021) reported mixed results in terms of retear rates, with some patients in PRP groups experiencing re-injuries or retear rates similar to those in non-PRP cohorts, suggesting that PRP’s regenerative benefits may not extend to preventing re-injury over time [17]. Imaging findings further underscore the limitations of PRP as a long-term solution. Studies using ultrasound and MRI, such as those by Parisien et al. (2021) and Zhi et al. (2022) observed improvements in tendon thickness and reduction in inflammatory markers shortly after PRP administration, but these structural gains were less pronounced in follow-ups beyond 6 months [12,16]. This discrepancy suggests that PRP may act more as a biological catalyst for immediate healing processes rather than a permanent solution for structural reinforcement. Consequently, Tsikopoulos et al. (2016) and Barman argue that while PRP holds value in managing acute symptoms and enhancing early recovery, its role in long-term tendon health and durability remains inconclusive, necessitating further research into potential adjunctive treatments [15,18].
Comparison with previous literature
The findings of this meta-analysis both align with and differ from previous studies on PRP’s efficacy for rotator cuff tendinopathy, providing a more nuanced understanding of its clinical utility. Many earlier studies, such as those by Andia et al. (2014) and DeClercq et al. (2021), highlighted PRP’s potential for reducing pain and improving function in the short term. These results are consistent with the current analysis, which also found significant short-term improvements in pain and functionality within the first 3–6 months following PRP injections [11,17]. This consistency suggests that PRP’s high concentration of growth factors, which initiates early tissue repair processes, is likely beneficial across varied patient populations and injury severities. However, discrepancies arise when considering PRP’s long-term benefits. In previous reviews, such as Parisien et al. (2021), it was noted that PRP’s efficacy tends to diminish over time, often becoming comparable to placebo or corticosteroid treatments by the 1-year follow-up [12]. This finding parallels the results of the current analysis, which shows that while PRP initially reduces pain and enhances function, these benefits frequently decline after 6–12 months. Similarly, Tsikopoulos et al. (2016)and Wangreported that PRP’s long-term impact on tendon structure, as observed through imaging, does not consistently prevent retear rates, a conclusion also reached in the current review [15,19]. These alignments reinforce the notion that while PRP may serve as an effective short-term treatment, it may lack the durability needed for prolonged tendon integrity. There are, however, some differences in interpretation across the literature. For instance, Barman et al. (2022) and Rossi et al. (2021) reported more optimistic findings, suggesting that repeated PRP injections or combining PRP with physical therapy could extend its benefits beyond the initial treatment phase [18,20]. This perspective is less emphasized in the current analysis due to limited data on repeated treatments within the included studies. In addition, Rossi et al. (2021) indicated that certain preparation techniques, like LR-PRP, may produce more favorable outcomes in chronic cases of rotator cuff tendinopathy, a factor that was acknowledged but not extensively analyzed in this review due to variability in study protocols [20]. Moreover, several earlier meta-analyses, including that by Rathod et al. (2024), highlighted concerns regarding PRP preparation standardization, a critical issue that persists in the present review [21]. Inconsistent PRP formulations, differing concentrations of platelets and leukocytes, and various delivery methods all contribute to variability in outcomes. This lack of uniformity has been cited repeatedly in the literature, and studies such as those by Kesikburun et al. (2013) continue to emphasize the need for standardized PRP preparation methods to improve comparability and reproducibility of results [22].
Limitations of the study
This systematic review and meta-analysis, while comprehensive, have several limitations that may impact the interpretation of findings regarding PRP’s efficacy in rotator cuff tendinopathy. A primary limitation is the heterogeneity in study designs. The included studies varied widely in terms of patient populations, study durations, and follow-up periods, which introduces variability in the results. In addition, PRP preparation methods differed significantly across studies, with variations in platelet concentration, leukocyte content, and centrifugation techniques. For instance, some studies used LR-PRP, while others applied leukocyte-poor formulations, which may yield different therapeutic outcomes due to varying inflammatory responses [2,3]. This diversity in PRP formulations complicates direct comparisons and limits the ability to draw consistent conclusions about the optimal PRP type for rotator cuff tendinopathy. Sample sizes were also inconsistent, ranging from small-scale trials with fewer than 50 participants to larger studies involving over 200 patients. Smaller studies may lack the statistical power needed to detect meaningful differences, whereas larger studies tend to produce more reliable results. The inclusion of both small and large trials may therefore contribute to an uneven representation of PRP’s efficacy. In addition, certain studies lacked uniform criteria for outcome measurements, with variations in pain and function assessment tools, which could lead to discrepancies in reported effectiveness [19,20]. Together, these factors create substantial heterogeneity, limiting the generalizability of the findings and underscoring the need for standardized methodologies in future research.
Future research recommendations
To build on the current findings and address existing gaps, future research should prioritize developing standardized protocols for PRP preparation and application. Consistency in PRP composition – including platelet concentration, leukocyte levels, and delivery methods – is crucial to ensuring reproducible results and optimizing therapeutic benefits. Studies by Feltri et al. (2023) and Rathod et al. (2024) underscore the importance of uniformity in PRP protocols to facilitate accurate comparisons across trials and improve clinical decision-making [9,21]. In addition, research should focus on long-term efficacy by extending follow-up periods beyond the typical 6–12 months observed in most studies. Given that PRP’s short-term effects are well-documented, future studies should investigate whether repeated PRP injections or combination therapies, such as PRP with physical therapy, can sustain pain relief and functional gains over multiple years [12,23]. The pooled data reveal that PRP’s regenerative properties can effectively reduce pain and enhance shoulder function within the first three to six months post-injection. These findings align with previous literature, reinforcing PRP’s role as a viable short-term treatment option for patients who may prefer to avoid corticosteroid injections or surgical intervention [21,22]. However, the analysis also highlights PRP’s limitations, particularly in its long-term efficacy, as the benefits often diminish after 12 months. Imaging outcomes and retear rates suggest that while PRP initiates tendon repair, it may not always achieve sustained structural improvements [23,24]. The clinical relevance of these findings suggests that PRP can be a useful therapeutic option in the conservative management of rotator cuff tendinopathy, providing an alternative for patients who seek non-invasive solutions. However, the considerable variability in PRP preparation methods and the lack of standardized protocols present challenges to consistent application and efficacy. To address these limitations, further high-quality RCTs are essential. Future studies should focus on developing standardized PRP protocols, including platelet concentration and leukocyte content, to reduce heterogeneity and enable reliable comparisons. In addition, longer follow-up periods and larger sample sizes are necessary to fully evaluate PRP’s potential for long-term tendon health and function [12,20]. By addressing these research needs, future investigations can clarify PRP’s role in the long-term management of rotator cuff tendinopathy and refine its use as a clinically effective treatment option.
PRP therapy demonstrates significant short-term benefits in alleviating pain and improving shoulder function in patients with rotator cuff tendinopathy. However, its long-term efficacy remains inconclusive, with diminishing benefits observed beyond one year. The variability in PRP preparation methods and protocols underscores the need for standardized approaches to ensure consistent outcomes. While PRP offers a promising alternative to conventional treatments like corticosteroids or surgery, further high-quality studies are essential to establish its role in sustained tendon healing and functional recovery.
PRP therapy offers significant short-term pain relief and functional improvement for rotator cuff tendinopathy. However, clinicians should be cautious about its long-term benefits and consider individualized treatment protocols.
References
- 1.Lin MT, Wei KC, Wu CH. Effectiveness of platelet-rich plasma injection in rotator cuff tendinopathy: A systematic review and meta-analysis of randomized controlled trials. Diagnostics (Basel) 2020;10:189. [Google Scholar | PubMed]
- 2.Xiang XN, Deng J, Liu Y, Yu X, Cheng B, He HC. Conservative treatment of partial-thickness rotator cuff tears and tendinopathy with platelet-rich plasma: A systematic review and meta-analysis. Clin Rehabil 2021;35:1661-73. [Google Scholar | PubMed]
- 3.Hurley ET, Lim Fat D, Moran CJ, Mullett H. The efficacy of platelet-rich plasma and platelet-rich fibrin in arthroscopic rotator cuff repair: A meta-analysis of randomized controlled trials. Am J Sports Med 2019;47:753-61. [Google Scholar | PubMed]
- 4.Lui M, Shih W, Yim N, Brandstater M, Ashfaq M, Tran D. Systematic review and meta-analysis of nonoperative platelet-rich plasma shoulder injections for rotator cuff pathology. PMR 2021;13:1157-68. [Google Scholar | PubMed]
- 5.Chen X, Jones IA, Park C, Vangsness CT Jr. The efficacy of platelet-rich plasma on tendon and ligament healing: A systematic review and meta-analysis with bias assessment. Am J Sports Med 2018;46:2020-32. [Google Scholar | PubMed]
- 6.Dai W, Yan W, Leng X, Wang J, Hu X, Cheng J, et al. Efficacy of platelet-rich plasma versus placebo in the treatment of tendinopathy: A meta-analysis of randomized controlled trials. Clin J Sport Med 2023;33:69-77. [Google Scholar | PubMed]
- 7.Cai YZ, Zhang C, Lin XJ. Efficacy of platelet-rich plasma in arthroscopic repair of full-thickness rotator cuff tears: A meta-analysis. J Shoulder Elbow Surg 2015;24:1852-9. [Google Scholar | PubMed]
- 8.Pang L, Xu Y, Li T, Li Y, Zhu J, Tang X. Platelet-rich plasma injection can be a viable alternative to corticosteroid injection for conservative treatment of rotator cuff disease: A meta-analysis of randomized controlled trials. Arthroscopy 2023;39:402-21.e1. [Google Scholar | PubMed]
- 9.Feltri P, Gonalba GC, Boffa A, Candrian C, Menon A, Randelli PS, et al. Platelet-rich plasma does not improve clinical results in patients with rotator cuff disorders but reduces the retear rate. A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2023;31:1940-52. [Google Scholar | PubMed]
- 10.Masiello F, Pati I, Veropalumbo E, Pupella S, Cruciani M, De Angelis V. Ultrasound-guided injection of platelet-rich plasma for tendinopathies: A systematic review and meta-analysis. Blood Transfus 2023;21:119-36. [Google Scholar | PubMed]
- 11.Andia I, Latorre PM, Gomez MC, Burgos-Alonso N, Abate M, Maffulli N. Platelet-rich plasma in the conservative treatment of painful tendinopathy: A systematic review and meta-analysis of controlled studies. Br Med Bull 2014;110:99-115. [Google Scholar | PubMed]
- 12.Parisien RL, Ehlers C, Cusano A, Tornetta P 3rd, Li X, Wang D. The statistical fragility of platelet-rich plasma in rotator cuff surgery: A systematic review and meta-analysis. Am J Sports Med 2021;49:3437-42. [Google Scholar | PubMed]
- 13.Desouza C, Shetty V. Effectiveness of platelet-rich plasma in partial-thickness rotator cuff tears: A systematic review. J ISAKOS 2024;9:699-708. [Google Scholar | PubMed]
- 14.Giovannetti de Sanctis E, Franceschetti E, De Dona F, Palumbo A, Paciotti M, Franceschi F. The efficacy of injections for partial rotator cuff tears: A systematic review. J Clin Med 2020;10:51. [Google Scholar | PubMed]
- 15.Tsikopoulos K, Tsikopoulos I, Simeonidis E, Papathanasiou E, Haidich AB, Anastasopoulos N, et al. The clinical impact of platelet-rich plasma on tendinopathy compared to placebo or dry needling injections: A meta-analysis. Phys Ther Sport 2016;17:87-94. [Google Scholar | PubMed]
- 16.Zhi F, Cai F, Zhang W, Xiong L, Hu J, Lin X. Clinical efficacy of different shoulder joint drug injections for rotator cuff injuries: A network meta-analysis. Medicine (Baltimore) 2022;101:e30659. [Google Scholar | PubMed]
- 17.DeClercq MG, Fiorentino AM, Lengel HA, Ruzbarsky JJ, Robinson SK, Oberlohr VT, et al. Systematic review of platelet-rich plasma for rotator cuff repair: Are we adhering to the minimum information for studies evaluating biologics in orthopaedics? Orthop J Sports Med 2021. [Google Scholar | PubMed]
- 18.Barman A, Mishra A, Maiti R, Sahoo J, Thakur KB, Sasidharan SK. Can platelet-rich plasma injections provide better pain relief and functional outcomes in persons with common shoulder diseases: A meta-analysis of randomized controlled trials. Clin Shoulder Elb 2022;25:73-89. [Google Scholar | PubMed]
- 19.Wang C, Fan H, Li Y, Yun Z, Zhang Z, Zhu Q. Effectiveness of platelet-rich plasma injections for the treatment of acute Achilles tendon rupture: A systematic review and meta-analysis. Medicine (Baltimore) 2021;100:e27526. [Google Scholar | PubMed]
- 20.Rossi LA, Piuzzi N, Giunta D, Tanoira I, Brandariz R, Pasqualini I, et al. Subacromial platelet-rich plasma injections decrease pain and improve functional outcomes in patients with refractory rotator cuff tendinopathy. Arthroscopy 2021;37:2745-53. [Google Scholar | PubMed]
- 21.Rathod V, Shrivastav S, Gharpinde MR. Platelet-rich plasma therapy for rotator cuff injuries: A comprehensive review of current evidence and future directions. Cureus 2024;16:e70042. [Google Scholar | PubMed]
- 22.Kesikburun S, Tan AK, Yilmaz B, Yaşar E, Yazicioğlu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: A randomized controlled trial with 1-year follow-up. Am J Sports Med 2013;41:2609-16. [Google Scholar | PubMed]
- 23.Liu X, Li Y, Shen L, Yan M. Leukocyte and platelet-rich plasma (L-PRP) in tendon models: A systematic review and meta-analysis of in vivo/in vitro studies. Evid Based Complement Alternat Med 2022;2022. [Google Scholar | PubMed]
- 24.Pithadia P, Sharmila S, Surya P. Platelet rich plasma therapy for shoulder tendinopathy: A systematic. Int J Clin Rheumatol 2021;16:149-57. [Google Scholar | PubMed]