This study compared two methods for treating radial head fractures: ORIF with plating and Herbert screw fixation. Herbert screw fixation led to better functional outcomes, including a greater range of motion and lower disability and pain scores. It was associated with complications, such as stiffness and heterotopic ossification. Overall, Herbert screw fixation may be preferable due to its less invasive nature and reduced complication rate, though further research with larger sample sizes is recommended to validate these findings.
Dr. Setu Kaneria, Department of Orthopaedics, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Dr. D. Y. Patil Vidyapeeth (Deemed to be University) Pimpri, Pune, Maharashtra, India. E-mail: setu.kaneria141@gmail.com
Background: Radial head fractures can be addressed with open reduction and internal fixation (ORIF) using either plating or Herbert screw fixation. This study aimed to evaluate and compare the functional outcomes of these two techniques.
Materials and Methods: A retrospective analysis was conducted on 30 patients who underwent surgery for radial head fractures between June 2020 and July 2023. Patients were assessed using the modified Mason classification and underwent ORIF with either plating or Herbert screws.
Results: This retrospective study evaluated 30 patients with radial head fractures treated between June 2020 and July 2023, comparing outcomes between ORIF with plating versus Herbert screw fixation. The mean age was 45.45 years (standard deviation 12.74). Fractures were evenly classified as Mason type II (15 cases) and Mason type III (15 cases). Patients treated with Herbert screws showed better functional outcomes with higher mayo elbow performance scores (86 ± 2.74 vs. 80 ± 4.47) and lower Quick disability of arm, shoulder, and hand scores (6.4 ± 1.14 vs. 9.6 ± 1.52).
Conclusion: Herbert screw fixation for radial head fractures results in better functional outcomes and fewer complications than plating. However, further studies with larger sample sizes and extended follow-up periods are needed to validate these findings.
Keywords: Quick disability of arm, shoulder, and hand score, mayo elbow performance score, mason classification, headless compression screw, open reduction and internal fixation, radial head fracture.
Radial head fractures are among the most unusual, constituting 20–30% of all elbow fractures in adults [1]. The mechanism of injury for radial neck fractures typically involves an axial load caused by a valgus force and a fall, with the impact on the radiocapitellar joint, which usually transfers 60% of the upper limb load [2-4]. The open reduction and internal fixation (ORIF) technique for the radial head involves using Kirschner wires, T-plate fixation, and screws in a designated safe zone. The screws compress the bone fragments and hold them in place, allowing physiological loads to facilitate healing [5]. However, tissue release around the radial neck for plate repair raises concerns about heterotopic ossification, associated scarring, and radial head revascularization [6]. The Mason category is extensively used to explain radial head-and-neck fractures [7]. Broberg and Morrey et al. changed this category and defined type II fractures as fractures with a displacement of more than 2 mm and concerning at least 30% of the radial head [8]. Johnston et al. later brought type IV fractures to this category, corresponding to radial head or neck fractures related to elbow dislocations [9]. The maximum not unusual classification used today is Hotchkiss’ changed Mason category [10]. It is commonly believed that Mason type 3 and 4 fractures should be treated with ORIF using screw or plate osteosynthesis. The purpose of this study was to compare the functional outcomes between two groups of patients with radial head fractures: One group treated with ORIF and plating and the other with ORIF and Herbert screw fixation.
Study design
A retrospective analysis of 30 patients with radial head fractures who underwent surgery between June 2021 and July 2023 was performed. All patients had been operated on using the Boyd posterior technique by an orthopedic healthcare provider and have been covered in this study. All cases underwent surgical treatment within 1 week of fracture; all fractures were categorized according to Hotchkiss’s modified model of Mason’s category. At some point in this article, any point out of Mason’s classification refers to Hotchkiss’s change [10]. Inclusion criteria include patients above the age of 18 years and isolated radial head fractures. Patients with complex injuries, including Monteggia-like lesions or ligamentous injuries such as elbow dislocations, were excluded. After osteosynthesis is completed, ligament stability is tested intraoperatively. Joint width under varus and valgus stress was evaluated under fluoroscopic control. If instability occurs, reconstruction with suture anchors can resolve the problem. In addition, polytrauma was also considered an exclusion factor. No patient developed Essex-Lopresti syndrome.
Operative procedure
The operative procedure was considered for radial head displaced fractures with more than one fragment, limited supination or pronation, impaired forearm motion, fracture displacement more significant than 2 mm, or when more than one-third of the radial head diameter was fractured [10-14]. All patients underwent surgery using a lateral approach, modified based on Kaplan’s method, which involves operating between the extensor digitorum communis and extensor carpi radialis brevis muscles [15]. The treatment method was selected according to the fractures’ instability and complexity, which were determined using the Hotchkiss modification of the Mason classification. Simple two-part fractures were stabilized with 2 mm headless screws, while more complex, multi-fragmentary fractures were managed with 2.4 mm locking compression radial head plates and 2.0 mm radial head plates. For example, typical cases, including pre-and post-operative X-rays showing screw osteosynthesis for Mason type II fractures, are shown in Figs. 1 and 2, respectively.

The pre- and post-operative X-rays showing plate osteosynthesis for Mason type III fractures are shown in Figs. 3 and 4, respectively.
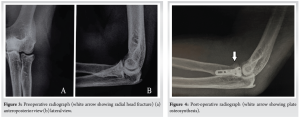
The muscles attached to the posterior supracondyles were released to obtain a complete view of the radial head. In lateral collateral ligament injury cases, suture anchors are used to reattach the ligament to the lateral epicondyle of the humerus. Cortical positioning screws, sized 1.5 mm to 2.0 mm and starting from 18 mm to 34 mm in length, have been used. The wide variety of screws is determined intraoperatively and placed transversely or obliquely as bicortical positioning screws without compression [16]. 10 out of 12 patients have been treated with ≥2 screws, treated with 4 screws (3 out of 30), and two affected person changed into dealt with a single screw (Figs. 1 and 2). There was no need for bone grafting in any individuals.
Follow-up
All patients were followed up for at least 12 months postoperatively. Functional assessment included the use of the Visual Analog Scale (VAS), the Quick disability of arm, shoulder, and hand score (QuickDASH), and the Mayo Elbow Performance Score (MEPS) [17,18]. The QuickDASH score ranges from 0 (no disability) to 100 (total disability), while the MEPS ranges from 0 to 100, with scores ≥90 considered excellent, 75–89 good, 60–74 fair, and below 60 indicating poor outcomes. These assessments were documented using photographs. The MEPS ranges from 0 to 100, where higher values indicate better outcomes [17]. The senior author evaluated the final radiographic images regarding fracture healing. Complications included non-union, infection, implant irritation, nerve injury, or heterotopic ossification. Range of movement was assessed clinically at 6 weeks, 3 months, 6 months, and 12 months postoperatively. Early functional exercises, guided by physiotherapists to encourage free range of motion, were then initiated. Preventing post-operative elbow stiffness is crucial in the aftercare of radius head fractures, whether treated conservatively or surgically. Therefore, all patients were advised to begin physiotherapy exercises early. Weight lifting was prohibited until clinical and radiological assessment at our outpatient clinic 6 weeks postoperatively.
A total of 30 patients met the inclusion criteria, with 12 (40%) being female and 18 (60%) males. The average age was 45.45 ± 12.74 years, ranging from 28 to 64 years. Follow-up occurred at 3 months, 6 months, and 1 year. The classification of fracture morphology showed 15 (50%) Mason type 2 fractures and 15 (50%) Mason type 3 fractures [7-9]. The right elbow was affected more frequently (n = 18, 60%) than the left side (n = 12, 40%); for patients who underwent ORIF with headless screw had slightly poor functional outcomes when compared to those who underwent ORIF with plating as shown in Table 1 and 2.
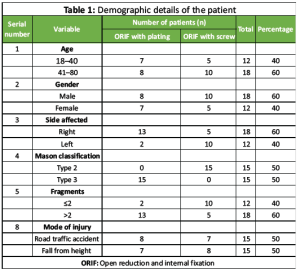
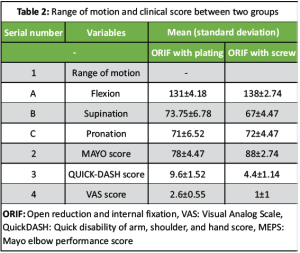
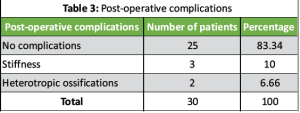
The mayo, Quick-DASH, and VAS scores for patients who underwent open reduction internal fixation with plating were 80 ± 4.47, 9.6 ± 1.52, and 2.6 ± 0.55, and for patients who underwent open reduction internal fixation with screw were 86 ± 2.74, 6.4 ± 1.14, and 1 ± 1, respectively. The flexion-extension arc of the elbow was 134 ± 4.18° for patients who underwent fixation with plating and 136 ± 2.74 for patients who underwent fixation with screws. Patients who received screw osteosynthesis showed substantially higher functional final results scores within the mayo (86 ± 2.74) as compared to patients handled with plate osteosynthesis (80 ± 4.47; P = 0.041). All patients achieved radiological union. Three patients experienced early post-operative elbow stiffness, which improved with passive physiotherapy, and two patients developed heterotopic ossification postoperatively, as shown in Table 3. Posterior interosseous nerve (PIN) neuropraxia was not observed in our study’s patients. There was no significant correlation between type of fracture pattern and gender.
In our series of 30 patients who presented at a selected center and underwent surgical treatment for isolated radial head fractures, we compared outcomes between screw osteosynthesis and plate osteosynthesis. We found that patients treated with screw osteosynthesis had better functional outcomes than those operated with plate osteosynthesis. The plate fixation reported a higher complication rate when compared to screw fixation, though the extent to which this affected outcome remains unclear. A randomized controlled trial was conducted by Chen et al. and unstable Mason III fractures were randomized to ORIF (n = 23, screw and plate) or arthroplasty (n = 22) [19]. ORIF using plates or screws for Mason types II to IV fractures have achieved good outcomes [20,21]. Headless compression screw fixation offers flexibility in screw placement within the radial head, avoiding impingement or stiffness due to well-buried heads [22]. In our study, all fifteen patients treated with screws had good results compared to plate fixation. The superior results of screw fixation have been attributed to minimal surgery compared with plate fixation. Due to the small implant protrusion, the screw head cover is easily achieved by tissue, annular ligament, and capsule repair [23]. Unlike plating, headless compression screws do not require countering. They are suitable for various radial head-and-neck morphologies, reducing soft tissue irritation and interference with elbow or forearm movement. However, mastering headless compression screw fixation requires a learning curve to ensure anatomical reduction and prevent fracture fragmentation. Headless compression screw fixation provided rigid fixation comparable to plate fixation with lower complication and revision rates in our study [6]. Despite challenges in restoring radiocapitellar contact in highly comminuted fractures using screws alone, screw fixation is recommended for three-part radial head fractures with good bone quality [24]. Conventionally, anatomical proximal radial plates (usually “T” or “L” shaped) are commonly used for fixation [25,26]. However, they are less effective in simple radial head-and-neck fractures or fractures with axial instability than in those where they may not adequately cover the fracture. Plate placement requires tissue expansion, which increases the risk of nerve injury (e.g., PIN), non-union, and post-operative stiffness [19,27]. Thick plates may also hinder annular ligament repair, compromising elbow stability and increasing local crepitation and pain during forearm rotation postoperatively [28,29]. Plate osteosynthesis yielded worse functional outcomes compared to screw osteosynthesis based on ESAS scores in our independent comparisons, particularly for Mason III fractures. While Wu et al. found comparable functional outcomes with screw osteosynthesis and higher complication rates with plate osteosynthesis in their study on 3-part radial head fractures, the lack of a prospective randomized design limits definitive conclusions on optimal treatment methods [30]. Surgical treatment with screw and plate osteosynthesis for radial head fractures generally yields good outcomes. However, post-operative function correlates with the initial Mason classification, with worse outcomes reported for Mason type III fractures compared to type I [31]. According to Lorenz, Christina Julia, et al., Mason type III fractures with three- and four-part patterns are more suited to plate osteosynthesis, often leading to favorable clinical outcomes [32]. Headless compression screws provide greater biomechanical stability compared to Mini T-Plates in managing transversely unstable fractures of the radial head and neck, consistent with the findings of our study [33]. Choosing the optimal osteosynthesis method requires precise pre-operative fracture analysis and intraoperative assessment, influenced by the surgeon’s judgment. No definitive superiority of one technique can be generalized from available data.
Limitations
Limitations of our study include potential biases such as selection bias among participating patients versus those who declined, and the non-randomized treatment allocation by surgeons and varied treatment approaches based on surgeon preference and fracture severity, potentially introducing bias due to the small sample size per group, which did not reach statistical significance. The international applicability of the ESAS score remains limited, despite its validation, due to scarce comparative studies. Future directions should focus on long-term follow-up and large-scale prospective cohorts or randomized controlled trials to provide more robust guidance.
This study highlights the advantages of Herbert screw fixation over plating for the management of radial head fractures. Patients treated with Herbert screws demonstrated superior functional outcomes, including higher MEPS and lower QuickDASH and VAS scores, indicating improved elbow function, reduced disability, and lower pain levels. The reduced complication rate, including minimal cases of stiffness and heterotopic ossification, underscores the benefit of a less invasive approach with Herbert screws, which preserves surrounding soft tissue and minimizes surgical morbidity. Although plating offers stability in complex fractures, it is associated with higher risks of post-operative stiffness and soft tissue irritation due to the bulkier implant and the need for extensive tissue dissection. Therefore, Herbert screw fixation is a reliable alternative that promotes better long-term functional recovery and a more favorable post-operative experience. However, given the small sample size and retrospective nature of this study, further research with larger cohorts and randomized controlled trials is essential to validate these findings and refine surgical decision-making protocols for radial head fractures.
Herbert screw fixation for radial head fractures offers superior functional outcomes, better range of motion, and fewer complications compared to plating, making it a preferable surgical option. However, careful patient selection based on fracture type and complexity is essential to achieve optimal results. Surgeons should also be aware of the learning curve associated with screw fixation to ensure precise anatomical reduction and stable fixation. Proper informed consent was obtained from all patients included in this study, ensuring their understanding of the procedure, potential risks, and benefits.
References
- 1.Kani KK, Chew FS. Terrible triad injuries of the elbow. Emerg Radiol 2019;26:341-7. [Google Scholar | PubMed]
- 2.Rosenblatt Y, Athwal GS, Faber KJ. Current recommendations for the treatment of radial head fractures. Orthop Clin North Am 2008;39:173-85. [Google Scholar | PubMed]
- 3.Rhyou IH, Kim KC, Kim KW, Lee JH, Kim SY. Collateral ligament injury in the displaced radial head and neck fracture: Correlation with fracture morphology and management strategy to the torn ulnar collateral ligament. J Shoulder Elbow Surg 2013;22:261-7. [Google Scholar | PubMed]
- 4.Shepard MF, Markolf KL, Dunbar AM. Effects of radial head excision and distal radial shortening on load-sharing in cadaver forearms. J Bone Joint Surg Am 2001;83:92-100. [Google Scholar | PubMed]
- 5.Wheeler DL, McLoughlin SW. Biomechanical assessment of compression screws. Clin Orthop Relat Res 1998;350:237-45. [Google Scholar | PubMed]
- 6.Neumann M, Nyffeler R, Beck M. Comminuted fractures of the radial head and neck: Is fixation to the shaft necessary? J Bone Joint Surg Br 2011;93:223-8. [Google Scholar | PubMed]
- 7.Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg 1954;42:123-32. [Google Scholar | PubMed]
- 8.Broberg MA, Morrey BF. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res 1987;216:109-19. [Google Scholar | PubMed]
- 9.Johnston GW. A follow-up of one hundred cases of fracture of the head of the radius with a review of the literature. Ulster Med J 1962;31:51-6. [Google Scholar | PubMed]
- 10.Hotchkiss RN. Displaced fractures of the radial head: Internal fixation or excision? J Am Acad Orthop Surg 1997;5:1-10. [Google Scholar | PubMed]
- 11.Pike JM, Athwal GS, Faber KJ, King GJ. Radial head fractures--an update. J Hand Surg Am 2009;34:557-65. [Google Scholar | PubMed]
- 12.Pike JM, Grewal R, Athwal GS, Faber KJ, King GJ. Open reduction and internal fixation of radial head fractures: Do outcomes differ between simple and complex injuries? Clin Orthop Relat Res 2014;472:2120-7. [Google Scholar | PubMed]
- 13.Lindenhovius AL, Buijze GA, Kloen P, Ring DC. Correspondence between perceived disability and objective physical impairment after elbow trauma. J Bone Joint Surg Am 2008;90:2090-7. [Google Scholar | PubMed]
- 14.Ruchelsman D, Christoforou D, Jupiter J. Fractures of the radial head and neck. J Bone Joint Surg Am 2013;95:469-78. [Google Scholar | PubMed]
- 15.Surgical Approach to the Proximal end of the Radius and its Use in Fractures of the Head and Neck of the Radius; 1941. Available from: https://journals.lww.com/jbjsjournal/fulltext/1941/23010/surgical_approach_to_the_proximal_end_of_the.8.aspx [Last accessed on 3rd November, 2024. [Google Scholar | PubMed]
- 16.Smith GR, Hotchkiss RN. Radial head and neck fractures: Anatomic guidelines for proper placement of internal fixation. J Shoulder Elbow Surg 1996;5:113-7. [Google Scholar | PubMed]
- 17.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (Quick DASH): Validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord 2006;7:44. [Google Scholar | PubMed]
- 18.Cusick MC, Bonnaig NS, Azar FM, Mauck BM, Smith RA, Throckmorton TW. Accuracy and reliability of the mayo elbow performance score. J Hand Surg Am 2014;39:1146-50. [Google Scholar | PubMed]
- 19.Chen X, Wang S Cao LH, Yang GQ, Li M, Su JC. Comparison between radial head replacement and open reduction and internal fixation in clinical treatment of unstable, multi-fragmented radial head fractures. Int Orthop 2011;35:1071-6. [Google Scholar | PubMed]
- 20.Zwingmann J, Welzel M, Dovi-Akue D, Schmal H, Südkamp NP, Strohm PC. Clinical results after different operative treatment methods of radial head and neck fractures: A systematic review and meta-analysis of clinical outcome. Injury 2013;44:1540-50. [Google Scholar | PubMed]
- 21.Nalbantoglu U, Kocaoglu B, Gereli A, Aktas S, Guven O. Open reduction and internal fixation of mason type III radial head fractures with and without an associated elbow dislocation. J Hand Surg 2007;32:1560-8. [Google Scholar | PubMed]
- 22.Duckworth DG, Avakian Z, Chien C. Newly defined fracture pattern specific to mason III radial head fractures: Fracture description, management and outcomes using screw fixation. ANZ J Surg 2012;82:434-8. [Google Scholar | PubMed]
- 23.Iacobellis C, Visentin A, Aldegheri R. Open reduction and internal fixation of radial head fractures. Musculoskelet Surg 2012;96:81-6. [Google Scholar | PubMed]
- 24.Ring D. Radial head fracture: Open reduction-internal fixation or prosthetic replacement. J Shoulder Elbow Surg 2011;20:107-12. [Google Scholar | PubMed]
- 25.Ikeda M, Yamashina Y, Kamimoto M, Oka Y. Open reduction and internal fixation of comminuted fractures of the radial head using low-profile mini-plates. J Bone Joint Surg Br 2003;85:1040-4. [Google Scholar | PubMed]
- 26.Duckworth AD, McQueen MM, Ring D. Fractures of the radial head. Bone Joint J 2013;95:151-9. [Google Scholar | PubMed]
- 27.Ruan HJ, Fan CY, Liu JJ, Zeng BF. A comparative study of internal fixation and prosthesis replacement for radial head fractures of mason type III. Int Orthop 2009;33:249-53. [Google Scholar | PubMed]
- 28.Biewener A, Bischoff F, Rischke T, Tille E, Nimtschke U, Kasten P, et al. Instability of the proximal radioulnar joint in monteggia fractures-an experimental study. J Orthop Surg Res 2019;14:392. [Google Scholar | PubMed]
- 29.Xu G, Chen W, Yang Z, Yang J, Liang Z, Li W. Finite element analysis of elbow joint stability by different flexion angles of the annular ligament. Orthop Surg 2022;14:2837-44. [Google Scholar | PubMed]
- 30.Wu PH, Shen L, Chee YH. Screw fixation versus arthroplasty versus plate fixation for 3-part radial head fractures. J Orthop Surg (Hong Kong) 2016;24:57-61. [Google Scholar | PubMed]
- 31.Müller M, Mann V, Zapf J, Kirchhoff K, Zyskowski M, Biberthaler P, et al. Functional postoperative outcome for 92 cases of radial head fractures: A PROM-based retrospective study. J Clin Med 2023;12:5870. [Google Scholar | PubMed]
- 32.Lorenz CJ, Carbon CC, Meffert R, Eden L. Plate or arthroplasty for complex mason Type-III radial head fractures? Mid-to-long term results from a blinded outcome assessor study. Injury 2025;56:111981. [Google Scholar | PubMed]
- 33.Yang L, Zhang X, Zhong Z, Li J, Xiong Z. Patient-specific finite element analysis of four different fixation methods for transversely unstable radial head fractures. Sci Rep 2024;14:21134. [Google Scholar | PubMed]











