Periprosthetic fractures of tibia in young population can be managed with revising tibial component and bone grafts without the need for constrained knee or megaprosthesis.
Dr. Nitish Khosla, Department of Orthopaedics, SGL Multispeciality Charitable Hospital, Kapurthala, Punjab, India. E-mail: khoslanitish@gmail.com
Introduction: Periprosthetic fractures of tibia are rarer form of injury after total knee arthroplasty. Most of these fractures occur in elderly patients with osteoporotic bones. Poor bone quality, age, and comorbidities restrict the management options for these fractures to constrained knee or megaprosthesis. However, in younger age group patients, considering the short survival of constrained or mega knee prosthesis in comparison to primary knee, every attempt should be made to restore the primary knee.
Case Report: We report the case of a rare combination type periprosthetic tibial fracture, that is, Felix Type 1B with Felix Type 4, in a 47-year-old female. Considering the young age of the patient and thus good bone quality, we planned for restoration of tibia with bone grafts while revising the tibial component with stemmed tibial base plate, and preserving the cruciate retaining femoral component. The avulsed tibial tuberosity was fixed with cerclage wire looped around the tibial stem. Patient was kept non-weight bearing for 4 weeks, followed by partial weight-bearing for next 6 weeks. Bone grafts were fully incorporated at the final follow-up. Patient had 0–110° range of motion with no limp or laxity in the operated limb.
Conclusion: We conclude that in patients with good bone quality, even if a small part of the tibial plateau is preserved, stemmed tibia with reconstruction of the tibial plateau should be considered as an option to manage the Type 1B fractures, since these patients have high potential for osteointegration of the grafts and restoration of the primary knee will definitely have longer survival than constrained or mega knee prosthesis.
Keywords: Periprosthetic fracture, tibial component, complex Felix classification, primary knee preservation.
Periprosthetic fractures following arthroplasty are increasingly common and present a significant management challenge due to the complex nature of the bony injury and the necessity of maintaining the compatibility of articulating surfaces [1]. Tibial periprosthetic fractures are 4 times less frequent than femoral fractures, resulting in limited data on these more onerous types of periprosthetic fractures [2,3]. Management decisions depend on multiple factors, including bone quality, skin condition, bone stock, and the integrity of the collateral ligaments [4,5]. Most of the unstable periprosthetic tibial fractures occur in elderly patients with osteoporotic bones and are typically managed surgically with either hinge knee prosthesis or megaprosthesis implantation [6]. However, in relatively younger patients with good bone quality, periprosthetic fractures warrant efforts to restore the primary arthroplasty, even in cases of unstable tibial components, to avoid more extensive procedures such as hinge knee or megaprosthesis implantation. We present a case of a complex Felix Type periprosthetic tibial fracture in a young, healthy female, successfully managed by restoring the primary cruciate-retaining (CR) Total knee Arthroplasty (TKA).
History, examination, and pre-operative planning
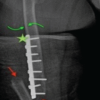
A 47-year-old female, who had undergone bilateral CR total knee arthroplasty (TKA) 2 years prior, for Grade IV osteoarthritis, presented to the emergency department following a fall at home. She was unable to move the affected limb or bear weight on the injured knee since the fall. Clinical examination revealed normal vital signs, an intact peripheral neurovascular status, and healthy overlying skin with localized ecchymosis lateral to the tibial tuberosity. Radiological and hematological investigations were conducted. An X-ray of the knee joint showed a loose tibial component that had sunk into the tibial metaphysis anteriorly, a minimally displaced avulsion of the tibial tuberosity, and a laterally displaced fragment of the lateral tibial condyle (Fig. 1). A fracture line was also observed in the posterior cortex of the tibia. Hematological investigations were within normal limits. Due to the pain and swelling around the knee, it was not possible to fully assess the stability of the knee joint clinically. The patient was thoroughly counseled regarding the possible need for a metaphyseal cone along with a stemmed tibial component or a hinge knee prosthesis. She was also informed about the potential requirement for bone graft harvesting from iliac crest and the necessity of strict bed rest for 1 month if restoration of the primary knee arthroplasty was attempted after reconstructing the tibial bone loss with autogenous bone graft. The surgical plan was to approach the knee joint through the previous incision, using the avulsed tibial tuberosity as a tibial tuberosity osteotomy to enhance exposure of the knee joint. This would allow for an assessment of the bone stock after removing the loose tibial component, before deciding on the further course of management.

Procedure
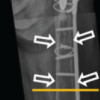
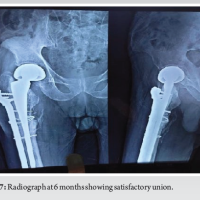
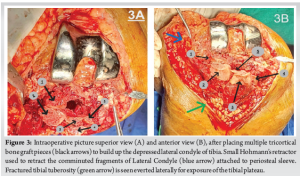
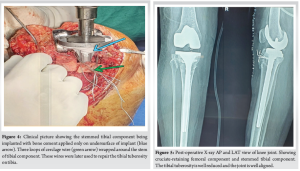
Surgery was performed under spinal anesthesia and tourniquet control. The knee was exposed through the previous incision, with the fractured tibial tuberosity everted laterally, taking care not to breach the lateral periosteum of the tuberosity. The loose implant was removed, and the bone stock was assessed. It was found that the posteromedial half of the tibial plateau was intact, and the tibial component had lifted off at the cement-implant interface. The anterolateral tibial plateau was compressed, but the lateral periosteal sleeve remained intact and attached to the laterally displaced fragment of the tibial plateau (Fig. 2, 3). At this stage, tibial stem preparation began, as a tibial stem was necessary regardless of the final approach. After adequate reaming, the stemmed tibial trial was implanted, seating it on the preserved medial tibial condyle. A trial reduction was performed, and the knee was taken through its full range of motion to assess the integrity of the collateral ligaments and the stability of the knee joint. The rotation of the tibial implant was determined by the preexisting tibial keel flange mark on the medial tibial condyle. Once the knee was confirmed to be stable, the next step was to address the bone loss, either with a metaphyseal cone or bone graft. Given the retained bone stock and pre-operative X-rays, it was determined that preparing for a metaphyseal cone would further erode the medial half of the intact tibial plateau, thereby reducing bone stock. Moreover, placing the lateral tibial plateau bone and tibial tuberosity in opposition to the metallic material of the metaphyseal cone could compromise the healing potential of these fragments with the native tibial bone. Therefore, the final decision was made to rebuild the lateral tibial plateau with bone grafts. A tricortical bone graft was harvested from the ipsilateral iliac crest and shaped into smaller pieces after measuring the depth of the bony defects at different levels on the tibial plateau. A minimal revision cut was made on the tibia to freshen the medial condyle bone for better cementing. Multiple pieces of tricortical bone graft were grafted onto the tibial plateau to rebuild the bone stock (Fig. 4). Gentle tapping over the grafted bone was done by placing the base plate over the tibia to level the grafted bone. Three cerclage wires were looped around the stem of the tibial component, and the final cemented tibial component was implanted (Fig. 5). A trial reduction was performed, and an 11 mm tibial insert was chosen after satisfactory trialing. The lateral end of the cerclage wires was passed through the lateral periosteal sleeve of the tibial tuberosity and tied to the medial ends over the tuberosity after reducing it onto the tibia. The wound was closed in layers over a suction drain, and a post-operative knee brace was applied for 3 weeks. The patient was advised to perform static quadriceps strengthening exercises and calf-pumping exercises from day one. Passive-assisted knee flexion up to 60° was recommended for the first 3 weeks, gradually progressing to 90° over the next 3 weeks. She was kept non-weight-bearing for 4 weeks, followed by partial weight-bearing for the next 6 weeks. The patient was followed up at 1 month, 3 months, 6 months, 1 year, and yearly thereafter. Radiological examinations were performed at each visit, confirming radiological union with good osteointegration of the graft at 6 months (Fig. 6). At 1-year follow-up, the patient regained a range of motion of 0–110°, which was 10° < the opposite knee (Figs. 7, 8). Oxford knee score used to evaluate the functional outcome of the operated knee came out to be 42 compared to 46 on the opposite knee (best outcome score=48).



The overall incidence of tibial periprosthetic fractures is 0.4–1.7% of total primary knee arthroplasty (TKA) surgeries [7]. However, the number of cases is rising due to the increasing number of procedures performed, longer implant survival, and improved life expectancy. Future projections estimate a 2.5-fold increase in periprosthetic fractures by 2030 [8]. Advanced osteoarthritis is becoming more prevalent among relatively younger populations due to lifestyle and dietary habits. This group is more prone to periprosthetic fractures due to their more active lifestyles following surgery. Unlike elderly patients with osteoporosis and comorbidities, younger patients can tolerate restricted mobility for short periods with minimal risk of systemic complications. Therefore, it is crucial to attempt restoration of the primary arthroplasty in these patients, as less constrained implants generally offer longer survival. To support this approach, we aimed to restore the bone anatomy while retaining the CR femoral component, thereby avoiding more constrained knee or megaprosthesis, as reported in the literature [9,10]. We achieved a successful outcome with our patient and believe this technique can be effectively applied to individuals with good bone stock, overall health, and an active lifestyle. A key aspect of this procedure is preserving the vascularity of the fractured fragments to ensure the union and incorporation of the bone graft. If the tibial tuberosity is not fractured, we recommend incorporating procedures such as a quadriceps snip during primary exposure to minimize periosteal stripping of the fracture fragments. All surgical steps should be followed as described, with grafts harvested only after the final implant has been selected and the graft bed prepared. This approach helps maintain the vitality of the bone graft by reducing the time between harvest and implantation. In this case, delayed weight bearing was advised to ensure early radiological signs of bony union of the tuberosity, as the fractured tuberosity lacked step stabilization typical of tibial tuberosity osteotomies. The patient was allowed partial weight bearing with a knee brace after 4 weeks and full weight bearing without a brace at 10 weeks, once the extensor lag had resolved with active quadriceps engagement.
We conclude that in younger patients, even if only a small portion of the tibial plateau is preserved, using a stemmed tibial component with reconstruction of the tibial plateau should be considered for managing Felix Type 1B fractures, since these patients have a high potential for osteointegration of the grafts and restoration of the primary knee will definitely have longer survival then hinged prosthesis and megaprosthesis.
Very limited data is available for in the literature for the management of the fractures discussed in this case study. We have tried to solve the dilemma for the management of periprosthetic fracture in younger age group patients. Every attempt should be made to preserve the primary knee after proper assessment and counseling of the patient.
References
- 1.Felix NA, Stuart MJ, Hanssen AD. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Relat Res 1997;345:113-24. [Google Scholar | PubMed]
- 2.Dennis DA. Periprosthetic fractures following total knee arthroplasty: The good, bad, and ugly. Orthopedics 1998;21:1048-50. [Google Scholar | PubMed]
- 3.Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 2018;100:1455-60. [Google Scholar | PubMed]
- 4.Meek RM, Norwood T, Smith R, Brenkel IJ, Howie CR. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br 2011;93:96-101. [Google Scholar | PubMed]
- 5.5. Benkovich V, Klassov Y, Mazilis B, Bloom S. Periprosthetic fractures of the knee: A comprehensive review. Eur J Orthop Surg Traumatol 2020;30:387-99. [Google Scholar | PubMed]
- 6.Springer BD, Hanssen AD, Sim FH, Lewallen DG. The kinematic rotating hinge prosthesis for complex knee arthroplasty. Clin Orthop Relat Res 2001;392:283-91. [Google Scholar | PubMed]
- 7.Shukla T, Vaish A, Vaishya R, Patralekh MK. Tibial periprosthetic fractures in total knee arthroplasty - a scoping review. J Clin Orthop Trauma 2022;29:101892. [Google Scholar | PubMed]
- 8.Park JW, Won SH, Kim HS, Won SJ, Lee YK, Koo KH. Current incidence and future projection of periprosthetic fractures in South Korea: A study based on national claim database. Orthop Surg 2022;14:530-5. [Google Scholar | PubMed]
- 9.Lewis DP, Tarrant SM, MacKenzie S, Cornford L, Sato T, Shiota N, et al. Managing periprosthetic tibia fractures: International perspectives. OTA Int 2023;6 1 Suppl:e241. [Google Scholar | PubMed]
- 10.Kuzyk PR, Watts E, Backstein D. Revision total knee arthroplasty for the management of periprosthetic fractures. J Am Acad Orthop Surg 2017;25:624-33. [Google Scholar | PubMed]