Pediatric medial clavicular physeal injuries present similarly to adult posterior sternoclavicular joint dislocations, but differ in their ability to remodel and achieve ultimate stability, allowing select cases to be managed non-operatively, with caution and close follow up, with good outcomes.
Dr. Daniel Fernandes, 1 Robert Wood Johnson Plaza, New Brunswick, NJ 08901.E-mail: dff40@rwjms.rutgers.edu
Introduction: Sternoclavicular joint (SCJ) disruptions are rare, with posterior dislocations even less common. In pediatric patients, these injuries primarily manifest as medial clavicular physeal fractures. Posteriorly displaced SCJ injuries are of particular concern due to their potential involvement with mediastinal structures. Treatment options remain variable, with open or closed reduction favored in acute cases and conservative management considered in delayed presentations.
Case Report: We present an 11-year-old male with a posteriorly displaced medial clavicular physeal fracture following a basketball injury managed nonoperatively. Long-term follow-up with computed tomography over the course of a year demonstrated good callus formation and eventual fracture healing. Despite the concerns with his posteriorly displaced SCJ injury, the patient returned to full athletic participation with no complications.
Conclusion: This case supports expectant management as a viable option for medial clavicular physeal fractures with posterior displacement, particularly in delayed presentations without mediastinal involvement. Long-term follow-up demonstrated successful remodeling and return to sport without complications. Given the healing potential of the pediatric medial clavicular epiphysis, further studies are needed to investigate the viability of expectant management.
Keywords: Sternoclavicular joint injury, medial clavicular physeal fracture, posterior sternoclavicular joint displacement, pediatric shoulder injury, conservative management.
Sternoclavicular joint (SCJ) disruptions are relatively rare injuries, accounting for only 3% of all shoulder injuries and <1% of dislocations [1]. Of SCJ dislocations, posterior dislocations are further infrequent, accounting for 3–5%, largely due to the strength of the posterior capsular ligament [2]. In the pediatric population, SCJ injuries come in two main varieties: SCJ dislocations and medial clavicular epiphyseal fractures. Medial epiphyseal fracture is frequently mistaken for an SCJ dislocation and is termed by some as “pseudodislocations.” The medial clavicular epiphysis is the last epiphysis to fuse in the human body, ossifying at 18 years and fusing between 21 and 26 years; thus, these injuries can present into early adulthood [3]. The mechanism is a direct blow to the SCJ, typically secondary to sports injuries, falls, or physical altercations. Posterior SCJ injuries also pose unique challenges given the potential for injury to mediastinal structures, including but not limited to pneumothorax, tracheal injury, great vessel injury, esophageal rupture, brachial plexus palsies, and recurrent laryngeal nerve injuries [4]. Moreover, there are currently no practice-based guidelines for optimal treatment of posterior SCJ injuries [5]. If there are no signs of mediastinal compression, some authors advocate for attempted closed reduction within the first 48 h of injury, whereas others have demonstrated successful closed reduction up to 10 days post-injury [6,7]. Beyond 10 days, conservative management is generally recommended because of the potential for remodeling and the danger of life-threatening hemorrhage with attempted closed reduction [8]. However, given high rates of failed closed reduction, re-subluxation, and recurrent instability, others advocate for surgical reduction and stabilization [9]. Here, we present a case of a medial clavicular physeal fracture with posterior displacement treated with expectant management.
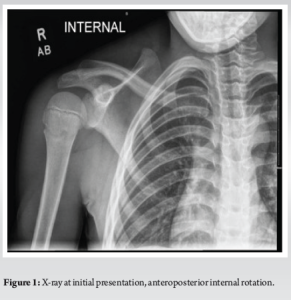
An 11-year-old male with no significant past medical history presented with a right shoulder injury secondary to trauma sustained during a basketball game. He was initially seen in the emergency department at an outside facility and placed into a sling after initial evaluation and X-rays showed no fracture or dislocation (Fig. 1). However, over the subsequent 2 weeks, he continued to have pain, and his mother noticed increased swelling over the anterior aspect of his chest.
Upon presentation to the office, the patient had gross swelling at the medial clavicle and tenderness to the medial third of the clavicle and SCJ, with no pain on glenohumeral range of motion (ROM), no bony crepitus, no difficulty breathing, or shortness of breath. The decision was made to obtain a computed tomography (CT) scan to further characterize the injury, given equivocal radiographs.
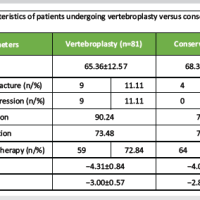
On follow-up 2 weeks later, continued swelling without discomfort on the shoulder ROM was noted on physical examination. CT scan revealed a right medial clavicle epiphyseal fracture and periosteal reaction about the right clavicular shaft consistent with an evolving subperiosteal fracture hematoma, with an intact anterior periosteal sleeve (Table 1). There was concern regarding recurrent injury to the mediastinum given the patient’s active lifestyle, and a lengthy discussion was had regarding surgical intervention. However, the patient and his mother were ultimately elected for non-operative management.

On follow-up 6 weeks after the initial injury, the patient had no complaints of pain and began engaging in sports despite recommendations for strict activity restrictions. A prominence anteriorly over the right medial clavicle was still noted on physical examination, with no tenderness to palpation and a full ROM without pain. Strict activity precautions with no contact sports were advised. Subsequent follow-up 4 months after the initial injury showed a reduction of the prominence about the medial clavicle with no tenderness to palpation and a full ROM without pain. CT scan at 3 months post-injury revealed good interval callus formation along the periosteal sleeve of the medial and middle aspect of the right clavicle (Table 1). Continued activity restrictions from high-impact activities were advised. At the 6-month follow-up, only a small prominence at the medial clavicle remained without tenderness or swelling, and full ROM was again demonstrated. A repeat CT scan demonstrated a healed fracture of the right medial clavicle with bony remodeling extending posteriorly (Table 1). Activity restrictions were lifted at this time. At 1 year, there were no changes in examination, and the patient was a full participant in sports without issue. CT scan revealed a healed medial right clavicular fracture with bony remodeling (Table 1). At 2 years, the patient suffered a minor ankle sprain while playing basketball and presented to the office again without shoulder discomfort, ROM deficit, or limitations in athletics.
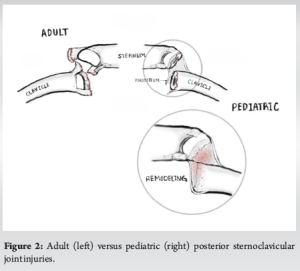
Posterior injuries to the SCJ are rare in pediatric populations, accounting for <3% of all shoulder girdle injuries [1]. Anatomically, the SCJ is a diarthrodial saddle-shaped joint with articulation between the clavicle and manubrium, covered by fibrocartilage rather than hyaline cartilage [10]. Stability is primarily conferred by the posterior sternoclavicular ligament and the costoclavicular ligament in addition to the anterior sternoclavicular ligament, the interclavicular ligament, and the intra-articular disc ligament [11]. Thus, the relative strength of the posterior sternoclavicular ligament makes posterior SCJ injuries far less likely than anterior SCJ injuries. Moreover, the medial clavicular epiphysis is the last epiphysis to close and does not ossify until 18 years of age or fuse with the shaft of the clavicle until 21–26 years of age [3]. True SCJ dislocations in pediatric patients are, therefore, difficult to distinguish from medial clavicular physeal fractures, given the relative weakness of the medial physis. Lee et al. reported in a retrospective review that there is a relatively similar incidence between both injuries, and posterior SCJ injuries may have been initially missed in 25% of patients [12]. In the case presented, given the patient’s age and the nature of remodeling on subsequent CT scans, it was presumed to be a medial clavicle epiphyseal injury, though treatment recommendations in the literature do not differ significantly depending on the pattern of injury. Furthermore, in line with prior literature, this case was initially missed, though there were no mediastinal complications secondary to this. An elevated index of suspicion is necessary, given the risk of injury to posterior mediastinal structures [13]. Although patients can present with dyspnea, dysphagia, hoarseness, cold extremities, or paresthesias, only 30% of patients have been noted to present with any of these additional symptoms [14]. Radiographic imaging has a low sensitivity for detecting SCJ injuries, especially in the anteroposterior view [15]. The serendipity view may allow for better visualization of the SCJ, in which the radiographic beam is tilted at a 40° angle cephalically [16]. CT scan provides better visualization of the SCJ and should be obtained if clinical suspicion for SCJ injury is high, especially since occult injuries to mediastinal structures can be revealed [3]. However, it can be difficult to delineate medial clavicular physeal fractures on CT, with some authors suggesting magnetic resonance imaging as the preferred diagnostic tool given its ability to provide better visualization of the SCJ [17]. Treatment of posterior SCJ injuries may be influenced by skeletal maturity. In adults, these injuries typically remain unstable given the inability for remodeling, bony union, and poor ligamentous healing at the site of injury, thus future impacts may lead to further posterior displacement and endanger mediastinal structures. As such, authors recommend attempted closed reduction in SCJ dislocations regardless of the direction of displacement, and open surgical treatment should be performed in failed closed reductions [18]. In the skeletally immature, in the instance of medial clavicular physeal fractures, there is potential for remodeling and bony union that would adequately stabilize the injury. Children also carry the benefit of a thick periosteal sleeve that is typically intact anteriorly that provides further stability to the fracture and robust healing potential (Fig. 2) [3].
While expectant management may be reasonable in the setting of delayed presentation and advanced imaging evidence of callus formation and periosteal reaction (as in the case presented), indicating a physeal fracture, it is still the author’s practice to obtain reduction, trialing closed and progression to open in the case of failure, given the potential for posterior instability in the acute injury phase as well as the initial difficulty delineating physeal fractures from SCJ dislocations. This patient was initially indicated for reduction of the SCJ injury, but ultimately, the intervention was declined by the family after discussion of the risks. The family elected instead for serial imaging and conservative management. In regard to closed reduction, a meta-analysis of posterior SCJ injuries in patients 12–18 years of age conducted by Tepolt et al. found that most authors recommend a closed reduction of posterior SCJ dislocations in the acute setting unless there is an injury to the trachea, esophagus, or neurovascular structures, a delayed presentation without mediastinal injury, or re-dislocation with chronic pain after a prior closed reduction [5]. Laffosse et al. support an attempted closed reduction within the first 48 h of injury if there are no signs of mediastinal compression, while Groh et al. demonstrated that successful closed reduction can be achieved up to 10 days after injury [6,7]. Although closed reductions may be the first step in management for some, open reductions are typically more reliable given the ability to remove interposed tissues, directly visualize reduction, and provide medial clavicular stabilization allowing for early ROM and full return to activity [13]. Various operative techniques have been used, including large cannulated screws, anterior plating, basilar plate stabilization, suture anchor fixation, resection of the medial clavicle, suture repair of the costoclavicular and sternoclavicular ligaments, figure-of-8 semitendinosus reconstruction, costoclavicular tenodesis, and sternoclavicular tenodesis [5]. Tepolt et al. reported that at a median 26-month follow-up, 92% of patients who underwent closed reduction and 96% of patients who underwent open reduction and internal fixation had full pain-free ROM without recurrence [5]. Despite the recommendations set by Wirth and Rockwood to allow physeal injuries to heal over time, expectant management is rarely used in the treatment of posterior SCJ injuries [8]. Wagner et al. report a case of an 18 years old with a posteriorly displaced medial clavicular physeal fracture successfully treated with expectant management at 8 weeks post-injury [19]. However, the long-term results of immobilization are not well known. In addition, fibrous non-union has been reported 2 years after a missed physeal fracture, and late complications of posterior SCJ can lead to severe injury to mediastinal structures [16,20]. In this case, we present an 11-year-old male who presented with a medial clavicular physeal fracture status post-basketball injury managed conservatively with serial examinations and imaging. Despite posterior displacement, this patient did not go on to develop issues secondary to mediastinal involvement. Furthermore, the patient promptly returned to sports without deficit, pain, or complication and remained asymptomatic at the last follow-up 2 years post-injury, though was only formally cleared for participation in athletics after 6 months and robust healing confirmed on CT. While reduction of these injuries is still the authors’ preferred management, patients may still be treated safely with expectant management once informed discussion is had with the patient and their family. Medial clavicular physeal fractures in particular may have more reliable outcomes given healing potential and ability to remodel. Advanced imaging is likely the only way to confirm appropriate healing of these fractures and significantly increase both the cost of conservative management and radiation exposure to the patient.
Our case contributes to the small body of evidence that medial clavicular physeal fractures with posterior displacement can be successfully treated with expectant management when presenting in a delayed fashion with radiographic evidence of physeal fracture and early healing. It also demonstrates the remodeling potential of the medial clavicular epiphysis through serial advanced images. Further studies should be conducted to demonstrate the utility of expectant management in pediatric patients with delayed presentations of posterior SCJ injuries.
This case report demonstrates that expectant management can be successfully utilized for posteriorly displaced medial clavicular physeal fractures in adolescents with delayed presentations.
References
- 1.Gil-Albarova J, Rebollo-González S, Gómez-Palacio VE, Herrera A. Management of sternoclavicular dislocation in young children: Considerations about diagnosis and treatment of four cases. Musculoskelet Surg 2013;97:137-43. [Google Scholar | PubMed]
- 2.Honeycutt MW, Cox K, Michaeli D, Hulon B, Brewer J. Pediatric posterior sternoclavicular dislocation closed reduction and management. J Orthop Trauma 2021;35:S11-2 [Google Scholar | PubMed]
- 3.Kim WG, Laor T, Jarrett DY. Physeal injuries of the clavicle: Pediatric counterparts to adult acromioclavicular and sternoclavicular joint separations. Pediatr Radiol 2023;53:1513-25. [Google Scholar | PubMed]
- 4.Van Tongel A, De Wilde L. Sternoclavicular joint injuries: A literature review. Muscles Ligaments Tendons J 2012;1:100-5. [Google Scholar | PubMed]
- 5.Tepolt F, Carry PM, Heyn PC, Miller NH. Posterior sternoclavicular joint injuries in the adolescent population: A meta-analysis. Am J Sports Med 2014;42:2517-24. [Google Scholar | PubMed]
- 6.Laffosse J, Espié A, Bonnevialle N, Mansat P, Tricoire JL, Bonnevialle P, et al. Posterior dislocation of the sternoclavicular joint and epiphyseal disruption of the medial clavicle with posterior displacement in sports participants. J Bone Joint Surg Br 2010;92-B:103-9. [Google Scholar | PubMed]
- 7.Groh GI, Wirth MA, Rockwood CA Jr. Treatment of traumatic posterior sternoclavicular dislocations. J Shoulder Elbow Surg 2011;20:107-13. [Google Scholar | PubMed]
- 8.Wirth MA, Rockwood CA Jr. Acute and chronic traumatic injuries of the sternoclavicular joint. J Am Acad Orthop Surg 1996;4:268-78. [Google Scholar | PubMed]
- 9.Jasty N, Bae DS. Sternoclavicular Dislocation. In: Farr S, editors. Congenital and Acquired Deformities of the Pediatric Shoulder Girdle. Cham: Springer; 2022. [Google Scholar | PubMed]
- 10.Klein MA, Miro PA, Spreitzer AM, Carrera GF. MR imaging of the normal sternoclavicular joint: Spectrum of findings. AJR Am J Roentgenol 1995;165:391-3. [Google Scholar | PubMed]
- 11.Lee J, Campbell K, Michalski M, Wilson K, Spiegl U, Wijdicks C, et al. Surgical anatomy of the sternoclavicular joint: A qualitative and quantitative anatomical study. J Bone Joint Surg 2014;96:e166. [Google Scholar | PubMed]
- 12.Lee JT, Nasreddine AY, Black EM, Bae DS, Kocher MS. Posterior sternoclavicular joint injuries in skeletally immature patients. J Pediatr Orthop 2014;34:369-75. [Google Scholar | PubMed]
- 13.Chaudhry S. Pediatric posterior sternoclavicular joint injuries. J Am Acad Orthop Surg 2015;23:468-75. [Google Scholar | PubMed]
- 14.Carmichael KD, Longo A, Lick S, Swischuk L. Posterior sternoclavicular epiphyseal fracture-dislocation with delayed diagnosis. Skeletal Radiol 2006;35:608-12. [Google Scholar | PubMed]
- 15.Sewell MD, Al-Hadithy N, Le Leu A, Lambert SM. Instability of the sternoclavicular joint. Bone Joint J 2013;95-B:721-31. [Google Scholar | PubMed]
- 16.Groh GI, Wirth MA. Management of traumatic sternoclavicular joint injuries. J Am Acad Orthop Surg 2011;19:1-7. [Google Scholar | PubMed]
- 17.Özer UE, Yalçin MB, Kanberoglu K, Bagatur AE. Retrosternal displacement of the clavicle after medial physeal fracture in an adolescent: MRI. J Pediatr Orthop B 2014;23:375-8. [Google Scholar | PubMed]
- 18.Sernandez H, Riehl J. Sternoclavicular joint dislocation: A systematic review and meta-analysis. J Orthop Trauma 2019;33:e251-5. [Google Scholar | PubMed]
- 19.Wagner R, Symanski J, Raasch W, Young C. Successful nonsurgical management of a posteriorly displaced medial clavicular physeal fracture in an adolescent athlete: A case report. Clin J Sport Med 2022;32:e319-21. [Google Scholar | PubMed]
- 20.Oyekanmi C, Higgins G, Nwachukwu IA. Asymptomatic fibrous non-union of displaced sternoclavicular epiphyseal fractures: Case report and literature review. Inj Extra 2005;36:297-9. [Google Scholar | PubMed]