To understand the timing of surgery,surgical technique and rehabilitation protocol.
Dr. K P Chiranjeevi, Department of Orthopaedics, Apollo Hospital, Plot #13, Parsik Hill Road, Off Urban Road, Opp. Nerul Wonder Park, Sector 23, CBD Belapur, Navi Mumbai - 400614, Maharashtra, India. Email: chiranjeevipirabhu@gmail.com
Introduction: Ipsilateral pilon and calcaneal fractures are quite rare. Tibial pilon fractures are uncommon, <1% of all fractures to the lower extremity. Calcaneum is the most frequently fractured tarsal bone.
Case Reports: This is a case report of a 33-year-old male presented on April 21, 2023 in Apollo Hospital, Navi Mumbai with ipsilateral pilon and calcaneal fracture with L2 burst fracture with cauda equina syndrome.
Result: The patient was treated D12–L4 Stabilization with dural repair on April 22, 2023 and was operated on April 28 with internal fixation with plates and screws for pilon and calcaneum .patient was followed up for a period of 1 year postoperatively.
Discussion: Open reduction and internal fixation of displaced calcaneal fractures and pilon fractures by locking plate to maintain the height and joint congruity. Surgery for pilon fractures fixation should be delayed, ideally till “wrinkling of the skin” occurs.
Conclusion: Based on our study, we conclude that a delayed single-stage open reduction and internal fixation with locking plate for calcaneum and pilon fracture with iliac crest bone graft is an excellent treatment option with good post-operative outcome and no significant complications. Axial loading due to a fall from height is the most common mode in these types of injuries.
Keywords: Calcaneum, pilon fracture, internal fixation.
Concomitant ipsilateral pilon fracture with a calcaneum fracture is a rare occurrence. In our case, it is also associated with L2 burst fracture with cauda equina syndrome. Pilon fractures are rare, comprising 3–10% of all fractures of the tibia and 1% of all lower extremity fractures. Pilon is the French word for “pestle” and was introduced in 1911 by French radiologist Étienne Destot [1]. About 2% of all fractures are calcaneal fractures. However, they make up 60% of fractures of the midfoot bones [2].
Pre-operative evaluation
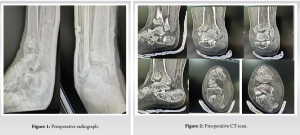
A 33 year old male came with alleged history of fall from electric pole after suffering electric shock and was taken to outside hospital and there he was diagnosed to have compression fracture of L2 (burst type) with right pilon fracture and right calcaneum fracture (sanders type 4) (Fig. 1) and later patient shifted to Apollo hospital neurologically Right hip ⅕ knee ⅕ and ankle 0/5, Left hip 1/5knee ⅕ and ankle 0/5, Perianal sensation decreased. A CT scan was done, suggestive of a displaced fracture medial malleolus and an intra-articular displaced calcaneum fracture (Figs. 2 and 3). Fracture was temporarily stabilized with below knee pop-back slab and limb elevation given. Patient underwent D12–L4 stabilization with dural repair for L2 burst fracture and cauda equina (Fig. 4). For 5 days, patient was optimized in ICU. The patient was planned for definitive fixation of calcaneal and pilon fracture.

Surgical technique
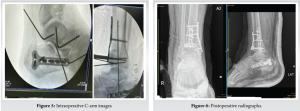
A third-generation cephalosporin was administered for prophylaxis during the induction of general anesthesia. The patient was first placed in a floppy lateral position for reconstruction of the calcaneal fracture. The surgery was performed under tourniquet hemostasis, and a lateral approach was used. A full-thickness subperiosteal flap was raised and reduced with Kirschner wires. The fracture was stabilized with a Locking T plate and screws. Subsequently, the tourniquet was released. Closure done with 2-0 Ethilon and mini VAC kept. The tourniquet was reinflated. The pilon fracture was exposed through an anteromedial incision, with care taken to minimize soft-tissue dissection. The fracture was reduced temporarily with K wires and fixed with an AO cruciate locking T plate and LC DCP Plate and screws. Cancellous bone graft was harvested from the ipsilateral iliac crest to support the articular surface (Fig. 5). Closure was done with 2-0 Ethilon. Below Knee- Back slab applied.
Postoperative period
Postoperative radiograph (Fig. 6) showed stable fixation.
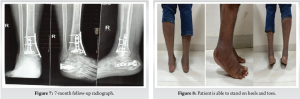
In the postoperative period, the left lower limb was kept elevated and, after swelling had reduced, a cast was applied. At the time of discharge, power of lower limbs improved to grade 3. Mobilization of the ankle and subtalar joints was initiated once the incisions had healed. The patient received physiotherapy treatment for 6 months. After discharge from the hospital, the patient was followed regularly for clinical and radiographic assessment in the outpatient clinic. The patient had good neurological recovery and regained bowel and bladder control. For the first 2 months, the patient was kept non-weight bearing on the right lower limb. He then gradually progressed to full weight bearing. 3 months postoperative, both fractures had gone on to unite clinically and radiologically. At final follow-up, after surgery, there was no radiographic evidence of posttraumatic osteoarthritis (Fig. 7).
Immediate post-operative shows acceptable Calcaneal height, but it is reduced later on which is common in comminuted calcaneal fracture.
The patient had terminal restriction of range of motion of both the ankle and the subtalar joints (Fig. 8 and 9).
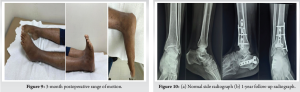
The patient had full neurological recovery at 9 months of follow-up. At 1-year follow-up, radiograph shows complete radiological union, and the patient did not have any further loss in calcaneal height (Fig. 10).
The timing of surgery becomes critical in achieving a good outcome and to reduced complications. The historically high rates of infection associated with open reduction and internal fixation of pilon fractures may be due to attempts at immediate fixation through swollen, compromised soft tissues [3]. Hence, it is important to wait for the development of wrinkle in skin “wrinkling of the skin” seems to be the best indicator for deciding surgery, which in most cases will occur ~10–14 days after the trauma [4]. The location of the blisters might also limit surgical approaches [5]. In a prospective study of 53 cases complicated by fracture blisters, Giordano and Koval found no significant difference in outcome whether the blisters were aspirated, de-roofed, or left intact. 2 cases of wound infection occurred when an incision was made directly through blood-filled blisters [6]. Hence, we applied a temporary splint and kept the limb elevated and delayed our surgery by 5 days. The results of ORIF and EFLIF in the treatment of high-energy pilon fractures are equally effective in terms of functional outcomes and complication rates in the short term [7]. Conventional radiographs are limited for visualization of the calcaneal anatomy, especially at the subtalar joint. A CT scan is currently the imaging study of choice for evaluating calcaneal injury and has substituted conventional radiography in the classification of calcaneal fractures [8]. In a study of 26 distal tibial explosion fractures in 24 patients results of operative treatment were, however, superior to the results of non-operative treatment. Adequate treatment consists of anatomic reconstruction of the distal tibia, rigid internal fixation, early active motion, and nonweight bearing in 3–5 months [9]. A strong Axial load is the reason for the development of ipsilateral pilon fracture and calcaneum fracture as proven by a cadaveric study, Yoganandan et al. [10]. The occurrence of deep vein thrombosis in trauma patients is high, with the incidence ranging from 20 to 90% [11]. Anatomic open reduction and stable internal fixation led to an excellent result in this particular patient at a follow-up of 9 months [12]. These fractures are better treated either with external fixation or with open reduction and internal fixation techniques, depending on the surgeon’s preference and the fracture configuration [13].
The timing of surgery, surgical technique, method of fixation, and early mobilization play an important role in achieving a good functional outcome and to reduce the chances of infection.
Comprehensive radiological evaluation with appropriately timed surgical intervention with an anatomical fixation with appropriate implants and early mobilsation are the key to achieve good functional outcome.
References
- 1.Mandi DM, Belin RP, Banks J, Barrett B. Pilon fractures. Clin Podiatr Med Surg 2012;29:243-78, 8. [Google Scholar | PubMed]
- 2.Palmersheim K, Hines B, Olsen BL. Calcaneal fractures: Update on current treatments. Clin Podiatr Med Surg 2012;29:205-20, 7. [Google Scholar | PubMed]
- 3.Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma 1999;13:78-84. [Google Scholar | PubMed]
- 4.Calori GM, Tagliabue L, Mazza E, De Bellis U, Pierannunzii L, Marelli BM, et al. Tibial pilon fractures: Which method of treatment? Injury 2010;41:1183-90. [Google Scholar | PubMed]
- 5.Saad BN, Yingling JM, Liporace FA, Yoon RS. Pilon fractures: Challenges and solutions. Orthop Res Rev 2019;11:149-57. [Google Scholar | PubMed]
- 6.Giordano CP, Koval KJ. Treatment of fracture blisters: A prospective study of 53 cases. J Orthop Trauma 1995;9:171-6. [Google Scholar | PubMed]
- 7.Rayan A, Kotb A, Elmoatasem EM, Samir S, EL-Sobky TA, El-Hawi E, et al. Open reduction internal fixation versus external fixation with limited internal fixation for displaced comminuted closed pilon fractures: A randomised prospective study. J Orthop Trauma Rehabil 2018;24:84-9. [Google Scholar | PubMed]
- 8.Badillo K, Pacheco JA, Padua SO, Gomez AA, Colon E, Vidal JA. Multidetector CT evaluation of calcaneal fractures. Radiographics 2011;31:81-92. [Google Scholar | PubMed]
- 9.Kellam JF, Waddell JP. Fractures of the distal tibial metaphysis with intra-articular extension - the distal tibial explosion fracture. J Trauma 1979;19:593-601. [Google Scholar | PubMed]
- 10.Yoganandan N, Pintar FA, Kumaresan S, Boynton M. Axial impact biomechanics of the human foot-ankle complex. J Biomech Eng 1997;119:433-7. [Google Scholar | PubMed]
- 11.Hak DJ. Prevention of venous thromboembolism in trauma and long bone fractures. Curr Opin Pulm Med 2001;7:338-43. [Google Scholar | PubMed]
- 12.Bretschneider H, Rammelt S. Combined ipsilateral fracture of the tibial pilon, talar body, and calcaneus: Outcome at 4 years. Indian J Orthop 2018;52:334-8. [Google Scholar | PubMed]
- 13.Mittal R, Matthews SJ, Zavras DT, Giannoudis PV. Management of ipsilateral pilon and calcaneal fractures: A report of 2 cases. J Foot Ankle Surg 2004;43:123-30. [Google Scholar | PubMed]