The key learning point of this case report is that even in the rare and severe complication of clavicular osteomyelitis leading to near-total clavicular resorption, functional outcomes can remain surprisingly good. This emphasizes that clinical recovery and function should be prioritized over radiological findings when assessing a patient’s progress. It also highlights the need for early diagnosis, prompt treatment, and long-term follow-up to manage potential complications effectively.
Dr. Karan R Lakhani, Department of Orthopaedics, Government Medical College and Hospital, MARD Hostel, Government Medical College and Hospital, Nagpur, Maharashtra, India. E-mail-karanlakhani@ymail.com
Introduction: Clavicular osteomyelitis, a rare infection in children under 5, often arises from hematogenous spread. Treatment generally involves debridement and intravenous antibiotics to avert complications such as sepsis and mediastinitis. This case reports the first instance of complete clavicular resorption following debridement. Remarkably, 13 years later, the patient exhibits minimal functional impairment and can perform all daily activities.
Case Report: A 9-month-old infant presented to us with medial clavicular osteomyelitis which was cured by debridement and intravenous antibiotics. Follow-up was completed at 5 years and 13 years after the surgical procedure and complete clavicular resorption was noted with no noted functional deficit.
Conclusion: Clavicular osteomyelitis is a rare presentation and in spite of eradication of infection there can be complete resorption of the bone. Despite complete clavicular resorption, no noted functional deficits were present.
Keywords: Absent clavicle, complete clavicular resorption, clavicular osteomyelitis.
Clavicular osteomyelitis is a rare form of infection caused by hematogenous spread or trauma [1-3] Children below 5 years of age are particularly susceptible to hematogenous spread of acute osteomyelitis owing to their vascular metaphyseal ends. The objective of the management of clavicular osteomyelitis remains the elimination of infection with the help of debridement and intravenous antibiotics in order to prevent serious complications like sepsis, mediastinitis and haemorrhage from great vessels [4,5]. We present the first reported case in literature of complication in the form of complete clavicular resorption following debridement for osteomyelitis. Surprisingly, at 13-year follow-up, the patient has minimal functional deficit and is able to perform all his activities of daily living.
A 9-month-old infant presented to us with high-grade fever and pain in the region of the medial end of right clavicle (Fig. 1). Clinical examination revealed tenderness, swelling and discharging sinus over medial end of clavicle. Serological parameters and magnetic resonance imaging (MRI) were suggestive of medial clavicular osteomyelitis. The patient was operated on with incision, drainage of pus and wide local debridement for the osteomyelitis, and pus was sent for culture. The patient was given sensitive antibiotics for 6 weeks and the patient was kept on regular follow-up. There was complete resolution of infection at 6-week follow-up with no evidence of recurrence. The wound healed uneventfully and there was no clinical or serological evidence of infection. At sequential follow-ups of 1 and 5 years clavicle was not visualized (Fig. 2-4). At the latest 13-year follow-up, the patient has no evidence of right clavicle bone in comparison to the complete normal left clavicle (Fig. 5; 6a and b). But upon detailed clinical evaluation, the patient has no functional deficit (Fig. 7 and 8). He is able to attend school and carry out all his daily activities without any trouble whatsoever. Manual muscle testing grading showed near-normal power in all the muscle groups of the right upper limb. The DASH score in the right limb was 10 signifying better function. The grip strength of the right hand was not reduced as compared to the opposite normal side.
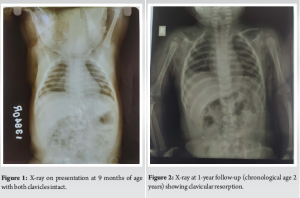
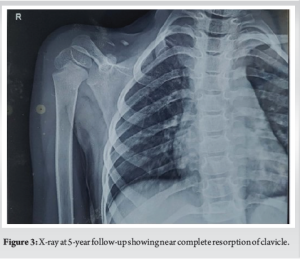
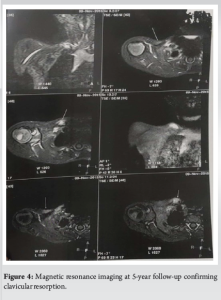

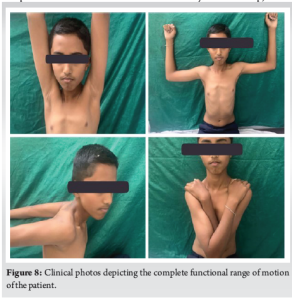
Hematogenous osteomyelitis of the clavicle is a rare entity with the incidence being around 1–3% [6,7]. Owing to the similarity of the clavicle to other membranous bones like ilium, osteomyelitis of clavicle is more difficult to treat than osteomyelitis of long bones [8]. The primary aim of management remains early diagnosis and prompt management with wide local debridement and appropriate sensitive intravenous antibiotics [1,9]. The known complications of clavicular osteomyelitis are sepsis, mediastinitis and hemorrhage from great vessels [10]. A rare and sparsely reported complication of osteomyelitis remains resorption of the bone. Bacterial infection of bone causes inflammatory bone loss that results from an imbalance between the increased activity of bone-resorbing osteoclasts, and a decrease in bone-forming osteoblasts [11]. In our case, it was noted at sequential follow-ups that the clavicle had not grown as much as the opposite side. There was definitive evidence of clavicular resorption at 1- and 5-year follow-ups. At sequential follow–up, the patient had no complaints of functional deficit. At final 13-year follow-up, we decided to go for a detailed evaluation of the status of the upper limb. Clinical examination revealed no functional deficit whatsoever. The patient has no difficulties in performing all the activities of daily living. He is able to attend school and play merrily. Objective evaluation with DASH score was around 10 pts (Range 0–150 with 0 being best function and 150 being poor function) and the grip strength by dynamometer showed no significant difference as compared to the normal opposite side. Upon imaging the X-ray, computed tomography and MRI revealed complete clavicular resorption. In this particular case, the patient has no clavicle at all! Yet he is able to perform all his activities smoothly and without any deficit.
This case highlights an unusual outcome of clavicle osteomyelitis, where a nearly complete resorption of the clavicle resulted in minimal functional deficit. It underscores the importance for clinicians to prioritize clinical recovery over radiological findings when assessing patient progress.
Clavicular osteomyelitis, though rare, can lead to significant bone loss, as seen in this case of near-total clavicular resorption. Despite this, early diagnosis, prompt debridement, and appropriate antibiotic therapy can result in favorable functional outcomes. This case underscores the importance of prioritizing clinical recovery over radiological findings in assessing long-term function. Clinicians should be aware that complete resorption of the clavicle may not necessarily lead to significant functional deficits, and patients may continue to lead normal lives with appropriate management and follow-up.
References
- 1.Waldvogel FA, Medoff G, Swartz MN. Osteomyelitis: A review of clinical features, therapeutic considerations and unusual aspects. N Engl J Med 1970;282:198-206. [Google Scholar | PubMed]
- 2.Sonobe M, Miyazaki M, Nakagawa M, Ikegami N, Suzumura Y, Nagasawa M, et al. Descending necrotizing mediastinitis with sternocostoclavicular osteomyelitis and partial thoracic empyema: Report of a case. Surg Today 1999;29:1287-9. [Google Scholar | PubMed]
- 3.Balakrishnan C, Vashi C, Jackson O, Hess J. Post-traumatic osteomyelitis of the clavicle: A case report and review of literature. Can J Plast Surg 2008;16:89-91. [Google Scholar | PubMed]
- 4.Pineda C, Vargas A, Rodríguez AV. Imaging of osteomyelitis: Current concepts. Infect Dis Clin North Am 2006;20:789-825. [Google Scholar | PubMed]
- 5.Harik NS, Smeltzer MS. Management of acute hematogenous osteomyelitis in children. Expert Rev Anti Infect Ther 2010;8:175-81. [Google Scholar | PubMed]
- 6.Donovan RM, Shah KJ. Unusual sites of acute osteomyelitis in childhood. Clin Radiol 1982;33:222-30. [Google Scholar | PubMed]
- 7.Chrysochoou EA, Antachopoulos C, Badekas K, Roilides E. A rare case of clavicle osteomyelitis in a child and literature review. Case Rep Pediatr 2016;2016:8252318. [Google Scholar | PubMed]
- 8.Alessi DM, Sercarz JA, Calcaterra TC. Osteomyelitis of the clavicle. Arch Otolaryngol Head Neck Surg 1988;114:1000-2. [Google Scholar | PubMed]
- 9.Le Saux N, Howard A, Barrowman NJ, Gaboury I, Sampson M, Moher D. Shorter courses of parenteral antibiotic therapy do not appear to influence response rates for children with acute hematogenous osteomyelitis: A systematic review. BMC Infect Dis 2002;2:16. [Google Scholar | PubMed]
- 10.Kocutar T, Snoj Ž, Salapura V. Complicated acute haematogenous osteomyelitis with fatal outcome following a closed clavicle fracture-a case report and literature review. BJR Case Rep 2016;2:20150389. [Google Scholar | PubMed]
- 11.Marriott I. Apoptosis-associated uncoupling of bone formation and resorption in osteomyelitis. Front Cell Infect Microbiol 2013;3:101. [Google Scholar | PubMed]