Dual bone grafting using a sandwich technique may enhance healing and function in scaphoid non-union with deformity, offering a promising alternative to traditional methods.
Dr Ankush Mohabey, Department of Orthopaedics, All India Institute of Medical Sciences, Nagpur, MIHAN, Nagpur - 441 108, Maharashtra, India. E-mail: ankushmohabey@aiimsnagpur.edu.in
Introduction: Scaphoid non-union (SNU) is a potential complication of scaphoid fractures due to limited blood supply, primarily from the radial artery. The scaphoid’s lack of a periosteum restricts its ability to undergo efficient healing, relying solely on primary bone healing.
Case Report: This case report aims to evaluate the management of SNU, particularly in waist fractures with shortening and humpback deformity. It assesses the clinical, radiographic, and functional outcomes of patients treated with bone grafting, utilizing tricalcium phosphate and cancellous bone grafts, contributing to the ongoing discussion on optimal treatment strategies for SNU cases.
Conclusion: Learning points of view from this article include: The use of dual bone grafting gives good results in terms of union and patient function. Tricalcium phosphate is an effective augment for autograft in cases of non-union.
Keywords: Scaphoid fractures, non-union, tricalcium phosphate, grafting, fracture fixation.
The wrist joint is highly intricate, made up of numerous interconnected bones that form complex articulations, enabling a wide range of motion. Among these bones, the scaphoid is particularly notable for its complex three-dimensional structure and distinct orientation. This unique design is essential to the wrist’s biomechanics, affecting both its mobility and stability, and makes the scaphoid a vital element in wrist function. Scaphoid fractures rank as the second most frequent wrist injury, after distal radius fractures [1]. Scaphoid non-union (SNU) is a possible complication of scaphoid fractures due to the bone’s limited healing ability. This is because the scaphoid receives inadequate blood supply, primarily from the radial artery, which enters the bone through small holes on its dorsal side. The scaphoid lacks a periosteum, which means it can only undergo primary bone healing, a process that may be less efficient in certain situations [2]. In cases of displaced or unstable fractures, healing is compromised, leading to bone resorption and potential bone loss at the scaphoid waist. As a result, the bone may shorten, and the distal pole may tilt toward the wrist, causing a flexion deformity. The scaphoid bone is particularly vulnerable to non-union and avascular necrosis of the proximal pole due to factors such as its retrograde blood supply, high shear stress from its shape, fractures with a gap of 1 mm or more, delayed diagnosis, and improper treatment [3]. These conditions hinder proper healing and blood flow to the bone. The treatment of scaphoid fractures has primarily concentrated on ensuring bone union, while less emphasis has been placed on restoring the scaphoid’s original shape and alignment.
The scaphoid is susceptible not only to non-union but also to malunion. Its shape and orientation naturally create a flexion force that is transmitted to the lunate through the scapholunate (SL) ligament. The flexion force is opposed by an extension force generated by the triquetrum through the lunotriquetral ligament. However, this balance can be disturbed if a scaphoid fracture occurs. The location of the fracture to the SL and dorsal intercarpal (DIC) ligaments determines the type of non-union deformity. If the fracture occurs distal to the apex of the dorsal ridge (waist) of the scaphoid, the proximal fragment extends. This happens because the SL and DIC ligaments, which attach above the dorsal ridge, anchor the proximal fragment, leading to the development of a humpback deformity [4]. Scaphoid humpback deformity involves volar shortening, angulation of the scaphoid with the apex facing dorsally, dorsal displacement of the distal fragment, and a dorsal intercalated segment instability (DISI) deformity. The extension of the proximal pole and flexion of the distal pole causes the fracture site to open on the dorsal side. Ongoing movement at the fracture site leads to bone resorption, especially on the volar side, resulting in volar shortening and carpal collapse. This case report seeks to contribute to the ongoing discussion regarding the management of SNU cases, specifically those involving waist fractures with shortening and humpback deformity [5]. It focuses on evaluating the clinical, radiographic, and functional outcomes of patients treated with bone grafting, which includes tricalcium phosphate and cancellous bone graft.
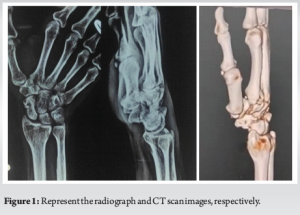
A 58-year-old right-hand-dominant male presented with pain and stiffness in his right wrist, which has been ongoing for several months. The initial injury occurred 8 months ago when he fell onto his outstretched hand. The patient is a non-smoker and has generally been in good health. He was previously diagnosed with a scaphoid fracture and opted for conservative management at the time. However, over the past few months, he has experienced worsening pain and stiffness, which have been affecting his ability to perform daily activities. There is no history of any further trauma since the initial injury. Radiographs revealed a fracture through the waist of the scaphoid, accompanied by a notable humpback deformity. A CT scan was performed to assist in further planning and to confirm the union status of the fracture. In addition, an MRI was conducted to assess for any signs of avascular necrosis in the proximal fragment, which appeared to be within normal limits (Fig. 1). We reviewed the management options with the patient, including the possibility of salvage surgery if the primary intervention failed. A right scaphoid open reduction and internal fixation were performed using Herbert screws, along with a cancellous bone graft harvested from the radius through the same incision. A bone substitute, tricalcium phosphate, was also used. Postoperatively, the patient was placed in a below-elbow slab for a period of 4 weeks (Fig. 2a-d). The patient was started on a range of motion exercises of the wrist and thumb including Handgrip exercises and tabletop exercises. Heavy weight lifting was prohibited for the whole follow-up period. The patient was followed up for a period of 6 months, during which his range of motion showed significant improvement. The DASH (Disabilities of the Arm, Shoulder, and Hand) score decreased from 46 at the time of admission to 8 at the 6-month post-operative follow-up. The patient reported no functional disability at this stage. Six months following the procedure, the patient exhibited good wrist function and grip strength. The range of motion of the wrist increased from 40° of flexion and extension preoperatively to 80° flexion and 70° extension post-rehab. Radiographs showed clear signs of fracture union (Fig. 3).


To provide proper context, it is important for readers to understand that this article does not endorse this method as the sole approach for all scaphoid fractures or SNU. We present this case report to highlight the use of dual bone grafting in the management of SNUs, aiming to contribute to the growing body of literature on this topic. The delayed presentation of SNU continues to pose significant challenges for hand surgeons and can be a complex issue for surgical planning, requiring careful consideration to ensure the best outcomes for patients. Certain intraoperative tricks are needed for good exposure and clean dissection, keeping vital structures intact, using 2 Kirchner wires in both the proximal and distal segments of the scaphoid, and using it as a joystick for distraction and opening of non-union sites. Sandwiching graft by outer layers with tricalcium phosphate and cancellous graft inside between non-union sites. The guide wire was used instead of Kirschner wires for provisionally holding the graft to prevent escaping of graft and drilling only the proximal fragment for insertion of Herbert screw. The idea behind using compression devices such as Herbert screws is to promote faster bone healing. It is widely recognized that applying compression to cancellous bone accelerates the healing process [6]. Furthermore, conservative treatment also poses a significant threat of causing non-union in cases of significant displaced fractures, and hence, surgical treatment is chosen as a better option [7,8]. However, this objective must be carefully balanced with the need to prevent the shortening of the bone or loss of graft material. The scaphoid is particularly challenging due to its limited blood supply and tendency for poor fracture healing. It is important to note that bone grafting in scaphoid waist non-union is necessary not only to promote union but also to restore the normal dimensions of the scaphoid and maintain proper carpal alignment. As such, the selected graft must possess both strong biological properties and reliable mechanical strength. In summary, scaphoid humpback non-union deformity is characterized by volar shortening, angulation with the apex dorsally, a dorsal shift of the distal fragment, and a DISI deformity. Correcting the DISI deformity is crucial in the treatment of SNU to prevent kinetic issues that could lead to arthritic changes. CT scanning is valuable for visualizing the humpback deformity, assisting in selecting the surgical approach, planning the non-union defect and graft size, simulating deformity correction, and evaluating the healing process. We selected a palmar approach for dissection due to the presence of the humpback deformity, as it allows for easier access to correct the deformity from this side. In addition, using a distal end radius graft minimizes donor site morbidity and eliminates the need for further dissection at additional sites. [9,10] We also used Tricalcium phosphate as an adjuvant graft along with cancellous graft, which provided scaphoid for better union and is something that is not done routinely and has very limited literature regarding the same.
SNU remains a complex and widely debated topic, with numerous studies exploring various approaches to its management. However, certain key principles remain critical: operative intervention is often required, and bone grafting is essential. The primary goal of treatment is to prevent future complications, such as arthritis and avascular necrosis. In addition, host factors play a crucial role in the outcome, and their importance should be considered alongside the management principles.
SNU remains a challenging orthopedic condition due to the bone’s unique vascularity and biomechanical properties. This case report highlights the use of dual bone grafting – tricalcium phosphate and cancellous bone grafts – as an effective approach for SNU management. The combination of structural support and biological integration facilitates bone healing while restoring wrist biomechanics. Early diagnosis and appropriate surgical intervention are crucial in preventing long-term complications such as degenerative arthritis and avascular necrosis. This report contributes to the ongoing discussion on optimizing treatment strategies for SNU cases.
References
- 1.Kirkham SG, Millar MJ. Cancellous bone graft and Kirschner wire fixation as a treatment for cavitary-type scaphoid nonunions exhibiting DISI. Hand (N Y) 2012;7:86-93. [Google Scholar | PubMed]
- 2.De Vitis R, Passiatore M, Perna A, Tulli A, Pagliei A, Taccardo G. Modified matti-russe technique using a “butterfly bone graft” for treatment of scaphoid non-union. J Orthop 2020;19:63-6. [Google Scholar | PubMed]
- 3.Samade R, Awan HM. Surgical treatment of scaphoid fractures: Recommendations for management. J Wrist Surg 2024;13:194-201. [Google Scholar | PubMed]
- 4.Mathoulin CL, Arianni M. Treatment of the scaphoid humpback deformity - is correction of the dorsal intercalated segment instability deformity critical? J Hand Surg Eur Vol 2018;43:13-23. [Google Scholar | PubMed]
- 5.Ferguson DO, Shanbhag V, Hedley H, Reichert I, Lipscombe S, Davis TR. Scaphoid fracture non-union: A systematic review of surgical treatment using bone graft. J Hand Surg Eur 2016;41:492-500. [Google Scholar | PubMed]
- 6.Proctor MT. Non-union of the scaphoid: Early and late management. Injury 1994;25:15-20. [Google Scholar | PubMed]
- 7.Singh HP, Taub N, Dias JJ. Management of displaced fractures of the waist of the scaphoid: Meta-analyses of comparative studies. Injury 2012;43:933-9. [Google Scholar | PubMed]
- 8.Siotos C, Asif M, Lee J, Horen SR, Seal SM, Derman GH, et al. Cast selection and non-union rates for acute scaphoid fractures treated conservatively: A systematic review and meta-analysis. J Plast Surg Hand Surg 2023;57:16-21. [Google Scholar | PubMed]
- 9.Özalp T, Öz Ç, Kale G, Erkan S. Scaphoid nonunion treated with vascularised bone graft from dorsal radius. Injury 2015;46:S47-52. [Google Scholar | PubMed]
- 10.Baamir A, Dhellemmes O, Coquerel-Beghin D, Auquit-Auckbur I. Graft choice for managing scaphoid non-union: Umbrella review. Hand Surg Rehabil 2024;43:101759. [Google Scholar | PubMed]










