Ilizarov ring fixation provides an effective, minimally invasive approach for complex comminuted tibial fractures with soft tissue compromise, enabling full union and functional recovery through distraction osteogenesis without bone grafting or secondary procedures.
Dr. Avik Kumar Naskar, Department of Orthopaedics, Indira Gandhi Government Medical College and Hospital, Nagpur, Maharashtra, India. E-mail: avik7933@gmail.com
Introduction: Tibial fractures, particularly complex and open types, present significant challenges in orthopedic trauma care due to their risk of complications and prolonged recovery. The Ilizarov technique offers a reliable and minimally invasive solution for achieving stable fracture fixation, promoting osteogenesis, and enabling early mobilization.
Case Report: A 27-year-old male sustained a Grade 1 compound comminuted fracture of the right tibia along with a proximal fibular fracture following a motorcycle accident. The patient was managed with an Ilizarov external fixator. The procedure provided stable fixation, facilitated bone regeneration, and supported early rehabilitation. The patient achieved full functional recovery and complete radiological union without complications. At 1-year follow-up, bone alignment and regeneration were excellent.
Conclusion: The Ilizarov ring fixation technique is an effective and dependable method for managing high-energy tibial fractures. It enhances bone healing, and promotes early functional recovery, making it a valuable tool in complex fracture management.
Keywords: Ilizarov technique, distraction osteogenesis, tibial fractures, ring fixator.
High-energy tibial fractures, especially those associated with soft-tissue injury, require meticulous planning for optimal outcomes [1,2]. Traditional fixation methods may not always be viable due to infection risks, poor bone quality, or extensive comminution [3]. The Ilizarov technique, which utilizes a circular external fixator, allows for gradual bone remodeling, alignment correction, enhanced stability, and early mobilization when applied appropriately [4,5]. This method offers advantages such as the generation of viable new bone through distraction osteogenesis and high union rates. This report describes in depth, a case of a young male patient with a shattered tibial fracture, treated successfully with Ilizarov fixation.
Distraction osteogenesis in Ilizarov fixation
Distraction osteogenesis is a biological process of new bone formation in response to a gradual mechanical stretching [6]. This principle, developed by Dr. Gavriil Ilizarov, is widely used for limb lengthening, deformity correction, and non-union treatment. The Ilizarov apparatus, a circular external fixator, applies controlled tension to stimulate bone regeneration while maintaining stability. The implant had been provided free of cost to the patient under a government scheme relieving the additional economic burden.
Biological stages of distraction osteogenesis
Latency phase (7–10 days)
Hematoma forms; mesenchymal stem cells differentiate into osteoblasts, chondrocytes, and fibroblasts.
Distraction phase
Gradual separation (0.5–1 mm/day) promotes fibrous interzone formation, angiogenesis, and early callus mineralization.
Consolidation phase (3–6 months)
Intramembranous ossification and corticalization occur; weight-bearing stimulates bone remodeling (Wolff’s Law).
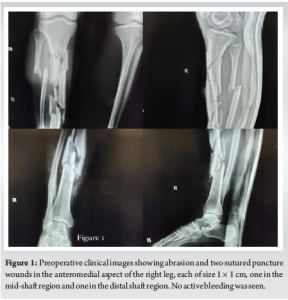
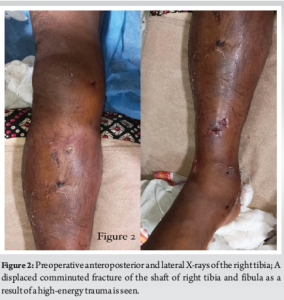
A 27-year-old male presented to the casualty with an open injury of his right leg following a traumatic fall from a motorcycle. On local examination, he had an abrasion and two puncture wounds of size 1 × 1 cm at the anteromedial aspect of the middle shaft and distal shaft of his right leg (Fig. 1) . No active bleeding or symptoms of compartment syndrome were found. The knee and ankle range of motions was painful with the absence of any distal neurovascular deficit. There were no other associated trauma. Pre-operative anteroposterior and lateral radiographs revealed a displaced and comminuted fracture of the shaft of the tibia and fibula (Fig. 2). The fracture was provisionally stabilized by an above-knee slab. Routine blood reports were normal.
Surgical procedure
After a thorough explanation regarding the surgical procedure, informed consent of the patient and his family were taken. Closed reduction of the tibial fracture was done under fluoroscopic guidance. Due to the comminuted nature of the fracture, internal fixation was deemed unsuitable, and a circular external fixator (Ilizarov apparatus) was selected to provide stable fixation while allowing for post-operative distraction osteogenesis.
Frame application
A three-ring Ilizarov frame was constructed using carbon fiber rings, tensioned stainless steel wires, and Schanz pins. The frame was configured to span both the tibial and fibular fractures to maintain alignment and permit bone regeneration.
Proximal fixation
Two olive wires were inserted transversely across the proximal tibial metaphysis, avoiding the joint line and neurovascular bundle. These were subsequently tensioned.
Distal fixation
Two additional wires were placed distal to the fracture, perpendicular to the shaft, ensuring bicortical purchase. A single Schanz pin was used in the distal tibia to augment fixation stability. Wires and pins were connected to the rings using Rancho cubes and cannulated bolts, and the construct was tensioned under fluoroscopy. Care was taken to preserve soft-tissue planes around the zone of injury.
Fracture reduction and alignment
The reduction was achieved by manipulation of the bone fragments through frame adjustments. Anatomical alignment was confirmed in anteroposterior and lateral planes using intraoperative fluoroscopy. Axial length, rotation, and coronal alignment were carefully restored. No additional soft-tissue procedures were done.
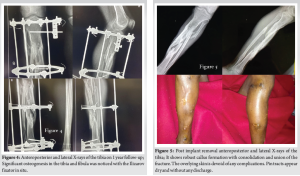
Post-operative protocol
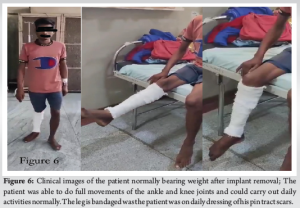
No intraoperative complications occurred. The limb was immobilized in the Ilizarov frame, and neurovascular status was intact post-surgery. Radiographs taken postoperatively confirmed proper alignment and frame positioning (Fig. 3). The distraction protocol was initiated after a latency period of 7 days, with gradual distraction of 1 mm/day in four increments (0.25 mm every 6 hrs). The patient was mobilized with partial weight-bearing on 2nd postoperative day to encourage functional recovery and stimulate callus formation. Radiographs after 1 year revealed substantial osteogenesis in both the tibia and fibula. There were no clinical or radiological signs of infection or hardware-related complications. The Ilizarov fixator was retained in situ to ensure complete bone consolidation (Fig. 4). The fixator was removed after 1 year from the initial Ilizarov fixation, following radiological confirmation of complete bone healing. Post-removal X-rays confirmed solid union without deformity (Fig. 5). The overlying skin was devoid of any complications. The patient was advised daily dressing for complete healing of the pin tract scars.

Functional recovery
The patient achieved a full range of motion in the right knee and ankle joints. He was able to bear weight without difficulty and resumed daily activities independently immediately after fixator removal (Fig. 6). At final follow-up after 1 month from implant removal, no residual pain or functional limitations were noted.
The Ilizarov method has demonstrated high success rates in treating complex tibial fractures, including open, comminuted, and segmental fractures. Its circular external fixator provides stable fixation, allowing for early mobilization and weight-bearing. Oztürkmen et al. performed Ilizarov surgery in 24 patients of segmental tibial fractures and had excellent outcome in 20 and good results in 4 patients in terms of bone assessment [7]. Ghimire et al. analyzed the clinical, radiological, and functional outcomes of the Ilizarov technique in 52 cases of high-energy tibial plateau fractures (Schatzker Types V and VI). It has been shown to be a safe, cost-effective, and efficient treatment method, yielding satisfactory outcomes [8]. When compared to internal fixation methods like intramedullary nailing, the Ilizarov technique offers distinct advantages, especially in cases with infection, bone loss, or soft-tissue compromise. While intramedullary nailing may provide faster recovery in certain scenarios, the Ilizarov method has a lower complication rate and is particularly effective in complex fracture patterns as per the comparative study conducted by Ramos et al. on 58 cases of tibial diaphyseal fractures [9]. In managing tibial bone defects, both the Ilizarov method and the Masquelet technique have shown comparable clinical outcomes. However, as per the report of Kanakaris et al., the Ilizarov method may offer advantages in specific contexts, such as larger defects or infected nonunions. In addition, the mean cost of the overall treatment in the case of an Ilizarov surgery was significantly lower than the Masquelet technique [10-13].
The Ilizarov technique remains an indispensable tool in the armamentarium of orthopedic trauma surgery. In the context of open, complex, and comminuted tibial fractures, this method offers distinct advantages over conventional internal fixation techniques. This case illustrates not only the biomechanical stability afforded by the circular fixator but also the biological efficacy of gradual tension-induced osteogenesis. The patient demonstrated timely and robust callus formation, progressive corticalization, and full radiographic union without secondary bone grafting or adjunct procedures. Furthermore, the preservation of limb alignment and early mobilization contributed to a swift and complete return to pre-injury functional status. Clinically, the use of Ilizarov fixation mitigated risks of infection, hardware failure, and malunion, all of which are heightened in complex high-energy tibial fractures. Radiologically, the consolidation observed over serial follow-ups highlighted the efficiency of the fixator. Final outcomes suggest that adherence to Ilizarov protocols yields excellent results. In conclusion, Ilizarov ring fixation in contemporary orthopedic practice should be considered a first-line strategy in select cases of severe tibial trauma, particularly where internal fixation is not feasible.
The Ilizarov technique is a powerful tool for managing complex, comminuted tibial fractures. Proper application of distraction osteogenesis principles using circular external fixation can achieve excellent fracture union and functional recovery without the need for bone grafting or additional interventions even in resource-limited settings.
References
- 1.Sen C, Kocaoglu M, Eralp L, Gulsen M, Cinar M. Acute treatment of segmental tibial fractures with the Ilizarov method. J Orthop Trauma 2004;18:150-7. [Google Scholar | PubMed]
- 2.Kumar A, Whittle AP. Treatment of complex tibial plateau fractures using Ilizarov technique. J Orthop Trauma 2005;19:340-5. [Google Scholar | PubMed]
- 3.Kocaoglu M, Eralp L, Sen C, Balci HI. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res 2006;449:222-9. [Google Scholar | PubMed]
- 4.Pugh KJ, Wolinsky PR, McAndrew MP, Johnson KD. Tibial fractures: The Ilizarov alternative. J Trauma 1992;33:316-23. [Google Scholar | PubMed]
- 5.Rozbruch SR, Segal K, Ilizarov S, Fragomen AT. Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma 2006;20:197-205. [Google Scholar | PubMed]
- 6.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res 1989;239:263-85. [Google Scholar | PubMed]
- 7.Oztürkmen Y, Karamehmetoğlu M, Karadeniz H, Azboy I, Caniklioğlu M. Acute treatment of segmental tibial fractures with the Ilizarov method. Injury 2009;40:321-6. [Google Scholar | PubMed]
- 8.Ghimire A, Devkota P, Bhandari KK, Kharel Y, Pradhan S. Ilizarov ring external fixation for complex tibial plateau fractures. Rev Bras Ortop (Sao Paolo) 2021;57:667-74. [Google Scholar | PubMed]
- 9.Ramos T, Ericsson BI, Karlsson J, Nistor L. Ilizarov external fixation or locked intramedullary nailing in diaphyseal tibial fractures: A randomized, prospective study of 58 consecutive patients. Arch Orthop Trauma Surg 2014;134:793-802. [Google Scholar | PubMed]
- 10.Kanakaris NK, Harwood PJ, Mujica-Mota R, Mohrir G, Chloros G, Giannoudis PV. Treatment of tibial bone defects: Pilot analysis of direct medical costs between distraction osteogenesis with an Ilizarov frame and Masquelet technique. Eur J Trauma Emerg Surg 2023;49:951-64. [Google Scholar | PubMed]
- 11.Bell WH, Guerrero CA. Distraction Osteogenesis of the Facial Skeleton. Hamilton (ON): BC Decker Inc.; 2007. Available from: https://pubmed.ncbi.nlm.nih.gov/00000011 [Last accessed on 2007]. [Google Scholar | PubMed]
- 12.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 1990;250:81-104. [Google Scholar | PubMed]
- 13.Kocaoglu M, Eralp L, Balci HI. Ilizarov segmental bone transport of infected tibial nonunions with large bone defects. Clin Orthop Relat Res 2006;449:222-9. [Google Scholar | PubMed]