Both PFNA-II and TFN are equally effective in the treatment of unstable intertrochanteric femur fractures, with no clear superiority of one over the other. Clinical and functional outcomes, as well as complication rates, are comparable between the two. Implant selection should be tailored to individual patient factors and surgeon familiarity.
Dr. Ismail Pandor, Senior Resident, Department Of Orthopaedics, Krishna Vishwa Vidhyapeeth,Karad,India. Email: i.pandor07@gmail.com
Introduction: Intertrochanteric femur fractures are among the most common injuries in the elderly population and represent a major public health issue. Treatment aims to achieve stable fixation that allows early mobilization and minimizes complications. The choice of implant plays a critical role in clinical outcomes, particularly in unstable fracture patterns.
Objectives: The aim of this study was to compare the intraoperative parameters, functional outcomes, union times, and complications between proximal femoral nail anti-rotation-II (PFNA-II) and trochanteric femur nail (TFN) in patients with unstable intertrochanteric femur fractures.
Materials and Methods: A prospective, randomized, and comparative study was conducted in a tertiary care center over a period of 18 months. One hundred patients aged 50–85 years with Boyd and Griffin type III fractures were divided into two groups. Group A (n = 50) was treated using TFN, while Group B (n = 50) received PFNA-II. Surgical techniques, post-operative care, and rehabilitation protocols were standardized. Data on operative time, intraoperative blood loss, union duration, Harris Hip scores (HHS), and complications were collected and statistically analyzed.
Results: The PFNA-II group had shorter operative times (Mean 65.5 min. vs. 71.5 min) and less blood loss (253 ± 36.4 mL vs. 275 ± 35.1 mL) than the TFN group. Average union time was similar between groups. Mean HHS at 6 months was higher in the PFNA-II group (67.83 ± 8.05) than the TFN group (71.72 ± 7.45), though the difference was not statistically significant. PFNA-II also showed a lower incidence of implant-related complications.
Conclusion: PFNA-II offers certain intraoperative advantages and trends toward better functional outcomes and fewer complications, but the differences with TFN were not statistically significant. Both implants are viable for the treatment of unstable intertrochanteric fractures.
Keywords: Intertrochanteric fracture, proximal femoral nail anti-rotation-II, trochanteric femur nail, functional outcome, intramedullary fixation.
Hip fractures, particularly intertrochanteric fractures, constitute a growing healthcare burden due to increased life expectancy and age-related osteoporosis. Globally, approximately 1.6 million hip fractures occur annually, and this number is projected to rise to over 6 million by 2050. In India, the incidence of hip fractures has also increased significantly, primarily among elderly women [1,2].
Intertrochanteric fractures are extracapsular femoral fractures located between the greater and lesser trochanters. These fractures are commonly classified using the Boyd and Griffin system and the AO/OTA classification, with unstable patterns posing greater management challenges. These injuries necessitate operative treatment due to their poor prognosis with conservative management [3,4].
The treatment of intertrochanteric fractures has evolved from traction to dynamic hip screws and more recently, to intramedullary devices such as the PFN, trochanteric femur nail (TFN), and proximal femoral nail anti-rotation (PFNA). While TFN provides dual screw fixation for rotational control, PFNA-II incorporates a single helical blade designed to offer improved purchase in osteoporotic bone and reduce implant migration and cut-out [5,6].
Despite numerous studies comparing these devices, consensus remains elusive regarding their superiority in unstable fractures [7]. This study aims to compare PFNA-II and TFN in terms of functional outcome, surgical parameters, and post-operative complications, although both PFNA-II and TFN are widely used for unstable intertrochanteric fractures, there is no clear consensus on which implant is superior. Existing studies report comparable outcomes with variations in specific complications and surgical ease. Their differing design features, such as blade versus screw fixation, contribute to ongoing debate. This clinical uncertainty justifies equipoise and forms the basis for conducting a direct comparative study [3,4,5].
Study design and setting
This prospective, randomized, and comparative study was conducted in the department of orthopedics at a tertiary care teaching hospital (Krishna Vishwa Vidhyapeeth) from February 2021 to June 2022 after the Institutional Ethics Committee approval.
Participants were randomly assigned using sealed envelope technique into:
- Group A: TFN (n = 50)
- Group B: PFNA-II (n = 50).
Sample size
The sample size was calculated based on the expected difference in functional outcomes (e.g., Harris Hip score [HHS] or surgical time) between the PFNA-II and TFN groups. Assuming a significance level (α) of 0.05 and a power (1−β) of 80%, we used effect size estimates from prior studies (e.g., Sharma et al., 2020; Kashid et al., 2019) that reported a mean difference of approximately 5–7 points in outcome scores. Based on this, a minimum of 50 patients per group was determined to be adequate to detect statistically meaningful differences. Adjustments were also made for potential dropouts and follow-up loss.
Randomization
Allocation concealment was ensured using the sealed opaque envelope technique, with envelopes prepared and numbered by an independent staff member not involved in the study. Envelopes were opened only after patient enrollment. Due to the surgical nature of the intervention, blinding of surgeons and patients was not feasible. However, outcome assessment relied on objective measures such as the HHS and radiographic union to reduce bias.
Inclusion criteria
- Patients aged 50–85 years
- Boyd and Griffin type III unstable intertrochanteric fractures
- Presenting within 1 week of injury
- Medically fit for surgery.
Exclusion criteria
- Pathological fractures
- Previous ipsilateral hip surgery
- Polytrauma
- Associated femoral shaft fractures
- Non-ambulatory status before injury.
Surgical technique
Under spinal or general anesthesia, patients were placed in the supine position on a fracture table. Closed reduction was achieved under fluoroscopic guidance. Standard operative techniques for TFN and PFNA-II were followed. All procedures were performed by experienced surgeons. Prophylactic antibiotics were administered preoperatively and continued postoperatively.
Post-operative protocol
Patients were encouraged to begin mobilization from post-operative day 1. Weight-bearing was initiated based on fracture stability and radiological progress. Follow-up evaluations were conducted at 6 weeks, 3 months, and 6 months.
Outcome measures
- Operative time (minutes)
- Intraoperative blood loss (mL)
- Time to radiological union (weeks)
- HHS
- Post-operative complications.
Statistical analysis
Data were analyzed using the Statistical Packages for the Social Sciences software version 25. Descriptive statistics included mean, standard deviation, and percentage. Student’s t-test and Chi-square test were used to compare quantitative and categorical variables respectively. P < 0.05 was considered statistically significant.
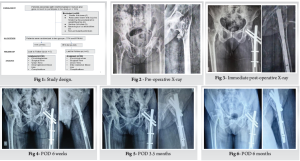
STUDY DESIGN:
Following algorithm was followed for enrollment,allocation ,followup and analysis as shown in fig 1.
Study design (Fig. 1)
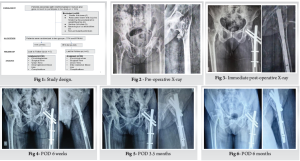
This prospective randomized study included 120 patients with intertrochanteric femur fractures, of whom 100 were eligible after excluding cases with stable fractures, severe comorbidities, and non-ambulatory status. Patients were randomly assigned into two groups—TFN and PFNA-II (n=50 each)—and assessed for functional outcome, surgical time, union time, intraoperative blood loss, and complications, with no loss to follow-up as shown in fig 1.
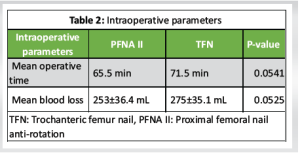
The age of the patients in both groups were compared. The age groups varied from 52 years to 75 years with the mean age of 60 years in patients treated with PFN A II. The age groups varied from 51 years to 67 years with the mean age of 58.2 years in patients treated with TFN. Among the 100 patients, 55 patients were males and 45 were females. Right side was common in our study. All cases were Boyd and Griffin type III (unstable) fractures (Table 1). No significant differences in clinical outcomes or complication rates were observed with respect to age, gender, or side of fracture. Both PFNA-II and TFN performed consistently across these demographic subgroups. This indicates that implant efficacy was not influenced by baseline patient characteristics.
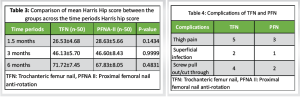
Among 100 cases in PFNA-II group operated patients, the average time of surgery is 65.5 min and among those who were operated with TFN that the average was 71.5 min. The average intraoperative blood loss in PFN A II patients was 238 mL and in TFN patients was 300 mL (Table 2).
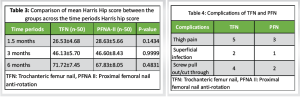
The mean HHS for patients of TFN and PFNA-II are not statistically significant (P > 0.05), as depicted in Table 3.
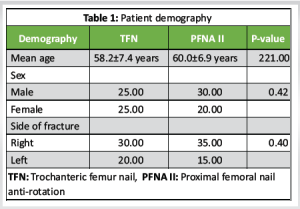
Time for radiological union was evaluated in this study using plain radiographs at regular follow-up and, in our study for TFN, it was 13.9 ± 1.54 weeks and for PFNA-II, it was 12.4 ± 2.9 weeks time taken for radiological union of fracture.(Fig 2-11)
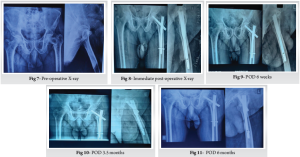
The incidence of anterior and lateral thigh pain requiring the use of oral analgesics to relieve the pain at 6-month post-operative period were recorded and, three patients in PFN A II group and five patients in TFN group had this complication. There were two cases of superficial infection in patients operated with TFN and one in patients operated with PFNA-II (Case 1 Image).
The incidence of screw pull out/cut through resulting in biomechanical failure of the implant at 6-month post-operative period was recorded and out of 100 patients, two patients in PFNA-II group and four patients in TFN group had this complication. Comparison between the two groups is shown in Table 4.
Unstable intertrochanteric fractures present a treatment challenge, particularly in elderly patients with osteoporotic bone. Traditional fixation methods like sliding hip screws often fail in unstable patterns due to poor rotational stability and risk of varus collapse. Cephalomedullary nails, including TFN and PFNA-II, offer biomechanical advantages, better load sharing, and improved fixation in such scenarios [5,8,9]. PFNA-II’s helical blade enhances bone purchase, while TFN provides dual screw stability [6,10]. Parker and Handoll’s review also support the biomechanical superiority of intramedullary nails over extramedullary implant [5]. Despite advancements, post-operative complications and functional limitations persist. This study compares TFN and PFNA-II in terms of intraoperative parameters, complications, and functional outcomes, aiming to clarify the optimal implant for unstable intertrochanteric fractures. In our study, the trochanteric fixation nail and proximal femoral nail are being tested and studied in view of an era of newer emerging implants.
In this study, the mean age of patients of TFN and PFNA-II was 58.2 ± 7.4 years and 60.0 ± 6.9 years, respectively. More than half of patients of PFN (56.7%) and 43.3% of PFNA were male. There was no significant (P > 0.05) difference in age and gender between the groups. Similar results were observed in a study by Kashid and Waghchoure [11], in which the mean age of patients in TFN and PFNA-II was 64.36 ± 8.28 years and 65.36 ± 8.66 years, respectively, which did not differ significantly.
This study demonstrated that the operative time was 71.5 min among patients of TFN and 65.5 min among patients of PFNA-II with no significant difference between the groups. Bajpai et al. [12] found that the two groups were also similar in operation time (screw PFN, 85.91 min; helical blade PFN group 83.91 min; P = 0.43) with no significant difference between the two.
In our study, the average blood loss for TFN cases was 275 ± 35.1 mL and for PFNA-II was 253 ± 36.4 mL. Although the value for TFN was higher, there is no significant statistical difference between both the implants.
The average union time in our study for TFN was 13.9 ± 1.54 weeks and for PFNA-11 was 12.4 ± 2.9 weeks. This result shows no significant statistical difference between both the implants for union time of fracture.
There was no significance (P > 0.05) in HHS between the groups across the time periods in patients of PFNA-II than TFN [13]. Bojan AJ et al. [10] also reported similar finding in which the average HHS obtained at final follow-up was identical in the two groups of patients – 75.37 for the TFN group and 78.85 for the PFNA-II group.
The complications that were observed on included the prolonged anterior and lateral thigh pain screw pull out leading biomechanical failure and infection. There were three cases of thigh pain in PFNA-II and five in TFN group. Superficial infection was noted in one case of PFNA-II and two case of TFN. Implant failure was seen in two patients of PFN A-II and four cases of TFN at end of follow-up. Cases operated with TFN that failed showed a significant lower singhs index which could indicate osteoporosis playing a role in the failure of TFN. Whereas failed cases of PFN A-II did not show lower singhs index; hence, its failure could be attributed to improper reductions or screw placements [14] .
Strengths
This study was a prospective, randomized, and comparative trial, which minimizes selection bias and enhances the validity of the findings. A relatively large sample size (n = 100) with standardized surgical and rehabilitation protocols adds to the reliability and reproducibility of the results.
Limitations
Blinding was not feasible due to the nature of surgical interventions, which may introduce some performance or detection bias. In addition, the short follow-up duration (6 months) may not capture long-term complications such as implant failure or late functional decline.
PFNA-II demonstrated better functional outcomes, shorter operative times, less blood loss, and a lower complication rate compared to TFN although not statistically significant. Both PFNA-II and TFN are equally effective in the treatment of unstable intertrochanteric femur fractures, with no clear superiority of one over the other. Both implants are reliable and effective, and implant choice should depend on patient profile, bone quality, and surgeon experience.
In the management of unstable intertrochanteric femur fractures, both PFNA-II and TFN are reliable intramedullary fixation options. While PFNA-II offers certain intraoperative and early post-operative advantages, implant selection should ultimately be individualized based on patient-specific factors such as bone quality, anatomical considerations, and surgeon expertise. Optimal outcomes are achieved not solely by implant choice but by meticulous surgical technique and comprehensive patient care.
References
- 1.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006;17:1726-33. [Google Scholar | PubMed]
- 2.Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop 2011;45:15-22. [Google Scholar | PubMed]
- 3.Boyd HB, Griffin LL. Classification and treatment of trochanteric fractures. Arch Surg (1920) 1949;58:853-66. [Google Scholar | PubMed]
- 4.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium-2007: Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 2007;21:S1-133. [Google Scholar | PubMed]
- 5.Haidukewych GJ. Intertrochanteric fractures: Ten tips to improve results. J Bone Joint Surg Am 2009;91:712-9. [Google Scholar | PubMed]
- 6.Simmermacher RK, Ljungqvist J, Bail H, Hockertz T, Vochteloo AJ, Ochs U, et al. The new proximal femoral nail antirotation (PFNA) in daily practice: Results of a multicentre clinical study. Injury 2008;39:932-9. [Google Scholar | PubMed]
- 7.Zhang S, Zhang K, Li Q. A meta-analysis of proximal femoral nail anti-rotation versus dynamic hip screw in intertrochanteric fractures of the elderly. J Orthop Surg Res 2014;9:75. [Google Scholar | PubMed]
- 8.Takigami I, Matsumoto K, Ohara A, Yamanaka K, Naganawa T, Ohashi M, et al. Treatment of trochanteric fractures with the PFNA (Proximal femoral nail antirotation) nail system - report of early results. Bull NYU Hosp Jt Dis 2008;66:276-9. [Google Scholar | PubMed]
- 9.Babhulkar S, Babhulkar S. Management of trochanteric fractures. Indian J Orthop 2006;40:210-8. [Google Scholar | PubMed]
- 10.Bojan AJ, Beimel C, Speitling A, Taglang G, Ekholm C, Jonsson A. 3066 consecutive gamma nails. 12 years experience at a single centre. BMC Musculoskelet Disord 2010;11:133. [Google Scholar | PubMed]
- 11.Kashid RM, Waghchoure A. Comparative study of PFNA2 and TFN in intertrochanteric fractures. Int J Orthop Sci 2022;8:11-4. [Google Scholar | PubMed]
- 12.Bajpai S, Tiwari A, Tripathi AK. A comparative study between proximal femoral nail antirotation (pfna) and proximal femoral nail (pfn) in the treatment of intertrochanteric fractures of the femur. Int J Orthop Sci 2022;8:45-9. [Google Scholar | PubMed]
- 13.Sahin EK, Demirel M, Karadeniz H. PFNA vs. TFN in treating intertrochanteric fractures: A comparison of clinical and radiological outcomes. Eur J Orthop Surg Traumatol 2022;32:21-8. [Google Scholar | PubMed]
- 14.Zhou ZY. Comparative study of PFNA-II and DHS for treatment of intertrochanteric fractures. Chin J Traumatol 2015;18:273-7. [Google Scholar | PubMed]











