The Gustilo-Anderson Grade and the time-lag to surgical debridement are the two most critical determinants of non-union and infection rates in open tibial shaft fractures, underscoring the necessity of urgent, grade-specific management.
Dr. Hardik Kharbanda, Consultant Orthopaedics, Vidisha - 464001, Madhya Pradesh, India. E-mail: shardikkharbanda4@gmail.com
Introduction: Open (compound) fractures of the tibia and fibula diaphysis remain a major challenge in orthopedic trauma due to their high risk of infection, non-union, and chronic osteomyelitis. Effective management requires timely debridement, stable fixation, and meticulous soft-tissue handling . This study aimed to analyze the complication rates and identify the major determinants influencing outcomes in patients with open tibial fractures treated at a tertiary care center. .
Materials and Methods: A retrospective analysis was conducted on 138 consecutive patients with Gustilo-Anderson Grade I-IIIB open fractures of the tibia fibula diaphysis. Data recorded included demographics, Gustilo grade, definitive treatment type, presence of comorbidities, and time lag to surgery. Outcomes evaluated were fracture union, osteomyelitis, soft-tissue healing time, Barthel index, and duration of hospital stay. Statistical analysis included Chi-square/Fisher’s exact tests, Independent Sample t-tests, and multivariate logistic regression, with P < 0.05 considered significant.
Results: The mean age of patients was 35.3 ± 14.7 years, with 81.2% males. The overall non-union rate was 22.5%, and osteomyelitis occurred in 18.1%. The Gustilo-Anderson grade was the most significant determinant of non-union and complications (P < 0.001), with rates increasing from 3.3% in Grade I to 66.7% in Grade IIIB. The mean delay to definitive treatment was 5.2 days in non-union cases versus 4.2 days in union cases (P = 0.02). Intramedullary nailing (IMN) showed the highest union rate (91.5%) and the lowest infection rate (8.5%), whereas external fixation (Ilizarov/limb reconstruction system) was associated with higher complication rates, reflecting higher injury grades.Diabetes mellitus was significantly correlated with non-union (P = 0.001).
Conclusion: The severity of initial soft-tissue injury and delay to definitive treatment are the two most critical determinants of outcome in open tibia fibula diaphyseal fractures. Gustilo-Anderson grade remains the only independent predictor of both non-union and infection. Early debridement, stable fixation (preferably with IMN in lower-grade injuries), and comprehensive soft-tissue management are essential to minimize complications and improve functional recovery.
Keywords: Open fracture, tibial diaphysis, Gustilo-Anderson classification, non-union, osteomyelitis, intramedullary nailing
Open (compound) fractures of the tibial diaphysis are among the most severe injuries encountered in orthopedic trauma. They involve disruption of both bone and overlying soft-tissues, resulting in direct communication between the fracture site and the external environment [1]. These injuries are often the consequence of high-energy mechanisms such as road traffic accidents or industrial trauma and are frequently accompanied by extensive soft-tissue damage, contamination, and periosteal stripping [1,4]. The combination of skeletal and soft-tissue injury significantly increases the risks of infection, delayed union, non-union, and chronic osteomyelitis, leading to substantial functional morbidity (Table 1-5, Graph 1-4).
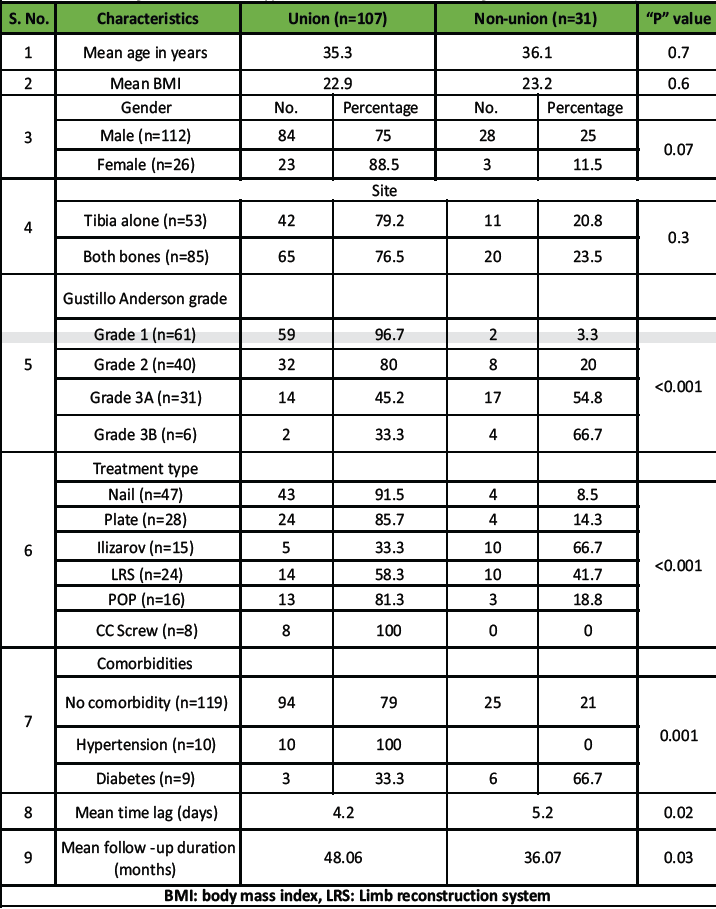
Table 1: Association of fracture union with patient and clinical characteristics (includes demographics, Gustilo grade, treatment type, comorbidities, and time lag vs. union/non-union)
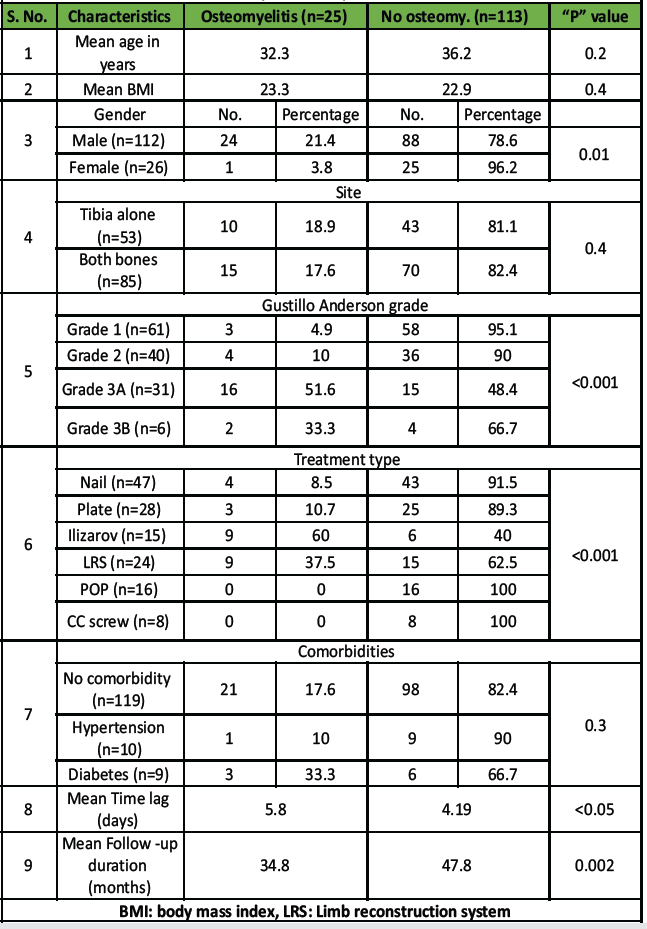
Table 2: Association of osteomyelitis with patient and clinical characteristics
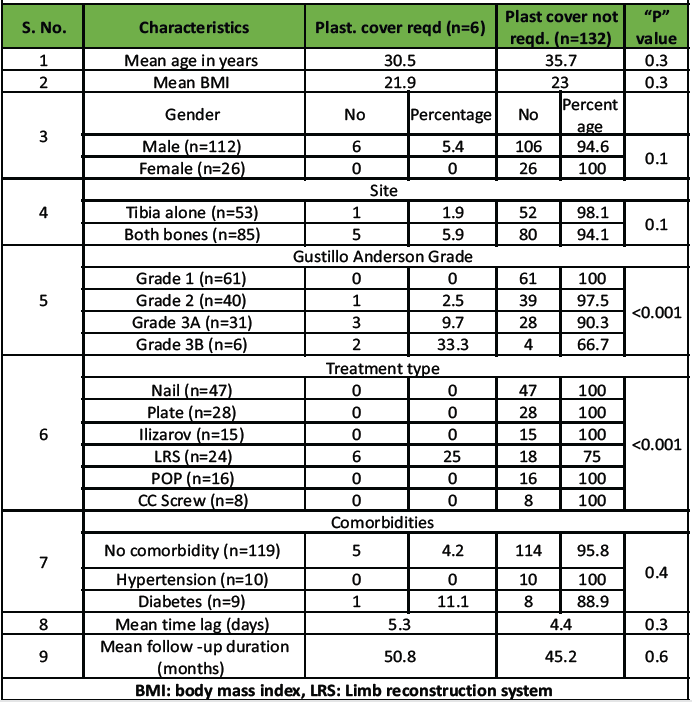
Table 3: Association of plastic cover requirement with patient and clinical characteristics
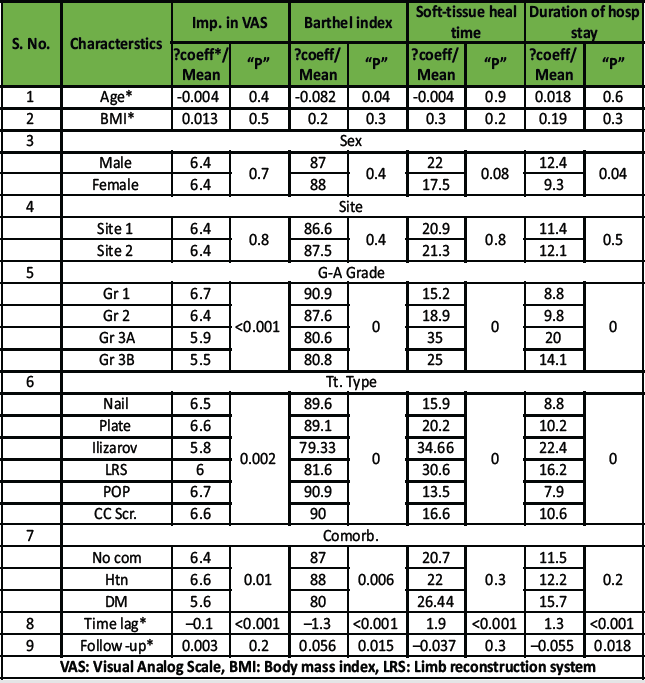
Table 4: Association of parametric outcomes (improvement in VAS, Barthel index, so-fttissue healing time, duration of hospital stay) with patient/clinical characteristics
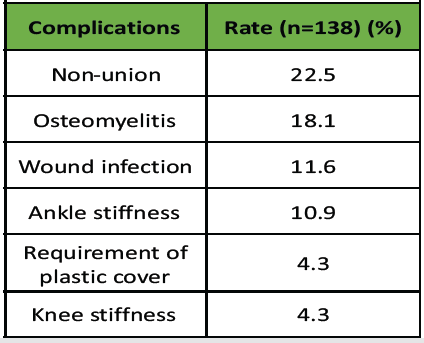
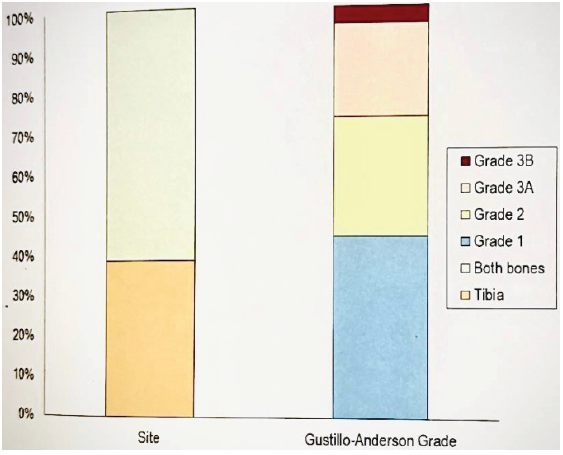
Table 5: Complication and outcome rates
Graph 1: mean age and body mass index of the study population.
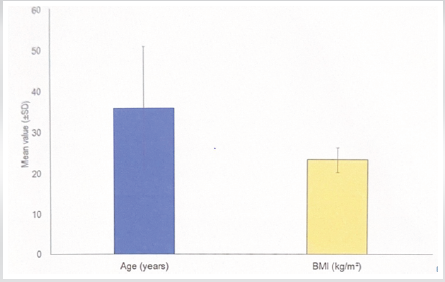
Graph 2: Gender and comorbidity status of study population.
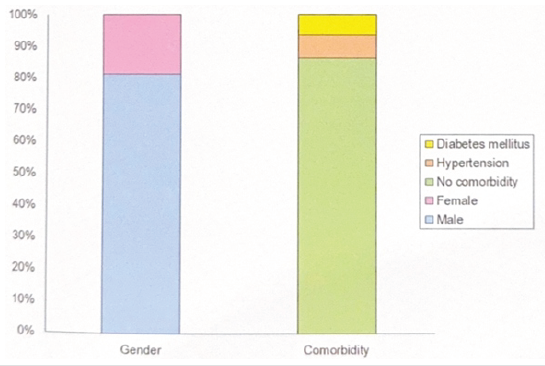
Graph 3: Site and grade of compound fracture.
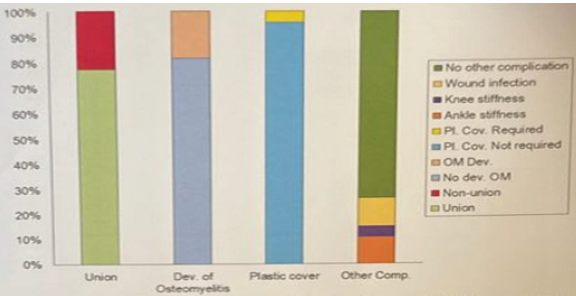
Graph 4: Outcome variables (union, development of osteomyelitis, requirement of plastic cover, and other complications).
Open fractures of the tibia account for approximately 3–5% of all fractures, but they constitute a disproportionately high share of post-traumatic complications [1]. The unique subcutaneous anatomy of the tibia renders it particularly vulnerable to soft-tissue compromise and infection [3,5]. Successful management, therefore, requires a multidisciplinary approach, integrating principles of early and thorough debridement, broad-spectrum antibiotic coverage, stable skeletal fixation, and early soft-tissue reconstruction to restore limb function and minimize long-term disability (Tables 1–4, Graphs 1–3) [2,5]. The Gustilo-Anderson classification remains the most widely accepted system for grading the severity of soft-tissue injury and guiding management [3]. Several studies have consistently demonstrated that increasing Gustilo grade correlates strongly with higher rates of infection, non-union, and poorer functional outcomes [4,6]. Nevertheless, ongoing debate persists regarding the relative influence of injury severity versus time to debridement, with some authors emphasizing the “six-hour rule,” while others suggest that the quality and timing of soft-tissue management may be more crucial determinants of prognosis [1,4]. The reported rates of non-union (22.5%) and osteomyelitis (18.1%) continue to be substantial, even with modern fixation techniques (Tables 5–6, Graph 4). The timing of surgical intervention, choice of fixation method, and presence of systemic comorbidities such as diabetes mellitus may further modulate these outcomes [1,3]. While intramedullary nailing (IMN) is recognized as the gold standard for lower-grade open fractures, higher-grade injuries often necessitate staged procedures with external fixation and plastic coverage due to soft-tissue loss and contamination (Table 6, Graph 6) [2,5].
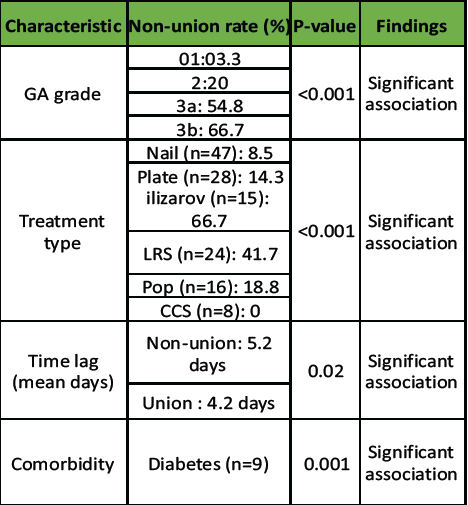
Table 6: Key determinants of fracture union (Union n=107, Non-union n=31)
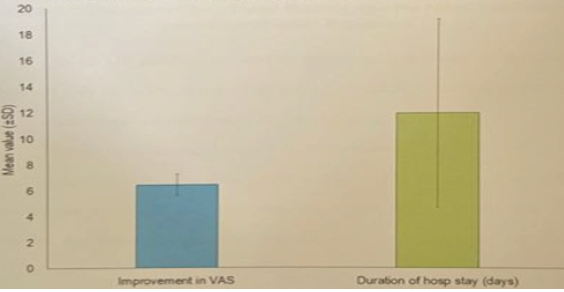
Graph 5: Improvement in Visual Analog Scale score and duration of hospital stay.
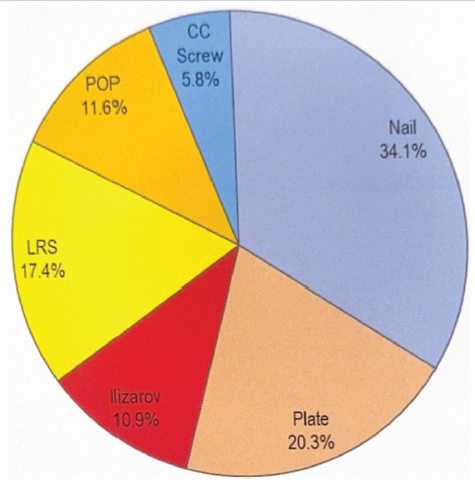
Graph 6: Showing types of treatment.
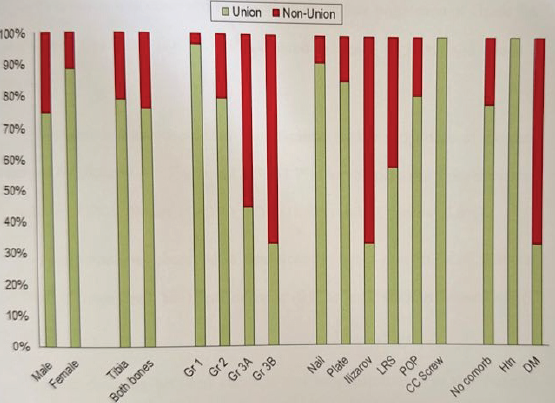
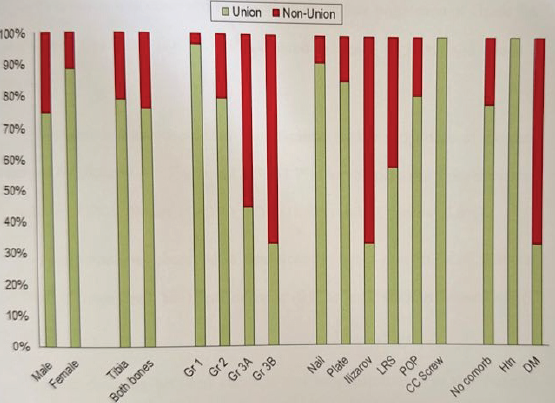
Graph 7: Association of fracture union with patients and clinical characteristics.
Given these considerations, the present study was undertaken to evaluate the complication rates and determinants of outcome in patients with open fractures of the tibial diaphysis managed at a tertiary care center (Tables 1–6, Graphs 1–7) [1–6]. Specifically, the study aimed to analyze the influence of Gustilo-Anderson grade, time lag to definitive treatment, type of fixation, and comorbidities on union rates, infection rates, and functional recovery, thereby providing insights for improving evidence-based management protocols in such complex injuries.
Study design and setting
This was a retrospective study conducted at the Department of Orthopedics in tertiary care center of India.
Duration of study
The study spanned 24 months.
Sampling frame and criteria
The study included patients with compound fractures of the leg (tibia/fibula/both).
Inclusion criteria
All patients with Gustilo-Anderson Grade I, II, IIIA, or IIIB fractures treated definitively at the center. Only patients who were directly admitted to and completed their follow-up at the same center were included.
Exclusion criteria
- Simple fracture
- Patients with Grade IIIC fracture (Gustilo-Anderson classification)
- Compartment syndrome and neurovascular damage
- Patients with knee dislocation
- Patients initially managed in other facilities or who continued their treatment and/or follow-up in other hospitals.
Methodology
Data of all patients with compound fractures of both bones of the leg fulfilling the inclusion criteria were analyzed. Demographic details, site and type of fracture, Gustilo-Anderson grade, duration since injury, treatment modality, antibiotics used, time from admission to surgery, and associated comorbidities were recorded. Only patients treated under the standard protocol at the centre — including prophylactic antibiotics for at least 3 days, emergency debridement, skeletal stabilization, and primary wound closure when indicated — were included. The final sample size was 138 patients. Outcome parameters included bone union, osteomyelitis, wound healing time, pain (Visual Analog Scale [VAS]), Barthel index for functional outcome, hospital stay duration, and other complications. Bone healing was assessed clinically and radiographically. Non-union was defined as failure to unite at 9 months with no radiological progression for 3 months. Osteomyelitis was diagnosed in patients presenting with fever, local redness, discharge, swelling, or limb dysfunction, confirmed by positive microbiological culture, and managed as per standard protocols. Pain assessment was done using the 10-point VAS, where 0 indicates no pain and 10 denotes the worst pain. Functional outcome was evaluated using the Barthel index, which assesses 10 parameters of activities of daily living such as feeding, mobility, dressing, toileting, and bathing, with higher scores reflecting greater independence.
The management of open tibia fibula diaphyseal fractures remains one of the most demanding challenges in orthopedic trauma due to the high incidence of soft-tissue injury, contamination, and vascular compromise [3,5]. In this retrospective study of 138 patients, we found that both the severity of the initial injury – quantified by the Gustilo-Anderson grade – and the time lag to definitive management were the most significant determinants of clinical and functional outcomes. The overall non-union rate of 22.5% and osteomyelitis rate of 18.1% observed in this study are within the range reported in previous literature, reflecting the persistent morbidity associated with these injuries despite modern surgical techniques. Our findings demonstrate a clear, statistically significant relationship between increasing Gustilo-Anderson grade and both non-union and infection rates. The non-union rate increased from 3.3% in Grade I fractures to 66.7% in Grade IIIB, mirroring the progressive escalation in soft-tissue destruction, periosteal stripping, and bacterial contamination associated with higher-grade injuries. This pattern aligns with prior meta-analyses such as Tian et al. (2020), which highlighted the Gustilo-Anderson grade as the most reliable predictor of delayed union or non-union. Similarly, Ukai et al. (2020) identified the extent of soft-tissue injury as a key determinant of deep infection in Type III fractures. Collectively, these findings reinforce the importance of early, meticulous soft-tissue management in improving outcomes [4,5]. The time lag between injury and surgical intervention was another significant factor influencing healing. In our series, non-union was significantly more common when the delay exceeded 4 days, with a mean lag of 5.2 days in non-union cases compared to 4.2 days in those that achieved union (P = 0.02). This observation supports the findings of Lack et al. (2015) [10] who emphasized that prolonged delays before initial debridement were associated with higher infection and amputation rates, particularly in Type III injuries. However, as also suggested by Li et al. (2020), the impact of timing may be secondary to the extent of soft-tissue damage – meaning that the severity of injury remains the dominant prognostic factor, while time to debridement is a modifiable contributor [1,2]. When evaluating the type of fixation, IMN demonstrated the best outcomes, with a union rate of 91.5% and the lowest osteomyelitis rate (8.5%). These findings are consistent with multiple contemporary studies supporting IMN as the most appropriate mode of fixation for Gustilo Grade I and II injuries, providing biological fixation with preservation of periosteal blood supply. In contrast, external fixation devices, particularly Ilizarov and limb reconstruction system (LRS), were associated with higher non-union and infection rates in our study. This observation is likely influenced by case selection bias, as these methods were primarily used in high-grade (III A/III B) injuries with severe contamination, bone loss, or soft-tissue compromise. Studies by Singh et al. (2020), Debnath et al. (2020), and Kapila et al. (2018) have similarly documented that while external fixators are invaluable for stabilization and infection control in complex injuries, their outcomes are inherently limited by the severity of the initial insult [5,6,7]. Comorbidities, particularly diabetes mellitus, played a significant role in impairing fracture healing. Diabetic patients in our series had a non-union rate of 66.7% (P = 0.001). Chronic hyperglycemia leads to microvascular compromise, impaired osteoblast function, and reduced resistance to infection – all of which adversely affect bone repair. This finding underscores the need for strict metabolic control and individualized surgical planning in patients with systemic illness. Functional outcomes, assessed by the Barthel index, soft-tissue healing time, and duration of hospital stay, further reflected the severity-dependent pattern of recovery. Patients with Grade IIIA-IIIB injuries demonstrated significantly lower Barthel index scores (mean 80.6–80.8) compared to Grade I fractures (90.9, P = 0.00). The mean soft-tissue healing time was 35 days for Grade IIIA versus 15.2 days for Grade I fractures, while hospital stay was markedly prolonged (20 days vs. 8.8 days, P = 0.00). These functional results highlight that beyond bony union, the extent of soft-tissue injury has a profound and prolonged impact on patient recovery, corroborating the conclusions of Vasanad et al. (2016) and Singla et al. (2016) [8,9]. Multivariate logistic regression in this study confirmed that the Gustilo-Anderson grade was the sole independent determinant for both non-union (odds ratio [OR]: 5.604, P = 0.001) and other complications (OR: 1.779, P = 0.017). This emphasizes the dominant prognostic role of initial soft-tissue injury severity, surpassing other clinical variables. From a clinical standpoint, this finding reinforces that timely and aggressive debridement, appropriate selection of fixation, and early soft-tissue cover remain the cornerstones of open fracture management. While traditional teaching advocated for the “six-hour rule” for open fracture debridement, recent evidence suggests that the quality of debridement and soft-tissue viability are more critical than exact timing. Our results support this evolving view: although delays beyond four days were detrimental, the grade of injury remained the overriding determinant. Thus, early intervention within the first few days, accompanied by meticulous debridement, remains essential to optimize union rates and minimize infection. This study has several limitations. First, due to its retrospective design, it is inherently susceptible to data recording errors and lacks control over potential confounding variables, thereby limiting the ability to establish causal relationships. Secondly, being a single-center study conducted at a tertiary care hospital, the findings may not be generalizable to other institutions with different patient populations, resources, or treatment protocols. In addition, there was an unequal distribution of fracture grades, with a predominance of lower-grade (Grade I-II) injuries and relative underrepresentation of severe (Grade IIIB) cases, which may have introduced sampling bias. Furthermore, follow-up parameters were limited, as long-term outcomes such as quality of life, return to work, and chronic pain were not evaluated beyond the basic functional scoring. Finally, several potential confounding factors, including smoking habits, nutritional status, and microbiological variations, were not assessed, which could have influenced both infection rates and fracture healing outcomes. Nonetheless, the sample size of 138 cases and the comprehensive analysis of both bony and functional outcomes provide strong evidence to support the current treatment paradigms. This study reinforces that the initial soft-tissue injury severity is the most powerful predictor of outcome in open tibial diaphyseal fractures. The time lag to definitive treatment acts as an important modifiable factor, and IMN remains the most reliable fixation method in lower-grade injuries. Conversely, high-grade (III A/B) injuries require an individualized, staged approach with early plastic coverage and possibly external fixation. Future prospective studies with longer follow-up and standardized functional scoring would help refine management protocols and improve patient outcomes.
A total of 138 patients fulfilling the inclusion criteria were included in the final analysis (Table 1).
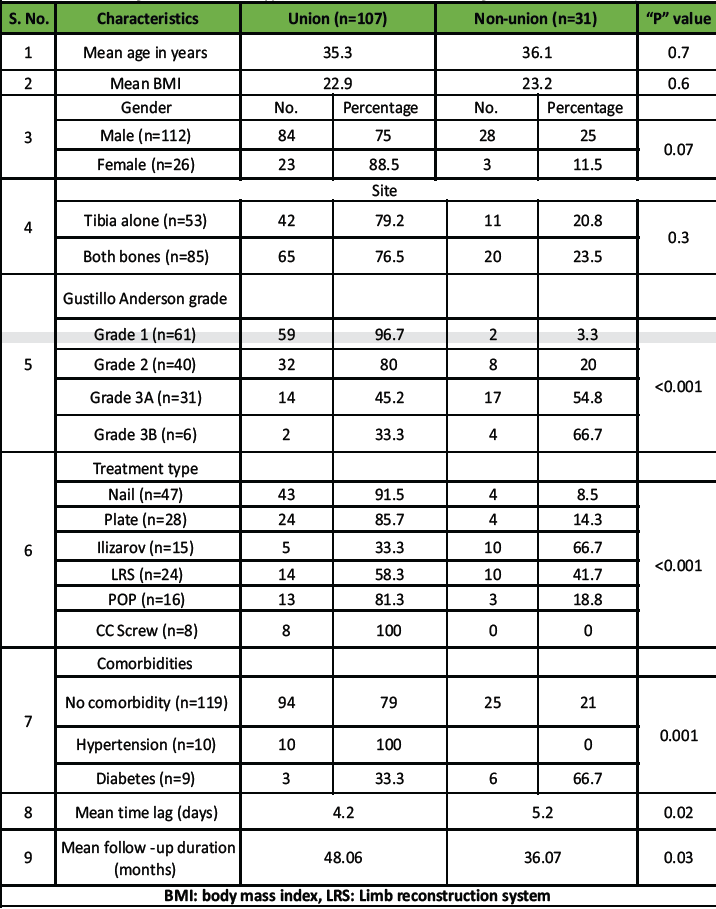 Table 1: Association of fracture union with patient and clinical characteristics (includes demographics, Gustilo grade, treatment type, comorbidities, and time lag vs. union/non-union)
Table 1: Association of fracture union with patient and clinical characteristics (includes demographics, Gustilo grade, treatment type, comorbidities, and time lag vs. union/non-union)
The mean age of the patients was 35.3 ± 14.7 years, with a clear male predominance (81.2%). The mean body mass index was 22.9 ± 2.9 kg/m2. Regarding comorbidities, 9 patients (6.5%) were diabetic, 10 patients (7.2%) were hypertensive, while 119 patients (86.2%) had no comorbidities. Most injuries (61.6%) involved both the tibia and fibula, and the mean time lag between fracture and initiation of treatment was 4.4 ± 2.15 days. According to the Gustilo–Anderson classification, 44.2% of fractures were Grade I, 29.0% were Grade II, 22.5% were Grade IIIA, and 4.3% were Grade IIIB. Among the 138 patients, non-union was the most common complication (22.5%), followed by osteomyelitis (18.1%) (Table 2),wound infection (11.6%), ankle stiffness (10.9%), requirement of plastic cover (4.3%), and knee stiffness (4.3%).
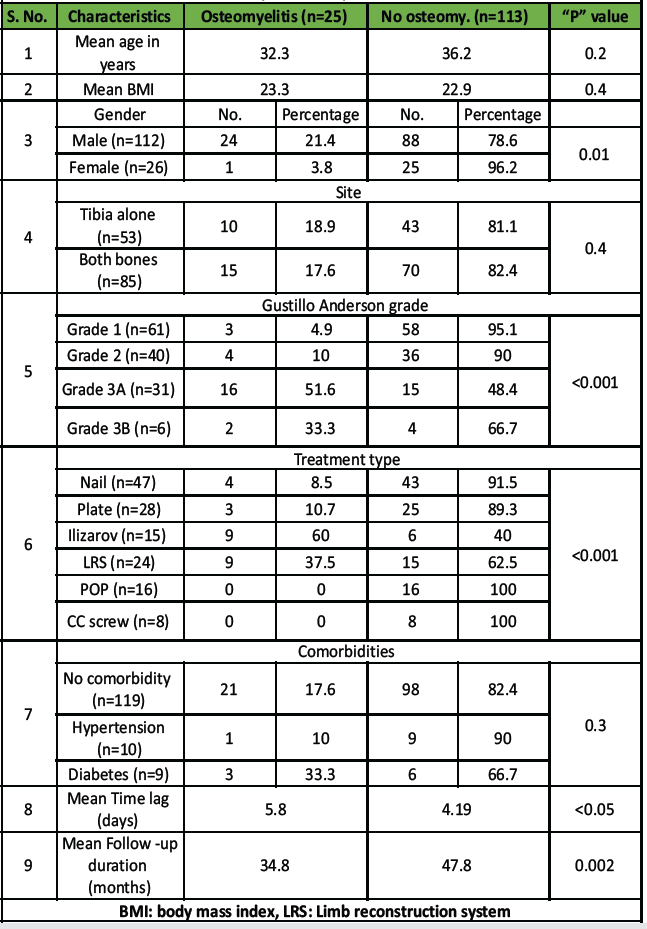 Table 2: Association of osteomyelitis with patient and clinical characteristics
Table 2: Association of osteomyelitis with patient and clinical characteristics
Higher Gustilo-Anderson grades showed a clear trend toward increase complication rates (Graph 1-4).
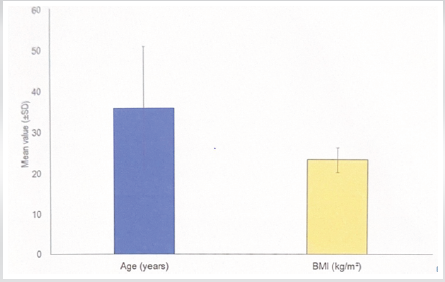 Graph 1: mean age and body mass index of the study population.
Graph 1: mean age and body mass index of the study population.
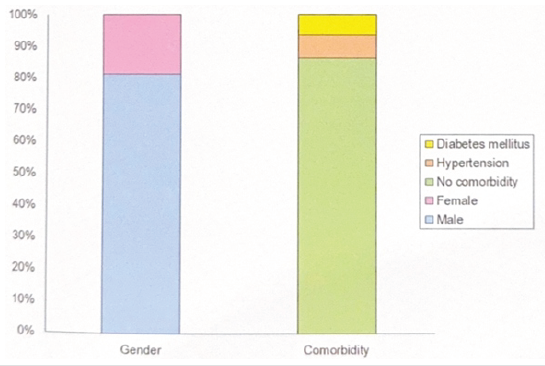 Graph 2: Gender and comorbidity status of study population.
Graph 2: Gender and comorbidity status of study population.
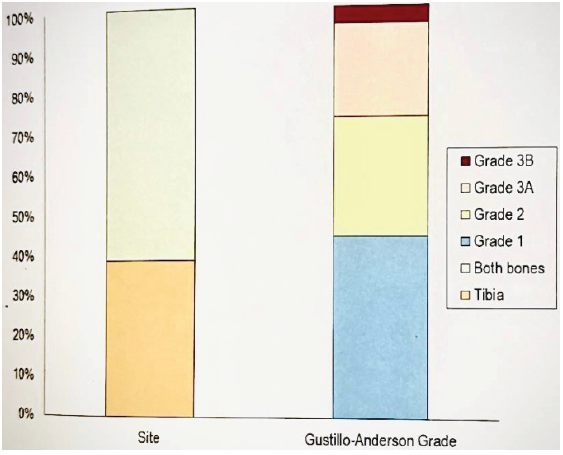 Graph 3: Site and grade of compound fracture.
Graph 3: Site and grade of compound fracture.
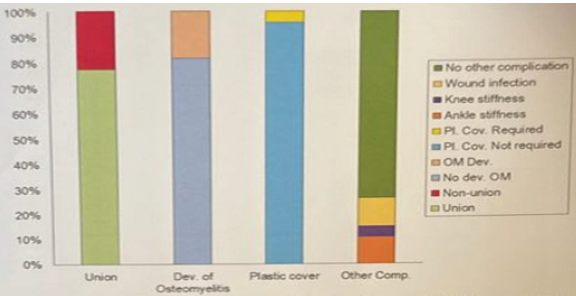 Graph 4: Outcome variables (union, development of osteomyelitis, requirement of plastic cover, and other complications).
Graph 4: Outcome variables (union, development of osteomyelitis, requirement of plastic cover, and other complications).
Out of 138 fractures, 107 (77.5%) achieved union, whereas 31 (22.5%) resulted in non-union. Univariate analysis revealed that the Gustilo-Anderson grade, treatment modality, time lag to treatment, and presence of diabetes mellitus were significantly associated with non-union. The non-union rate increased progressively with higher Gustilo-Anderson Grades – 3.3% in Grade I, 20% in Grade II, 54.8% in Grade IIIA, and 66.7% in Grade IIIB (P < 0.001). The type of treatment also had a significant impact, with nailing showing the lowest non-union rate (8.5%), while Ilizarov (66.7%) and LRS (41.7%) had higher rates (P < 0.001) (Graph 6 ).
 Graph 6: Showing types of treatment.
Graph 6: Showing types of treatment.
The mean time lag was 5.2 days in the non-union group and 4.2 days in the union group (P = 0.02). The presence of diabetes mellitus was also significantly associated with non-union (P = 0.001). On multivariate logistic regression analysis, only the Gustilo-Anderson grade emerged as an independent determinant of non-union with an OR of 5.604 (P = 0.001). Similarly, the same parameter was found to be the only independent determinant for other complications (OR 1.779, P = 0.017). Functional outcomes assessed using the Barthel index, soft-tissue healing time, and duration of hospital stay, demonstrated a significant correlation with the severity of soft-tissue injury. The Barthel index was markedly lower among patients with Grade IIIA and IIIB fractures (mean 80.6–80.8) compared to those with Grade I fractures (90.9, P = 0.00). The mean soft-tissue healing time was 35.0 days in Grade IIIA cases and 15.2 days in Grade I fractures (P = 0.00). Similarly, the mean duration of hospital stay was significantly longer in Grade IIIA patients (20.0 days) compared to Grade I (8.8 days, P = 0.00). These findings indicate that higher Gustilo-Anderson grades are associated with poorer functional outcomes and prolonged recovery (Table 1-4).
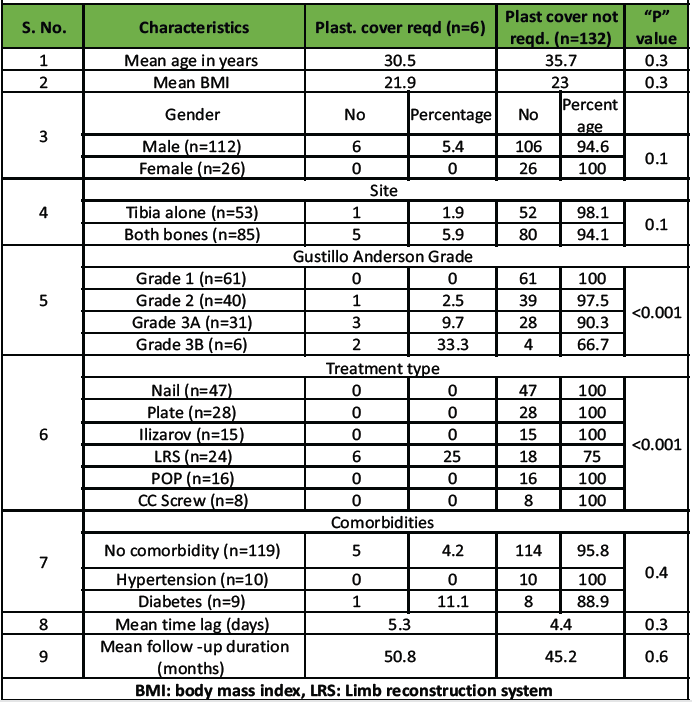 Table 3: Association of plastic cover requirement with patient and clinical characteristics
Table 3: Association of plastic cover requirement with patient and clinical characteristics
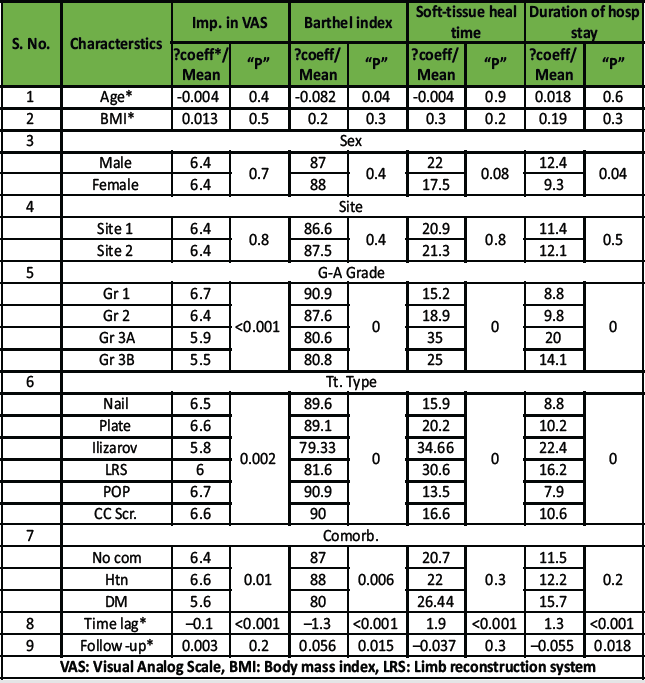 Table 4: Association of parametric outcomes (improvement in VAS, Barthel index, so-fttissue healing time, duration of hospital stay) with patient/clinical characteristics
Table 4: Association of parametric outcomes (improvement in VAS, Barthel index, so-fttissue healing time, duration of hospital stay) with patient/clinical characteristics
The data were analyzed using appropriate statistical methods, with a P < 0.05 considered statistically significant. Descriptive statistics were used to summarize baseline characteristics, and Chi-square/Fisher’s exact tests were applied for categorical variables, while the Independent Sample t-test was used for continuous variables such as age and time lag. Multivariate logistic regression analysis was performed to identify independent predictors of major outcomes. In summary, the overall non-union rate was 22.5%, with a strong association with higher Gustilo-Anderson grades. The Gustilo-Anderson grade was found to be the only independent determinant of both non-union and other complications. In addition, longer time lag, use of external fixation (Ilizarov/LRS), and presence of diabetes were significant predictors of non-union on univariate analysis. Functional outcomes, including the Barthel index, soft-tissue healing, and hospital stay, were significantly poorer in patients with higher-grade open fractures (Table 5).
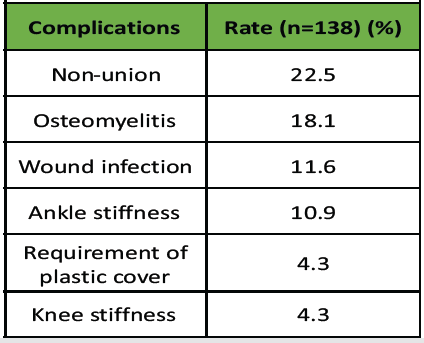 Table 5: Complication and outcome rates
Table 5: Complication and outcome rates
The present study highlights that the severity of the initial soft-tissue injury, as defined by the Gustilo-Anderson classification, is the most powerful determinant of complications and outcomes in open tibial diaphyseal fractures. The rates of non-union (22.5%) and osteomyelitis (18.1%) increased proportionally with the Gustilo grade, emphasizing the prognostic importance of soft-tissue damage. A time lag <4.2 days between injury and definitive treatment was found to be significantly associated with non-union, underscoring the importance of early surgical intervention. Among treatment modalities, IMN demonstrated the highest union rates and lowest infection rates, validating it as the preferred method for lower-grade open fractures (Grades I-II). In contrast, high-grade fractures (Grades IIIA-IIIB) continue to present formidable challenges due to soft-tissue compromise, contamination, and bone loss. For these injuries, a staged approach combining prompt debridement, temporary stabilization, and early soft-tissue coverage remains essential. Overall, this study reinforces that timely and meticulous debridement, appropriate fixation strategy selection, and meticulous soft-tissue management are crucial to improving union rates and minimizing infection.
Early and aggressive surgical management is key to achieving optimal outcomes in open tibial diaphyseal fractures.
- Prioritize early debridement and stable fixation – preferably within 4 days of injury
- IMN should be favored in lower-grade fractures (Gustilo I-II) for its superior union and lower infection rates
- High-grade fractures (Gustilo IIIA/IIIB) require a multidisciplinary, staged approach involving early plastic coverage and vigilant infection control.
By minimizing treatment delays and optimizing fixation selection, surgeons can significantly reduce non-union and osteomyelitis rates, improving both functional recovery and long-term outcomes.
References
- 1. Li J, Zhang K, He X, Wang Q, Lu Y, Feng Q, et al. Relationship between time to surgical debridement and the incidence of infection in patients with open tibial fractures. Orthop Surg 2020;12:524-32. [Google Scholar] [PubMed]
- 2. Singh P, Singh SK, Gill SP. Management of compound fractures of tibia by limb reconstruction system (LRS). J Bone Joint Dis 2020;35:29-34. [Google Scholar] [PubMed]
- 3. Tian R, Zheng F, Zhao W, Zhang Y, Yuan J, Zhang B, et al. Prevalence and influencing factors of nonunion in patients with tibial fracture: Systematic review and meta-analysis. J Orthop Surg Res 2020;15:377. [Google Scholar] [PubMed]
- 4. Ukai T, Hamahashi K, Uchiyama Y, Kobayashi Y, Watanabe M. Retrospective analysis of risk factors for deep infection in lower limb Gustilo-Anderson type III fractures. J Orthop Traumatol 2020;21:10. [Google Scholar] [PubMed]
- 5. Debnath R, Basak S, Sahu , Sahu PK, Sarkar A, Majhi P. lizarov technique for the management of open fractures of the tibia: A study of effectiveness. J Clin Diagn Res 2020;14:RC01-4. [Google Scholar] [PubMed]
- 6. Kapila A, Singh D, Sharma VK , Singh S. Usefulness of LRS for the treatment of open fractures of long bones of the lower limb with substantial bone loss. Int J Orthop Sci 2018;4:651-5. [Google Scholar] [PubMed]
- 7. Mahajan NP, Mangukiya HJ. Extended use of limb reconstruction system in management of compound tibia diaphyseal fracture as primary and definitive tool. Int J Orthop Sci 2017;3:1157-64. [Google Scholar] [PubMed]
- 8. Vasanad N, Anchan VK, Kumar BN, Singh T, Kulkarni V. minimally invasive plate osteosynthesis for concurrent distal tibia and fibula fractures. J Clin Diagn Res 2016;10:RC01-5. [Google Scholar] [PubMed]
- 9. Singla M, Bhaskar AR, Gupta A,Agrawal A , outcome of open femoral shaft fractures: A retrospective analysis of 55 patients. Int J Orthop Sci 2016;2:89-93. [Google Scholar] [PubMed]
- 10. Lack WD, Karunakar MA, Angerame MR, Seymour RB, Sims S, Bosse MJ, et al. Type III open tibia fractures: Immediate antibiotic prophylaxis minimizes infection J Orthop Trauma 2015;29:1-7. [Google Scholar] [PubMed]









