Septic arthritis of the wrist is a rare but limb-threatening condition that may present with subtle clinical and laboratory findings, leading to delayed diagnosis and rapid joint destruction. In neglected or advanced cases, a staged surgical strategy combining aggressive debridement, targeted antibiotic therapy, and definitive arthrodesis can achieve effective infection control and satisfactory functional outcomes.
Dr. Oruç Keleş, Department of Orthopaedics and Traumatology, Erzincan Binali Yildirim University, Erzincan, Turkey. E-mail: keles.oruc@gmail.com
Introduction: Septic arthritis of the wrist is an uncommon condition, representing only a small fraction of all septic arthritis cases.
Case Report: This report details the clinical course of a 63-year-old female patient who developed septic arthritis and subsequent osteomyelitis of the wrist following a traumatic laceration. Despite multiple courses of antibiotics and a delayed diagnosis, the patient ultimately required a two-stage surgical approach, including debridement, placement of an antibiotic spacer, and definitive arthrodesis with autologous bone grafting. Microbiological analysis revealed Staphylococcus aureus as the causative organism. The case highlights the diagnostic challenges associated with wrist septic arthritis due to its rarity and non-specific presentation, which can lead to delayed treatment and severe joint destruction.
Conclusion: Prompt recognition, thorough diagnostic workup, including synovial fluid analysis and culture, and early surgical intervention are crucial for optimal outcomes. The report underscores the importance of considering septic arthritis in the differential diagnosis of wrist pain and swelling to prevent irreversible complications.
Keywords: Wrist, septic, arthritis, Staphylococcus.
Septic arthritis of the wrist is a rare clinical condition, accounting for approximately 3% of all cases of septic arthritis [1]. Due to its potential to cause rapid and irreversible joint destruction, it is considered an orthopedic emergency. The differential diagnosis includes gout, osteoarthritis, crystal-induced arthropathies, and cellulitis [2]. Because it is an uncommon presentation and inflammatory markers and radiographic findings do not always correlate with the severity of infection, establishing the diagnosis can be challenging [3]. Septic arthritis of small joints is more likely to be overlooked than that of large joints, as it is less frequently considered in the initial differential diagnosis [4].
A 63-year-old female patient sustained a laceration to her right wrist after being struck by a propeller approximately 3 years before presentation. The wound was sutured at an outside center, and antibiotic therapy was initiated. After approximately 1 month of follow-up, the patient developed redness, swelling, pain, tenderness, and restricted range of motion in the wrist. She was subsequently followed at several different centers for nearly 6 months with antibiotic therapy. At the end of this period, she was informed that the osseous structure of the wrist was severely compromised and that extensive osteomyelitis had developed, for which surgical treatment was recommended. The patient later presented to our clinic with persistent wrist pain and limitation of motion. Her medical history was notable for hypertension, coronary artery disease, and an anxiety disorder. There was no history of rheumatologic disease. She denied smoking and alcohol use, and no significant family history was reported.
Physical examination and imaging
On inspection, marked swelling and erythema were observed in the right wrist compared with the contralateral side. Palpation revealed significant pain and tenderness over the wrist joint. Distal neurovascular and motor examinations were unremarkable. Range of motion assessment demonstrated limitation of wrist extension to 15° and flexion to 45°. Plain radiographs revealed joint subluxation, severe degeneration of the carpal bones consistent with osteomyelitis, narrowing of the radiocarpal and radioulnar joint spaces, and diffuse arthritic changes. According to the Eaton Littler Classification system, our patient’s wrist joint degeneration was grade 4 [5]. The patient was evaluated postoperatively at 15, 30, 45, and 60 days. At each follow-up visit, progressive improvement in pain and tenderness was noted, and pain on weight bearing had completely resolved.
Laboratory findings
At the patient’s initial presentation to the outside center, laboratory investigations demonstrated a C-reactive protein (CRP) level of 66.9 mg/L and an erythrocyte sedimentation rate (ESR) of 46 mm/h. During subsequent follow-up, CRP increased to 111 mg/L and ESR to 59 mm/h. At the time of admission to our clinic, laboratory values showed a CRP level of 11.7 mg/L, procalcitonin <0.12 ng/mL, and an ESR of 21 mm/h. Intraoperative culture specimens obtained at our institution yielded growth of Staphylococcus aureus. Following definitive treatment and follow-up, laboratory parameters normalized, with CRP of 3.9 mg/L, procalcitonin of 0.12 ng/mL, and ESR of 14 mm/h.
Surgical technique
A two-stage surgical approach was employed for wrist arthrodesis. In the first stage, a volar (Henry) approach was used to excise all necrotic bone and soft tissue affected by osteomyelitis, and tissue samples were obtained for culture (Figure 1).
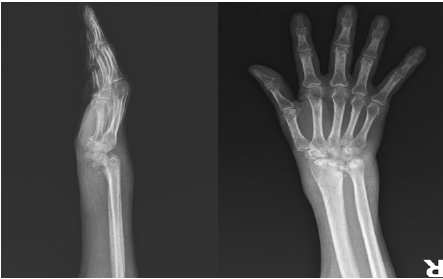
Figure 1: Pre-operative wrist joint degeneration.
An external fixator was applied to achieve wrist distraction, and an antibiotic-impregnated spacer was prepared and placed within the joint (Figure 2).
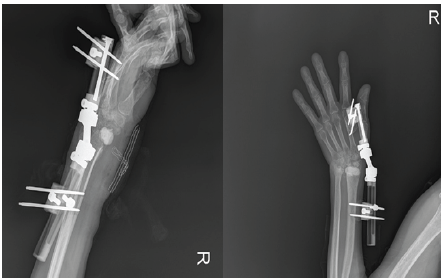
Figure 2: The first stage of the two-stage surgical approach involved placement of an antibiotic-impregnated spacer and a monolateral external fixator.
Postoperatively, antibiotic therapy was administered according to culture results in consultation with the infectious diseases department. After approximately a 3-month interval, definitive arthrodesis was performed (Figure 3).
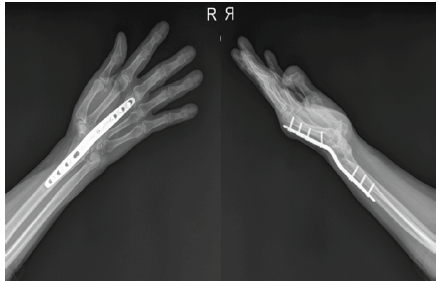
Figure 3: The second stage of the two-stage surgery consisted of wrist arthrodesis using plate-and-screw fixation.
Through a dorsal incision between the third and fourth extensor compartments, the spacer was removed, and an autologous bone graft harvested from the iliac crest was placed. Stable fixation was achieved using an arthrodesis plate in an appropriate functional position.
Septic arthritis of the wrist is an uncommon condition and may be easily overlooked due to its rarity and non-specific presentation. In many cases, inflammatory or degenerative joint disorders are initially considered, leading to delayed diagnosis and treatment. The diagnosis of wrist septic arthritis relies primarily on synovial fluid analysis. Therefore, joint aspiration should be attempted in all patients with suspected wrist joint infection. Given the similar underlying pathophysiological mechanisms, synovial fluid cell counts comparable to those observed in large joint septic arthritis are expected in wrist joint aspirates [6]. Positive Gram-staining and culture findings not only confirm the diagnosis but also guide antibiotic therapy. Although various microorganisms may be responsible for wrist joint infections, S. aureus is the most commonly isolated pathogen. However, in up to 40% of cases, no causative organism can be identified [7]. Treatment typically consists of 1–2 weeks of intravenous antibiotics followed by an additional 2–4 weeks of oral therapy. When managed promptly with appropriate surgical debridement and concomitant antibiotic treatment, outcomes are generally favorable. Rashkoff et al. reported superior clinical outcomes in patients who underwent arthrotomy within 10 h of diagnosis in their series of 29 patients [8-10].
Septic arthritis is a well-recognized orthopedic emergency, particularly in large joints, and plays a crucial role in the differential diagnosis due to its potentially devastating consequences. However, in smaller joints such as the wrist, it is less frequently considered and therefore more likely to be missed. Without early recognition and timely intervention, irreversible joint destruction is inevitable. Regardless of joint size, septic arthritis should always be included in the differential diagnosis when compatible symptoms are present and should be promptly ruled out.
Septic arthritis should always be considered in patients presenting with wrist pain and swelling, even in the absence of striking laboratory or radiographic findings, as delayed diagnosis can result in rapid joint destruction and osteomyelitis. In advanced or delayed cases, a staged surgical approach with aggressive debridement, appropriate antibiotic therapy, and definitive arthrodesis can provide effective infection control and satisfactory functional outcomes.
References
- 1. Kawamura K, Yajima H, Omokawa S, Maegawa N, Shimizu T, Nakanishi Y, et al. Septic arthritis of the wrist caused by Mycobacterium intracellulare: A case report. Case Reports Plast Surg Hand Surg 2016;3:79-82. [Google Scholar] [PubMed]
- 2. Momodu II, Savaliya V. Septic arthritis. İn: StatPearls. Treasure Island, FL: Statpearls; 2025. [Google Scholar] [PubMed]
- 3. Mathews CJ, Weston VC, Jones A, Field M, Coakley G. Bacterial septic arthritis in adults. Lancet 2010;375:846-55. [Google Scholar] [PubMed]
- 4. Adeboye T, Giwa L, Jemec B. Managing small joint septic arthritis of the hand. J Hand Surg Asian Pac Vol 2023;28:530-8. [Google Scholar] [PubMed]
- 5. Kennedy CD, Manske MC, Huang JI. Classifications in brief: The eaton-littler classification of thumb carpometacarpal joint arthrosis. Clin Orthop Relat Res 2016;474:2729-33. [Google Scholar] [PubMed]
- 6. Skeete K, Hess EP, Clark T, Moran S, Kakar S, Rizzo M. Epidemiology of suspected wrist joint infection versus inflammation. J Hand Surg Am 2011;36:469-74. [Google Scholar] [PubMed]
- 7. Jennings JD, Ilyas AM. Septic arthritis of the wrist. J Am Acad Orthop Surg 2018;26:109-15. [Google Scholar] [PubMed]
- 8. Rashkoff ES, Burkhalter WE, Mann RJ. Septic arthritis of the wrist. J Bone Joint Surg Am 1983;65:824-8. [Google Scholar] [PubMed]
- 9. Estipona B, Collins GL, Sivapalan S, Montgomery S, Riaz T. Native joint septic arthritis. Infect Dis Clin North Am 2025;39:449-63. [Google Scholar] [PubMed]
- 10. Benito N, Martínez-Pastor JC, Lora-Tamayo J, Ariza J, Baeza J, Belzunegui-Otano J, et al. Executive summary: Guidelines for the diagnosis and treatment of septic arthritis in adults and children, developed by the GEIO (SEIMC), SEIP and SECOT. Enferm Infecc Microbiol Clin (Engl Ed) 2024;42:208-14. [Google Scholar] [PubMed]