[box type=”bio”] What to Learn from this Article?[/box]
In the differential diagnosis of radicular pain, possibility of schwannoma of peripheral nerve should be kept in mind.
Case Report |Volume 5 | Issue 2 | JOCR April-June 2015 | Page 35-37 | Santosh Banshelkikar, Pruthviraj Nistane. DOI: 10.13107/jocr.2250-0685.268
Authors: Santosh Banshelkikar[1], Pruthviraj Nistane[1]
[1] Department of Orthopaedics, LTM Medical College And Hospital, Sion, Mumbai – 400022. India.
Address of Correspondence:
Dr Santosh N Banshelkikar
Flat 101, Building 40/1 Siddhivinayak Co-op, Housing Society, near Municipal School, Tilaknagar West, Mumbai 400089. India. Email : drsantoshnb@gmail.com
Abstract
Introduction: Peripheral nerve tumours are rarely acknowledged as a cause of radiating pain in lower limbs and suspicion is almost always pointed towards lumbo-sacral causes. Schwannomas are tumours of peripheral nerve sheaths occurring anywhere along the peripheral nervous system. Often it can produce symptoms, which can be misleading in cases where obvious swelling is not present. The diagnosis may therefore be delayed by several years of emergence of symptoms. Very few such cases have been reported previously and none of them had an intrasubstance location of the tumour as in our case.
Case Report: We present a case of a middle aged female patient presenting with radiating pain in left lower limb, which was diagnosed and treated as lumbo-sacral radiculopathy for five years before an obvious swelling appeared, which on further investigations led to diagnosis of schwannoma of tibial nerve. Intraoperatively, the schwannoma was found to be intrasubstance in location which has never been reported in the past literatures making its excision, without damaging the conducting elements, a challenge.
Conclusion: The possibility of peripheral nerve tumour should always be kept in mind while dealing with long standing cases diagnosed as radiculopathy and which do not get better with treatment on similar lines. A thorough clinical examination of the entire limb including Tinel’s sign can clinch the diagnosis earlier in cases where obvious swelling is not present. Even unusual presentations, as in our case, can be dealt surgically with good results.
Keywords: schwannoma; intrasubstance location; radiculopathy.
Introduction
Schwannoma also known as neurilemmoma, neurinoma or Schwann cell tumour is a benign, well-defined and usually solitary nerve sheath tumour accounting for 5% of all soft tissue tumours [1]. Schwannomas are the most common tumours of the sheath of peripheral nerves. It arises from the Schwann cells and generally located at the periphery of nerve. Malignant transformation is rarely seen [2]. It can occur anywhere along the peripheral nervous system but its occurrence in lower limb is rare. It is a slowly growing tumour and may present as a painless, discrete and firm swelling, unless it grows in a confined place in which case neurological deficit may occur. The clinical diagnosis may be delayed for many years in a schwannoma of the tibial nerve because rarity of its occurrence in this region and the fact that it is often misdiagnosed as entrapment neuropathy or lumbosacral radiculopathy etc. In such cases the diagnosis may be delayed for as long as many years [3]. Ghaly described a patient suffering with pain in the foot for ten years before diagnosis of a schwannoma of the tibial nerve in the calf was made [4].Smith and Amis described a patient who presented with pain in the foot for eight years before recognition of a schwannoma of the tibial nerve [5].
Preoperative diagnosis of schwannoma of tibial nerve is often difficult unless the surgeon is specifically looking for it because the swelling may not be evident in initial stages and symptoms may be non-specific. Computed tomography, magnetic resonance imaging, and sonography are useful imaging modalities in the diagnosis of these nerve sheath tumours. Treatment is conservative unless it is causing significant symptoms or neurological deficit in which case surgical excision of the tumour is often required. Excision is generally harmless due to peripheral location of the tumour in the nerve, as compared to neurofibroma. We report a case of schwannoma with unusual presentations which was located in tibial nerve and it was intrasubstance in location in the nerve, making the surgical excision a challenge.
Case report
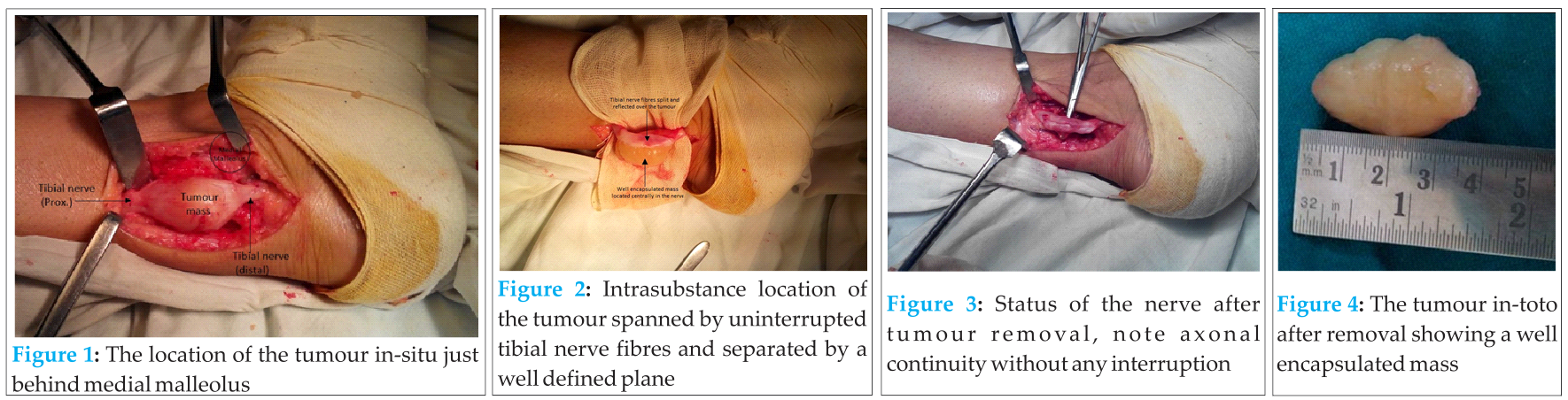
A middle aged female patient presented to our hospital with complains of radiating pain in left lower leg, ankle and sole of foot for past five years and for the past six months, a painful focal swelling was noted on inner aspect of ankle. Various diagnoses including lumbosacral radiculopathy, tarsal tunnel syndrome, complex regional pain syndrome (CRPS) etc. were made previously. She was on treatment in lines of radiculopathy, previously, without much benefit. There was no neurological deficit. No relevant medical/family history was noted. On local examination there was a swelling approximately of size 6*4*4 cm at left ankle just behind the medial malleolus (figure 1). It was exquisitely tender on palpation. Local temperature was normal. Swelling was firm in consistency. It was non fluctuant, non compressible, non reducible and non pulsatile. It was not fixed to underlying bone or overlying skin. It was freely mobile side to side but not longitudinally. Movements of the ankle were normal and there was no distal neuro-vascular deficit. Tinel’s sign was positive. Examination of rest of the extremity and lower back was inconclusive. Blood work up and x-rays were normal. MRI of the lumbo-sacral spine was done previously which was normal. Neurophysiological studies were performed which showed normal nerve conduction without an axonopathy. MRI of the left ankle was done which showed a well circumscribed mass of size 5*4.5*2 cm just adjacent to medial malleolus arising from the tibial nerve.
Based on the symptoms and investigations, a diagnosis of schwannoma of the tibial nerve was made and surgical resection was planned. In regional anaesthesia and the patient in supine position, the limb was kept in figure of four position. Direct incision was given over the swelling and a well defined mass was isolated which was arising from the tibial nerve forming a fusiform swelling. Adequate exposure of the nerve proximally and distally to the tumour was done. Contrary to usual eccentric location, the tumour was present centrally in the nerve with nerve fibres spanning it from all the sides. The swelling was opened by a longitudinal incision and a plane was developed between the nerve bundles and the well defined capsule of the tumour (figure 2) which was then removed as a whole. Small fascicles entering the tumour also required removal. The continuity of the nerve fibres of the main trunk was ensured (figure 3). The mass was dissected and resected without any damage to the nerve. Intra-operative opinion of plastic surgeon regarding status of the nerve, post tumour removal, was taken and it was relocated in the nerve bed as such and the wound closed in layers over a suction drain. The mass was well circumscribed, encapsulated, firm and gray in colour with areas of cystic change. It was 4*3.5*2 cm in size (figure 4). 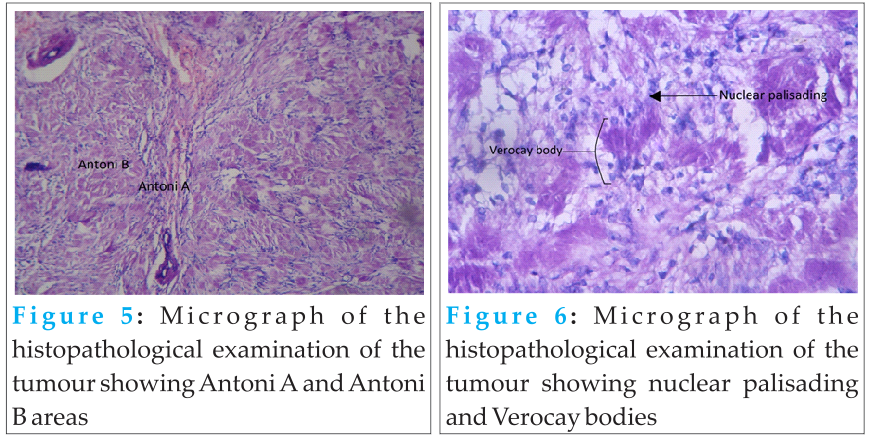
Discussion
Benign peripheral nerve sheath tumours can be classified into schwannomas and neurofibromas. As in our patient, schwannomas are usually solitary and well capsulated. Schwannoma has been reported to be eccentrically located and does not involve the main nerve [6]. Schwannoma tends to displace the nerve fibres peripherally in contrast to neurofibromas, which grow within the nerves and penetrates them, potentially necessitating partial or complete removal of the nerve producing deficit. Schwannoma is a very slow-growing mass and often is asymptomatic. However, symptoms may occur as a result of nerve compression or in some cases due to entrapment of the fascicles in the tumour. It has been reported that schwannoma presents as a palpable mass with local pain and paraesthesia, which is exacerbated by direct percussion of the mass [7]. Schwannomas most commonly occur in the head and neck involving the brachial plexus and spinal nerves. The upper and lower limbs are affected less often as contrast to what was seen in our case [8]. However if at all it occurs in the lower limb, tibial nerve at the tarsal sinus is the most frequently involved site [9]. The diagnosis of schwannoma in this case was difficult and delayed due to its unusual presentation in the lower limb which is not a common site for schwannomas and late appearance of the focal swelling of this slow growing tumour. There was radiating pain and distribution of the symptoms not localised to the pathological site for prolonged duration contributing to misdiagnosis as radiculopathy. Also schwannomas can present with no symptoms or mild symptoms. Most lesions present as a slowly growing painless soft-tissue mass. Symptoms are unusual, unless the mass has become large enough to compress the adjacent nerve. These factors may lead to dilemma in diagnosis and attribution of the symptoms to some other cause [10]. So schwannomas should always be considered as a differential diagnosis when tarsal tunnel syndrome, neuroma, nerve entrapment or radiculopathy is suspected.
Although schwannoma may occur at any age, it is commonly seen between the ages of 20 and 50 years, with equal male and female predisposition. In addition, it has been reported that schwannoma is often contiguous with the nerve and located eccentrically. Even though schwannoma tends to be benign, the treatment of choice is typically total resection of the tumor in symptomatic cases. Diagnosis can be confirmed on histopathology (H & E) but in certain cases, immunohistochemical markers like S100 protein (most important), CD34, Factor XIIIa, CD56, Ki67, neurofilament protein, calretinin etc can be used to distinguish it from neurofibroma [11]. The prognosis of schwannoma is very favourable. Severe nerve damage or neurological deficits are uncommon because of the perineurium and the eccentric location of the tumor with respect to the involved nerve. Postsurgical functional or sensational impairment may occur, but it typically resolves shortly after [12]. But in our case surgical resection was challenging because of the intrasubstance location the tumour which is highly uncommon and not reported so far in literature. Although post surgery there was no added neurological deficit noted.
Conclusion
Peripheral nerve tumours are rarely acknowledged clinical entities. A benign tumour of the sheath of a peripheral nerve can be one explanation for longstanding neuropathic pain in the foot, ankle and leg where all other possibilities are ruled out. Chronic unexplained foot, calf pain and a positive Tinel’s sign should raise suspicion of tibial nerve neurilemoma. A lump may not be palpable in the early stages and we therefore recommend to always keeping this possibility in mind while dealing with such cases. An examination of the entire length of the tibial nerve including sciatic nerve by palpation and percussion and looking for the Tinel’s sign is helpful in diagnosis which should be confimed by MRI or ultrasound examination. Even in patients who have had such tumors for years, surgical resection remains the treatment of choice. The surgical outcome is good and relieves the patient of the long standing symptoms. Results are encouraging even in unusual presentations like tumours with intrasubstance location.
Clinical
Peripheral nerve sheath tumours can present with radicular symptoms and this should always be included in the differential diagnosis of radiculopathy syndromes to facilitate early diagnosis and effective management.
References
1. Kransdorf M. Benign soft-tissue tumors in a large referral population: distribution of specific diagnosis by age, sex and location. AJR Am J Roentgenol. 1995;164:395–402.
2. Enzinger F, Weiss S. Malignant tumours of peripheral nerves. In: Soft tissue tumours. 2nd ed. Philadelphia: Mosby;1988:781-2.
3. Nawabi D, Sinisi M. Schwannoma of the posterior tibial nerve: the problem of delay in diagnosis. J Bone Joint Surg Br. 2007 Jun;89(6):814-6.
4. Ghaly R. A posterior tibial nerve neurilemmoma unrecognized for 10 years: case report. Neurosurgery. 2001;48:668-72.
5. Smith W, Amis J. Neurilemmona of the tibial nerve: a case report. J Bone Joint Surg [Am]. 1992;74-A:443-4.
6. Jenkins S: Solitary tumours of peripheral nerve trunks. J Bone Joint Surg. 1952;34B:401–411.
7. Maleux G, Byrs P, Samson I, Sciot R, Baert A. Giant schwannoma of the lower leg. EurRadiol. 1997;7:1031–4.
8. Birch R, Bonney G, Wynn Parry C. The peripheral nervous system and neoplastic disease. In: Surgical disorders of peripheral nerves. Edinburgh: Churchill Livingstone;1998:335-52
9. Eroglu U, Bozkurt M, Ozates O, Akturk S, Tuna H Sciatic nerve schwannoma: case report. Turk Neurosurg. 2014;24(1):120-2.
10 White NB: Neurilemomas of the extremities J Bone Joint Surg. 1967;49A:1605-1610.
11 Fine SW, McClain SA, Li M: Immunohistochemistry staining for calretinin is useful for differentiating schwannomas from neurofibromas. Am J Clin Pathol 122: 552-559, Oct 2004.
12. Sang-Min Kim, Sung-WookSeo, Jun-Young Lee, Ki-Sun Sung. Surgical outcome of Schwannomas arising from major peripheral nerves in the lower limb. International Orthopaedics. 2012 May;36(8):1721-5.
| How to Cite This Article: Banshelkikar S, Nistane P. Intrasubstance Schwannoma Of Posterior Tibial Nerve Presenting As Lumbo-sacral Radiculopathy. Journal of Orthopaedic Case Reports 2015 April-June;5(2):35-37. Available from: https://www.jocr.co.in/wp/2015/04/20/2250-0685-268-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com