[box type=”bio”] What to Learn from this Article?[/box]
Paediatric Hip dislocations still have good prognosis, if treated at right time.
Case Report | Volume 5 | Issue 2 | JOCR April-June 2015 | Page 69-71| Navin Balasubramanian, N Ganesh Babu, Sindhuja P. DOI: 10.13107/jocr.2250-0685.279
Authors: Navin Balasubramanian[1], N Ganesh Babu[2], Sindhuja P[3]
[1] Department of Orthopaedics, Saveetha Medical College, Thandalam, Chennai. India. [2] Department of Orthopaedics, Sri Ramachandra Medical College, Porur,Chennai. India. [3] Department of Orthopaedics, Govt. Peripheral Hospital , Anna Nagar, Chennai. India
Address of Correspondence Dr Navin Balasubramanian, No.19, 21st Main Road, Anna Nagar. Chennai-600040. Tamil Nadu. India. Email:- drnavin_ortho@yahoo.co.in
Abstract
Introduction: Hip dislocation in a child less than 3 years is a very rare event. Only a few case reports have been documented in Western literature. It is rarely reported from Indian population. Hip dislocations are mostly due to low velocity injury in children younger than 3 years. We report such a case of hip dislocation in a 2 year old child.
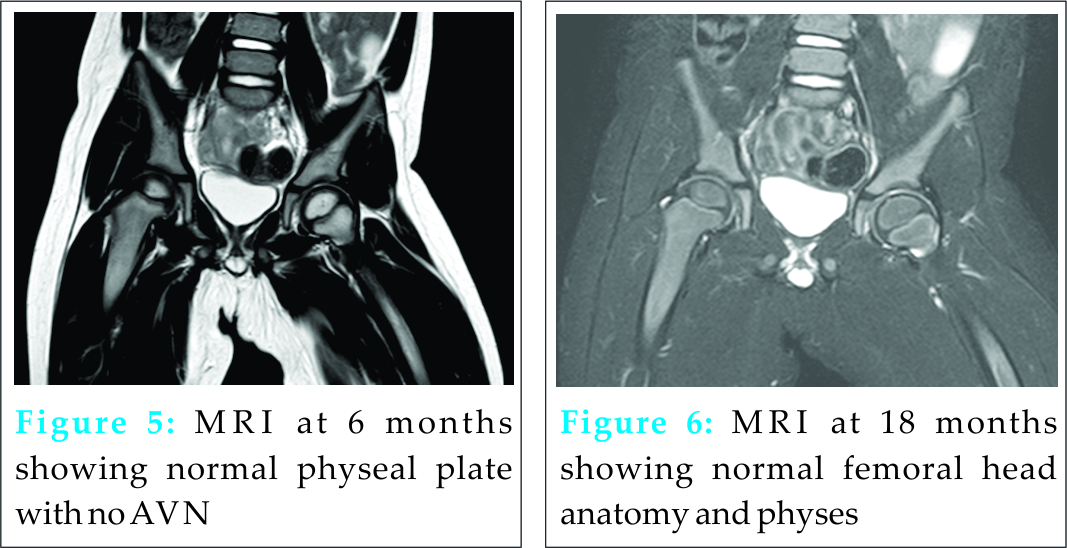
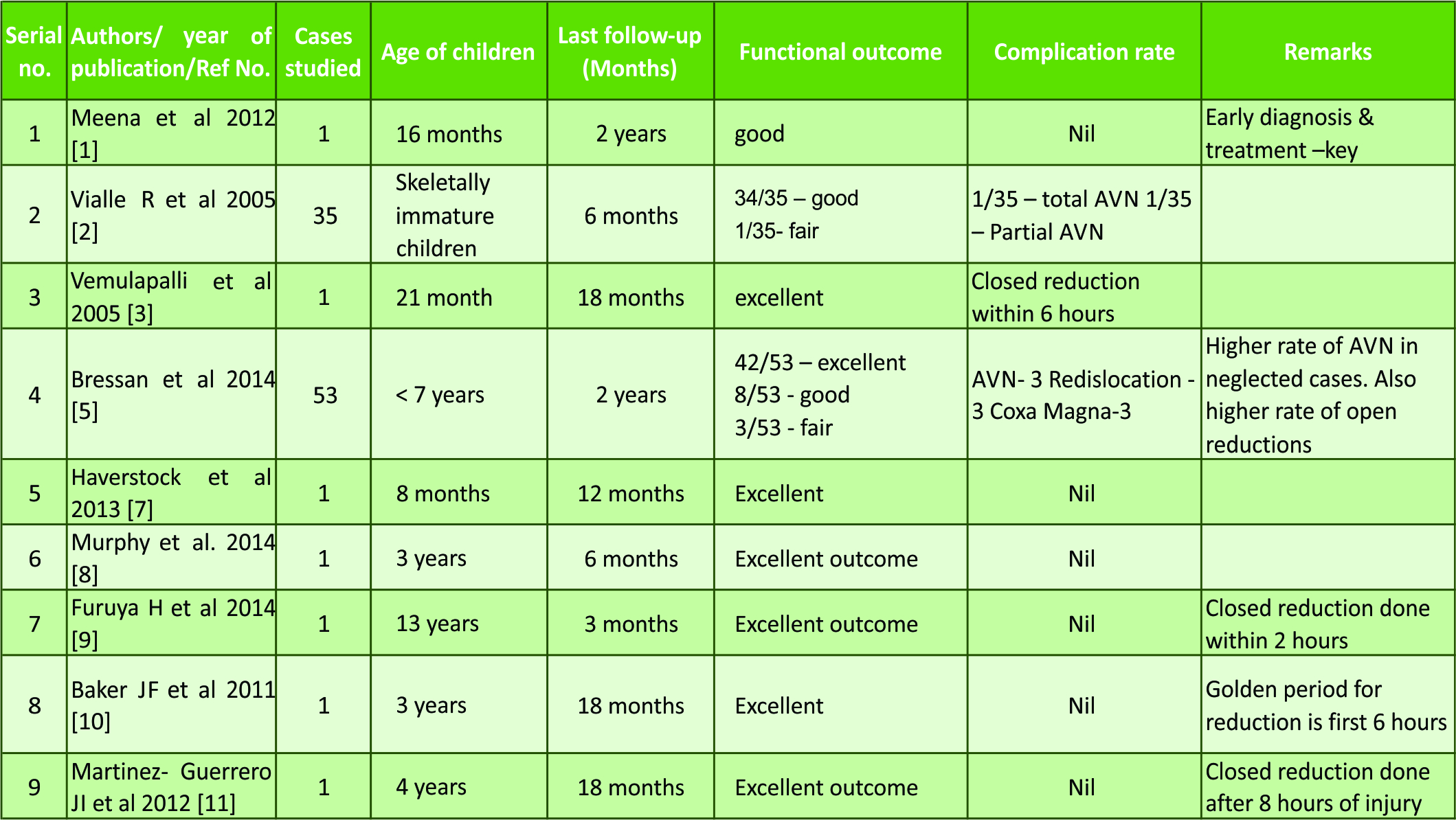
Case Report: A 25 month old child presented to our casualty following a fall from a slide 3 hours prior to presentation. His right lower limb was adducted and internally rotated. There was severe pain on attempting movements. An X-ray of the pelvis was taken which showed a posterior hip dislocation on the right side.The child had an emergency closed reduction under general anaesthesia followed by a broom stick plaster cast with hips in 30º abduction. Congruency of reduction was checked with image intensifier before plaster application. The plaster was removed at 6 weeks and gradual weight bearing started. The child was reviewed at 6 and 18 months with MRI scans at 6 and 18 months. There were no signs of avascular necrosis or chondrolysis.
Conclusion: Paediatric hip dislocation (less than 3 years of age) is a very rare entity whose incidence is on the rise due to the increase in road traffic accidents. The key stone in proper management is clinical suspicion, early recognition and promptreduction (within 6 hours) .Also gentle manipulation during reduction has a definite role in preventing iatrogenic chondrolysis and osteonecrosis of femoral head.
Keywords: Paediatric hip dislocation, broom stick plaster.
Introduction The musculoskeletal anatomy of children varies remarkably from that of the adult population. The periosteum is thick in children, the bones are soft and elastic and can absorb quite some force because of the soft spongy nature. Hence dislocations are rare in paediatric age group. However with the increasing number of motor vehicles plying on our roads and the ever present risk of road traffic accidents, there is a recent change in the above trend. Most of the paediatric injuries are the result of low velocity accidents. In case of high velocity injuries there is almost always the possibility of associated injuries and multi-system involvement. There has been case reports of traumatic hip dislocations in childhood mostly in the western world [3,8,9,10,11]. Most of the published articles in literature include the adolescent population (12-17 years). There are very few case reports of such dislocations in children < 3 years. Here we present a case report of a child (age 25 months) with traumatic posterior dislocation of the hip following low velocity injury.
Case report A 25 month old male child presented to our casualty following a slip and fall from a slide while playing in a park. He presented 3 hours following fall. He had severe pain in the right hip and limb was adducted and internally rotated. An emergency radiograph of the pelvis taken in emergency showed a posterior dislocation of his right hip[Fig.1]. Emergency closed reduction under general anaesthesia was performed. Gentle traction with minimal rotation was sufficient to achieve reduction, the congruency of which was checked under image intensifier. Once congruency was confirmed, an above knee broom stick plaster was applied to both lower limbs with hips in 30º abduction. Check radiographs[Fig.2] was taken along with a MRI[Fig.3] of the hip to check if there was any traumatic injury to the physes. 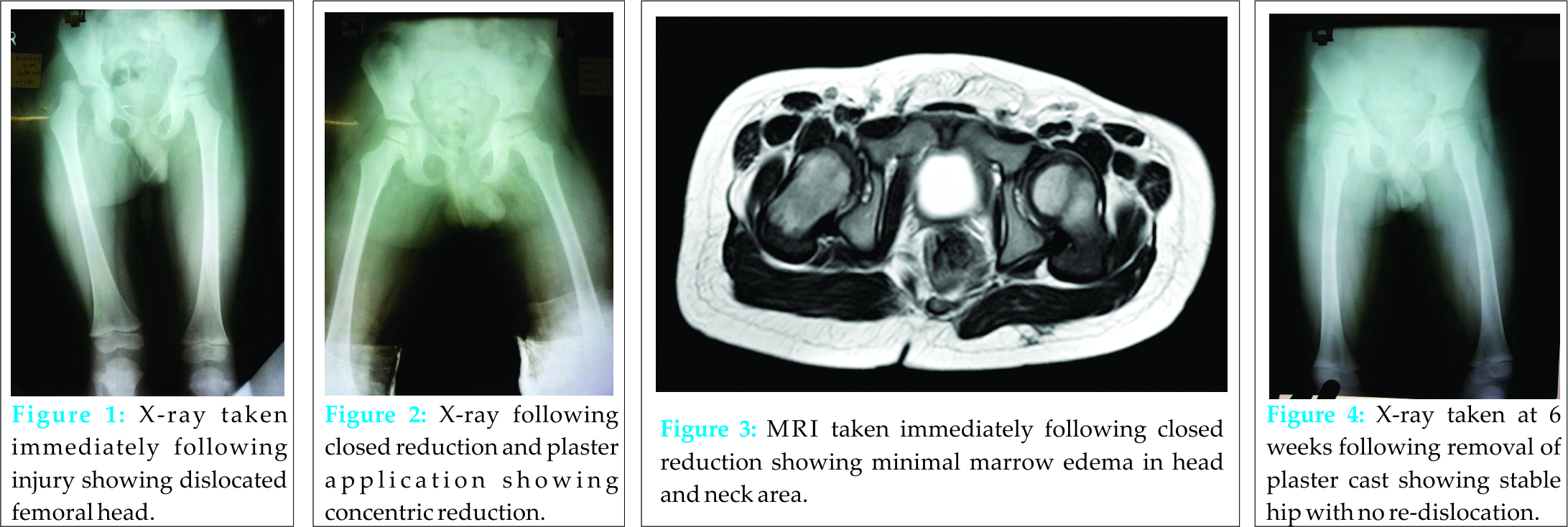
Discussion Paediatric hip dislocation in children less than 3 years is still a rare entity. However with the everpresent danger of motor vehicle accidents in our crowded and chaotic roads, this rarity may become more common. In most children however , hip dislocations are mostly due to low velocity accidents which occur during playing. There are a few reports in Western literature of hip dislocation in peadiatric population, most of them are case reports[3,8,9,10,11]. They mostly report children >3 year old with hip dislocation. There has been only two case reports of children less than 3 years with hip dislocation[1,3]. Also most of the reports emphasizes the need to do urgent reduction within the golden period (i.e 6 hours) [1,4,5,10,11]. The risk of osteonecrosis in one study was 5.7% in acute cases vs 47.8% in old neglected cases[5] undergoing reduction procedures. The severity of the injury is also an important predictor for the development of osteonecrosis [4]. Also important is that during closed reduction, care is to be taken not to perform forceful manipulation as this greatly increases the risk of iatrogenic physeal separation. As is with our case gentle traction with minimal rotation is enough to reduce the joint[2,4]. The method of immobilization varies with the authors from skin traction to plaster cast application[1,11] but we found that results with plaster cast are more predictable with better patient co-operation. Child abuse is also a possible etiology of hip dislocation in children when a child presents with a doubtful history and injuries in various stages of healing[8]. In our patient, the immediate post-reduction MRI showed a small linear posterior labral tear which had healed in subsequent MRI scans taken at 6 months
Conclusion In literature there are case reports of traumatic hip dislocations in childhood (< 3 years) in the western archives. Here we present a case report of a traumatic hip dislocations in a child < 3 years in Indian population. Paediatrichip dislocations are a medical emergency which requires a great deal of suspicion to detect early and treat appropriately. Our patient had excellent recovery and functional outcome because of early reduction within the “Golden period” (6 hours).Although he had a labral tear, the soft tissues healed with immobilisation without any further intervention with no permanent disability. We therefore conclude that traumatic hip dislocations in children< 3 years is an uncommon injury but a keen lookout is a must for early diagnosis and treatment.
Clinical Paediatric hip dislocations are uncommon injuries of childhood especially with low velocity injuries. However a high degree of suspicion combined with early and prompt reduction is the keystone in management. This is to ensure a good functional outcome and prevention of complications like osteonecrosis and chondrolysis.
References
1. Meena S, Krishnapuria T, Gangari SK, Sharma P :Traumaticposterior hip dislocation in a 16 month old child: a case report and review of literature. Chin J Traumatology 2012;15(6):382-4 2. Vialle R, Odent T, Pannier S, Pauthier F, Laumonier F, Glorion C: Traumatic hip dislocation in childhood. J PediatrOrthop. 2005 mar-Apr;25(2):138-44 3. Vemulapalli KK, Dey C, Peckham T, Paterson JM :Traumatic hip dislocation in a 21 month old child. Arch Orthop trauma Surg. 2005 Sep;125(7):490-2 4. Zrig M, Mnif H, Koubaa m, Abid A: Traumatic hip dislocation in children. ActaOrthop Belg. 2009 Jun;75(3):328-33 5. Bressan S, Steiner IP, Shavit I: Emergency department diagnosis and treatment of traumatic hip dislocations in children under the age of 7 years; a 10 year review. Emerg Med J, 2014 May;31(5):425-31 6. Herrera-Soto JA, price CT :Traumatic hip dislocations in children and adolescents :pitfalls and complications. J Am AcadOrthop Surg. 2009 Jan;17(1):15-21. 7. Haverstock JP, Sanders DW, bartley DL, Lim RK :Traumatic hip dislocation in a toddler. J Emerg Med. 2013 Jul;45(1):91-4 8. Murphy W, Naranje SM, Kelly DM, Spence DS, Warner WC Jr, Beaty JH: Non accidental traumatic dislocation of the hip in a 3 year old child: a report of a rare injury.Am J Orthop (Belle Mead NJ). 2014 Aug;43(8):374-6. 9. Furuya H, Shimamura Y, Kaneko K, Sakuramoto H, Hirata K, Arai Y : Traumatic dislocation of the hip in a child caused by trivial force for age. Case Rep Orthop. 2014;2014:467246. 10. Baker JF, Leonard M, Devitt BM, Queally JM, Noel J : Traumatic hip dislocation in a 3 year old girl. PediatrEmerg Care. 2011 Dec;27(27):1178-9 11. Martinez- Guerrero JI, Olguin- Hernandez F, Cabrera A: Traumatic hip dislocation in children. Case Report of a 4 year old girl .ActaOrthop Mex. 2012 jan-feb;26(1):45-8.
| How to Cite This Article: Balasubramanian N, Babu NG, Sindhuja P. Traumatic Hip Dislocation in A Child Younger Than 3 Years- A rare Case Report And Review of Literature. Journal of Orthopaedic Case Reports 2015 April-June;5(2): 69-71. Available from:https://www.jocr.co.in/wp/2015/04/20/2250-0685-279-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com