[box type=”bio”] What to Learn from this Article?[/box]
Patients suffering from hypophosphatasia may incur fractures with trivial injuries. Their management differs with emphasis on a multi-disciplinary approach and delayed mobilization until their is radiological evidence of bone healing.
Case Report | Volume 5 | Issue 3 | JOCR July-Sep 2015 | Page 66-68 | N Sharma, E Bache, T Clare. DOI: 10.13107/jocr.2250-0685.312.
Authors: N Sharma[1], E Bache[2], T Clare[3].
[1] Department of Orthopedics, Royal Stoke Hospital, University hospital of North Midlands. UK.
[2] Department of Orthopedics, Royal Orthopedic Hospital. UK.
[3] Department of Orthopedics, Russells Hall Hospital. UK.
Address of Correspondence
Dr. Nikhil Sharma
28 Buckingham Road, Penn, Wolverhampton, WV4-5TJ, West-Midlands, UK.
Email – n-sharma@doctors.org.uk
Abstract
Introduction: We report a case of an adolescent sustaining bilateral femoral neck fractures due to a first time epileptic seizure, as a result of expansion of his known syrinx.
Case Report: A 19-year-old patient suffering from hypophosphatasia (HPP), Arnold-Chiari malformation, and a ventriculoperitoneal shunt sustained a trivial fall with profound pain and an inability to mobilize. Radiographs demonstrated a right-sided Garden-4 femoral neck and left-sided multi-fragmentary intracapsular/extracapsular fractures. The patient had previously suffered bilateral proximal femoral shaft fractures, treated with intramedullary unlocked nail fixation that was still in situ. Operative treatment with an exchange to Synthes Adolescent Lateral Recon nail was performed on the right with two Recon screws inserted into the femoral head. On the left, the existing Pedinail was preserved with an additional single screw inserted into the femoral head. In addition, 3 months of non-mobilization was required for adequate bone healing. After 1-year from time of injury, there is no avascular necrosis on radiographs and the patient is mobilizing pain-free.
Conclusion: Patients with hypophosphatasia have delayed bone healing. We recommend surgical fixation with an intramedullary device and periods of non-mobilization until there is radiographical evidence of adequate bone healing.
Keywords: Hypophosphatasia, bilateral intracapsular neck of femur fractures.
Introduction
Hypophosphatasia (HPP) is a rare metabolic disorder with a mutation occurring within the liver/bone/kidney alkaline phosphatase gene (ALPL). This leads to the production of ineffective tissue-non-specific alkaline phosphatase with resultant defective skeletal mineralization and weakened bone morphology. Bilateral femoral neck fractures occurring within young adults are rare, associated with high-energy trauma [1] and occurred more frequently in the subset of patients treated for drug-induced convulsions [2]. We report a case of a young man suffering from childhood HPP, who presented with bilateral femoral neck fractures after experiencing a first-time epileptic seizure.
Case Report
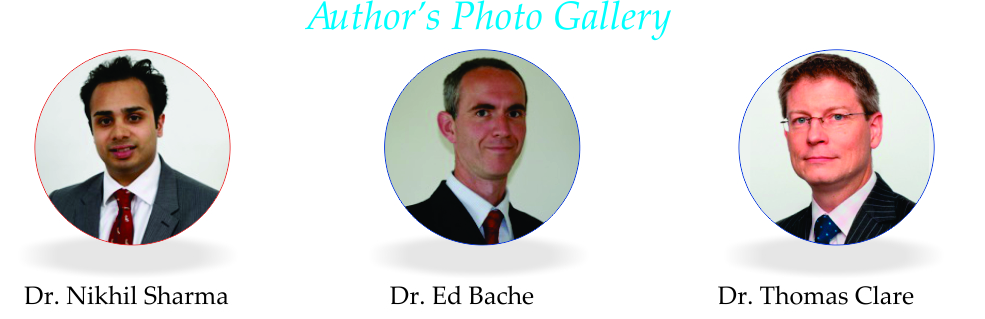
A 19-year-old adolescent presented to the emergency department after being found on his bedroom floor complaining of sudden onset excruciating bilateral hip pain and an inability to mobilize. Past medical history included childhood HPP, Arnold-Chiar malformation with syrinx, and bilateral ventriculoperitoneal shunts. The patient had previously suffered bilateral proximal femoral shaft fractures treated with intramedullary fixation in 2011 (8 mm Orthopedic Nails) and a proximal tibial fracture, treated conservatively with a sarmiento cast in 2012. Plain radiographs on admission demonstrated a right-sided Garden-4 femoral neck and left-sided multi-fragmentary intracapsular/extracapsular fractures (Fig. 1). Investigations (12-lead electrocardiogram, 24-h tape, echocardiogram, Electroencephalogram, computed tomography) confirmed a diagnosis of frontotemporal epilepsy due to an expansion of his known syrinx. Surgical fixation for both fractures was carried out sequentially under the same general anesthetic. The incision was made through the existing scar. The right-sided Garden-4 femoral neck fracture was reduced with the lead better maneuver. The previous intramedullary Pedinail was removed and exchanged for a 380 mm × 9 mm Synthes Adolescent Lateral Recon nail with two proximal locking screws within the head component. The left multi-fragmented intracapsular/extracapsular fracture was adjusted with gentle manipulation on the traction table. The existing Pedinail was preserved, its position adjusted slightly to allow a screw to be placed through it and into the femoral head. This was reinforced with 2 mm × 7 mm – cannulated screws inserted posterior to the nail (Fig 2.). Closure was performed in the usual fashion. Surgery was followed by 6 weeks of bed-rest and a further 3 months of non-mobilization. Radiographs taken 1-year after initial injury demonstrate good fracture healing with no evidence of avascular necrosis (Figs. 3 and 4.). The patient is mobilizing pain-free.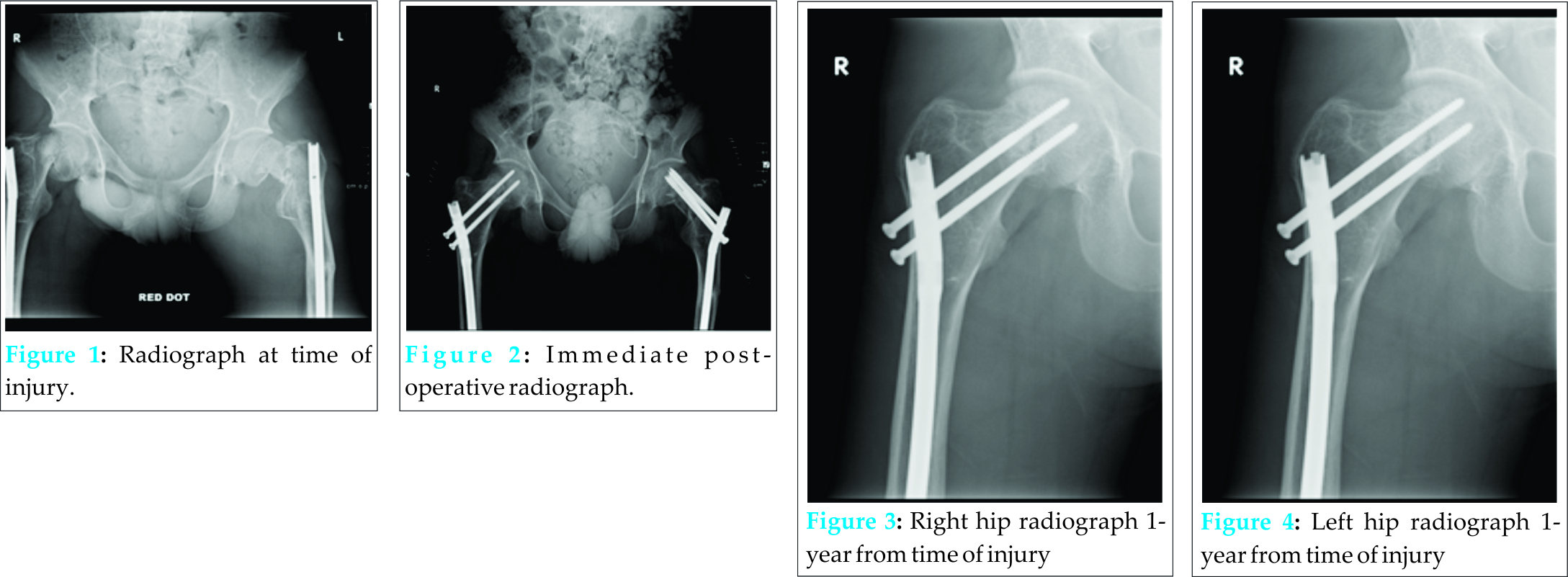
Discussion
HPP, eponymously named Rathburn disease [3] is an inborn error of metabolism. There are six clinical forms described [4]. Diagnosis is made by very low serum tissue alkaline phosphatase and high urinary phosphoethanolamine [5]. Fracture occurrence in HPP is documented within the literature and occurs due to impaired mineralization and calcification with altered non-mineralized osteoid bone matrix and subsequent degradation of bone quality [6]. There have been reports of stress and asymptomatic pseudofractures [7,8]. Bone healing in such patients is impaired [9]. Reports within the literature suggest fractures occurring in HPP patients should be managed operatively with internal fixation using intramedullary nails. This is because of their load sharing properties and to help reduce the risk of stress risers [7,10]. In this adolescent with HPP, the goal of operative treatment was to minimize bone damage in an already softened bone and to preserve bone and blood supply to maximize chances of healing. Thus, intraoperatively an attempt was made to preserve both Pedinails. The left Pedinail was successfully preserved requiring only minor adjustment to allow the insertion of a femoral head locking screw, with further reinforcement using a cannulated screw. The right-sided Garden-4 femoral neck fracture was successfully manipulated achieving good reduction allowing the femoral head to be preserved. However, it was felt that additional reinforcement was required to prevent any displacement of the femoral head. The Pedinail was exchanged for a Synthes Adolescent Lateral Recon nail with two proximal locking screws inserted within the head component. Six weeks of bed-rest and 3 months of non-mobilization were necessary to prevent any cut out of the prosthesis and screw displacement as the patient has proven to heal slowly from his previous fractures. There have been previous reports, which demonstrate delayed bone healing in HPP taking up to 3 months [10].
Conclusion
Fractures occurring in HPP patients present a challenge to the orthopedic surgeon due to soft bone quality and delayed bone healing. Reports within the literature suggest intramedullary devices be used for surgical fixation due to their load-sharing properties. We recommend coupling this with periods of non-mobilization until there is radiographical evidence of bone healing.
Clinical Message
Patients suffering from HPP have an increased propensity for fractures due to soft bone quality. Periods of non-mobilization after fracture fixation may be required until there is radiographical evidence of bone healing.
Reference
1. Thuan V Ly and Marc F Swiontkowski. Management of femoral neck fractures in young adults. Indian J orthop. 2008 Jan-Mar; 42(1): 3-12.
2. Taylor LJ, Grant SC. Bilateral fracture of the femoral neck during a hypocalcaemic convulsion. Journal of bone and joint surgery 1985;67-B(4).
3. Dickson and Horrocks. Hypophosphatasia. Journal of bone and joint surgery vol 40-B (1): 64.(1333K)
4. Etienne Mornet. Hypophosphatasia Review. Orphanet Journal of Rare Diseases 2007, 2:40 doi:10.1186/1750-1172-2-40
5. Whyte MP, Wenkert D, McAlister WH, Mughal MZ, Freemont AJ, Whitehouse R, Baildam EM, Coburn SP, Ryan LM, Mumm S. Chronic recurrent multifocal osteomyelitis mimicked in childhood hypophosphatasia. J Bone Miner Res. 2009 Aug;24(8):1493-505.
6. Barvencik F, Beil FT, Gebauer M, Busse B, Koehne T, Seitz S, Zustin J, Pogoda P, Schinke T, Amling M. Skeletal mineralization defects in adult hypophosphatasia–a clinical and histological analysis. Osteoporos Int. 2011 Oct;22(10):2667-75. Epub 2011 Jan 26.
7. F. Turturro, F. Conti, L. Giannetti, V. Di Sanzo, V. Della Chiara, L. Labianca, A. Montanaro, P. Bianco, and A. Ferretti. P33 – Hypophosphatasia: Possible Unrecognised Cause of Stress Fractures. Clin Cases Miner Bone Metab. 2010 Sep-Dec; 7(3): 237.
8. Sutton RA, Mumm S, Coburn SP, Ericson KL, Whyte MP. “Atypical femoral fractures” during bisphosphonate exposure in adult hypophosphatasia. J Bone Miner Res. 2012 May;27(5):987-94. doi: 10.1002/jbmr.1565.
9. Schalin-Jantti C, Mornet E, Lamminen A, Valimaki MJ. Parathyroid hormone treatment improves pain and fracture healing in adult hypophosphatasia. J Clinc Endocrinol Metab 2010 Dec;95(12):5174-9.
10. Anderton J.M. Orthopedic problems in adult hypophosphatasia. The Journal of bone and joint surgery vol 61-B(1), 1979.
| How to Cite This Article: Sharma N, Bache E, Clare T. Bilateral Femoral Neck Fractures in A Young Patient Suffering from Hypophosphatasia, Due to A First Time Epileptic Seizure. Journal of Orthopaedic Case Reports 2015 July – Sep;5(3):66-68 . Available from: https://www.jocr.co.in/wp/2015/07/10/2250-0685-312-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com