[box type=”bio”] What to Learn from this Article?[/box]
Implanting total hip arthroplasty in tuberculous hip osteoarthritis is a safe procedure. However, this requires the early commencement of antituberculous drugs.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 28-31 | Handy Eone Daniel, Jean Emile Bayiha, Théophyle Chunteng Nana, Olivier Kennedy Muluem, Jean Bahebeck. DOI: 10.13107/jocr.2250-0685.616
Authors: Handy Eone Daniel[1], Jean Emile Bayiha[1], Théophyle Chunteng Nana[1], Olivier Kennedy Muluem[1], Jean Bahebeck[1]
[1]Department of Orthopaedics, Unit of orthopedic surgery and traumatology of the motor apparatus Yaounde Central Hospital.
Address of Correspondence
Dr. Handy Eone Daniel,
Service de Chirurgie Orthopédique et de Traumatologie de l’Appareil Moteur, Hôpital Central de Yaoundé, Yaoundé, Cameroon.
E-mail: dhandyeone@gmail.com
Abstract
Introduction: Total hip arthroplasty (THA) remains controversial in active tuberculosis (TB) infection because of the risks of septic loosening and reactivation of the infection. We present a rare case of THA in a patient positive for the human immunodeficiency virus (HIV) with active tuberculous coxitis. The aim of this work is to share our experience and our preliminary results.
Case Report: The patient was a 53-year-old Black African woman, positive for the HIV, who was operated for implantation of a THA via the Hardinge approach indicated for a severe painful hip with restriction of joint movement and limp. A creamy-white liquid was noticed in the hip joint which was negative for urgent Gram-staining. The surgery was completed with the implantation of a hybrid THA. The post-operative period was uneventful, and she was put on antituberculous drugs following a positive histology result for TB, and to continue her antiretroviral drugs. She still has a satisfactory result for 3 years since her surgery.
Conclusion: On condition that the patient is put simultaneously on triple antibiotics and antituberculous drugs, we propose that THA could be an option in patient presenting with the association of HIV infection and active tuberculous coxitis.
Keywords: Tuberculous coxitis, total hip arthroplasty, human immunodeficiency virus, hip.
Introduction
Tuberculous coxitis still remains an indication for long-term antituberculous medications associated with surgical treatment. The principal surgical modalities include arthrodesis [1], resection arthroplasty, and total hip arthroplasty (THA) [2, 3]. Among all these surgical treatments, only the last confers a satisfactory functional status; but in an immune compromised terrain, it does not just expose to risks of early post-operative infections but also to short-term septic loosening. We have not found studies in the literature reporting the results concerning implantation of THA in human immunodeficiency virus (HIV) positive subjects with tuberculous coxitis. However, we sort for its indications in each infection separately.
The aim of this work is to share our experience and our preliminary results of a THA implanted on a 53-year-old subject with the acquired immunodeficiency syndrome (AIDS) who has been on antiretrovirals (ARV) but having an active tuberculous coxitis.
Case Report
The subject was a 53-year-old housewife, who consulted in December 2013 for inflammatory pain in the right hip evolving for 3 months controlled with non-steroidal anti-inflammatory drugs, with a walking distance of about 100 m. The medical history revealed that she is HIV infected and on triple ARV for 1 year, with a CD4 count of 473/ml, the viral load was not documented. Evaluation of the right hip showed flexion/extension of 80/20, abduction/adduction of 40/20, internal rotation/external rotation of 20/15, a trendelenburg gait, and a limb length discrepancy of 3 cm. The muscle power of the gluteus medius was 4/5. There was amyotrophy of the right quadriceps muscle. The Merle d’Aubigne and postel hip score was evaluated to be 9/18. The anterior-posterior view of the pelvic X-ray (Fig. 1) shows joint space narrowing, loss of head sphericity, shortened hip length, with no other signs of coxarthrosis (sclerosis, geodes, osteophytes). These findings coupled with the patient’s history of immunosuppression were suggestive of a coxitis, which could be due to tuberculosis (TB) infection. However, an MRI scan was not done because it was unavailable, and the patient could not afford to do it due to financial constraints. The full blood count revealed a hemoglobin level of 13 g/dl, however, the white cell count was 8000 with 45% lymphocytes and 50% neutrophiles. The rest of the laboratory investigation was unremarkable.
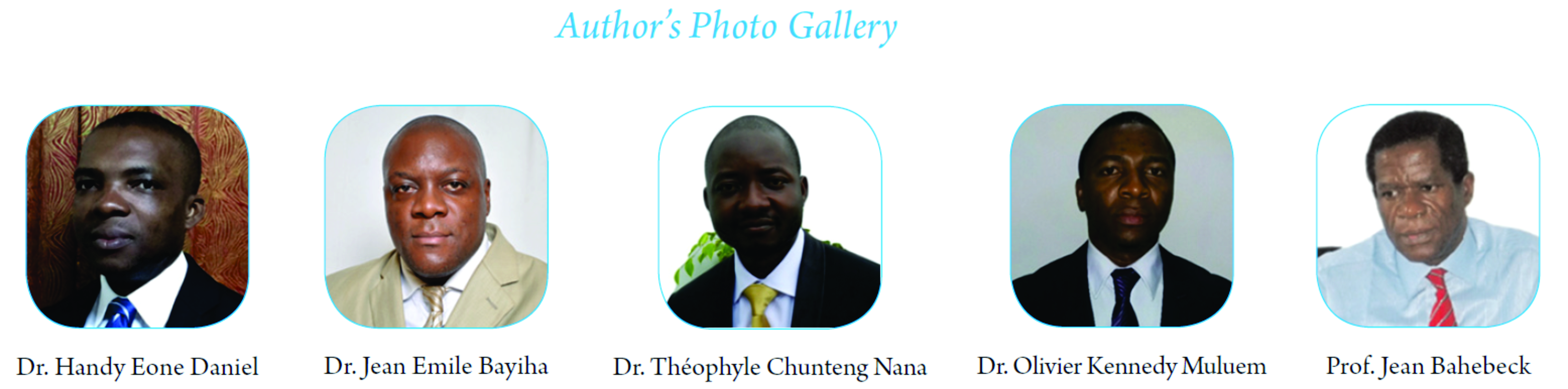
The patient was operated for implantation of a THA via the Hardinge approach. During surgery, an incident was encountered while dislocating the hip to resect the femoral head. There was a cream-white liquid that was oozing out of the hip joint (Fig. 2). A sample was rapidly collected per-operative and sent for urgent bacteriological analysis. The gram coloration was negative, the rest of the liquid was then sent for microbiological, mycobacteriological and histological analyses. The debris from reaming and the femoral head (Fig. 3) were also sent for analysis. The surgery was continued and completed with the implantation of a hybrid THA due to the fragile acetabulum; the stem was uncemented while the acetabulum was cemented (Fig. 4). The anatomopathological findings showed an active TB infection (Fig. 5).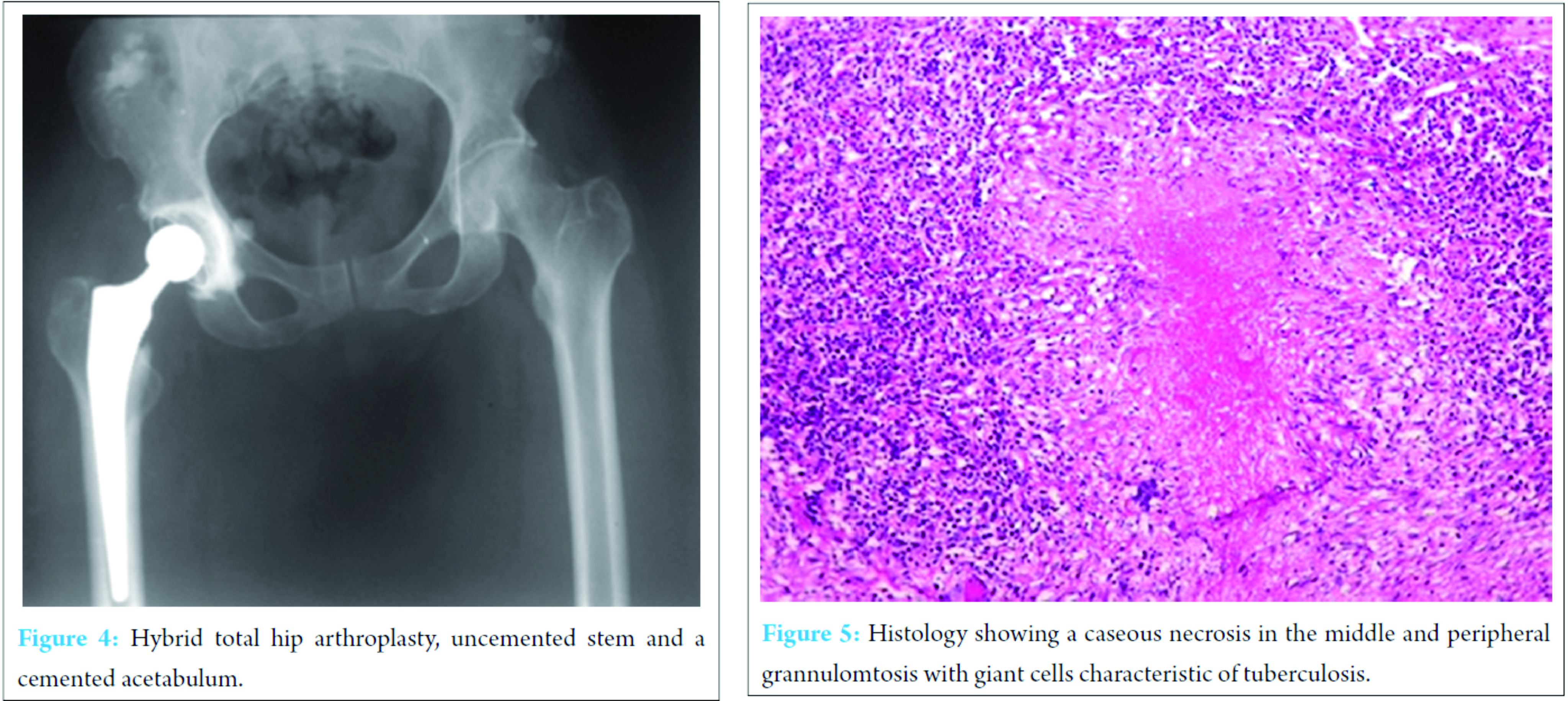 At the end of the surgery, the limb length discrepancy was corrected. The wound healing was normal, and rehabilitation commenced 24 h after surgery with isometric contractions of the gluteal and quadriceps muscles in bed. She was then verticalized the second day following surgery and walking was assisted using crutches. The patient thence continued with her ARV the same day of surgery and 10 days triple antibiotics initiated. She had a fixed combination of antituberculous drugs (isoniazid, rifampin, pyrazinamide, and ethambutol) to be taken for 12 months. 3 years after the surgery we have not noticed any relapse of the infection or any loosening.
At the end of the surgery, the limb length discrepancy was corrected. The wound healing was normal, and rehabilitation commenced 24 h after surgery with isometric contractions of the gluteal and quadriceps muscles in bed. She was then verticalized the second day following surgery and walking was assisted using crutches. The patient thence continued with her ARV the same day of surgery and 10 days triple antibiotics initiated. She had a fixed combination of antituberculous drugs (isoniazid, rifampin, pyrazinamide, and ethambutol) to be taken for 12 months. 3 years after the surgery we have not noticed any relapse of the infection or any loosening.
Discussion
This write up reports a case of THA with favorable short-term evolution in a 53-year-old female black African, with a tuberculous coxitis complicating an AIDS condition on triple ARV. To the best of our knowledge, this is the first case reported in contemporary literature. For this reason, and despite the fact that it is the only case, reporting it to the scientific community is a warranty. It should be noted that arthropathy has been found to be among the most common orthopedic pathology in HIV-positive patients [4] and could be either related to HIV-induced immunodeficiency, or due to side effects of antiviral drugs [5].
Although bacterial infection rates according to the literature are increased in HIV-infected patients who receive surgical treatment [6], our patient did not show any post-operative sepsis.
Campbell and Hoffman [7] found that patients with HIV disease are more susceptible to postoperative complications like delayed wound healing, and worsening of their disease condition, however, our patient did not have any wound complications and healed by primary intention.
Some authors have reported that implantation of prosthetic implants in active TB is controversial for fear of disease reactivation, but recent findings showed that metals could be safely used in tuberculous lesions [3, 8]. Oztürkmen et al. [9] did not observe any reactivation of disease in his 9 cases after an average follow-up of 5.6 years, all the femoral and acetabular components did not show signs of loosening. After 3 years of follow-up our patient presented with adequate bone ingrowth on X-ray films and no signs of loosening. Similarly, Wang et al. [3] had no case of hip dislocation and loosening. Other authors made similar observations [10, 11]. We carried out thorough debridement of infected tissues and post-operative antituberculous therapy as recommended by Wang et al. [3] thereby lowering the risk of reactivation.
Many authors have indicated and reported favorable results of THA on tuberculous coxitis [3, 10, 12], associated with long-term antituberculous drugs. Bahebeck et al. [13] and Harrison et al [14] have also reported favorable results of THA on HIV-positive subjects on condition that they are simultaneously on triple ARV and long-term peri-operative antibiotics. Because of the results obtained in the studies mentioned above, our experience on caseous necrosis, and a per-operative negative gram stain, we therefore decided not to do a Girdlestone resection arthroplasty but implant a THA. The histological findings comforted us as we instituted antituberculous drugs. The short- and medium-term results are satisfactory.
Conclusion
While awaiting a series of similar subjects which is difficult to assemble due to the rare nature of this association, THA could be a good surgical option on HIV-infected individuals having TB coxitis on condition that the subject is simultaneously placed on triple antibiotics and antituberculous drugs.
Authors Contributions
All the above-listed authors did actively participate in this work.
Clinical Message
It is possible to do a THA in active tuberculous coxitis in HIV-infected patients on the condition that the patient receives long-term antituberculous drugs and ARVs.
References
1. Babhulkar S, Pande S. Tuberculosis of the hip. Clin Orthop Relat Res 2002;398:93-99.
2. Kim YY, Ahn JY, Sung YB, Ko CU, Shim JC, Park HS, et al. Long-term results of Charnley low friction arthroplasty intuberculosis of the hip. J Arthroplasty 2001;211:106-110.
3. Wang Y, Wang J, Xu Z, Li Y, Wang H. Total hip arthroplasty for active tuberculosis of the hip. Int Orthop 2010;34(8):1111-1114.
4. Hoekman P, van de Perre P, Nelissen J, Kwisanga B, Bogaerts J, Kanyangabo F. Increased frequency of infection after open reduction of fractures in patients who are seropositive for human immunodeficiency virus. J Bone Joint Surg Am 1991;73(5):675-679.
5. Jellis JE. Orthopaedic surgery and HIV disease in Africa. Int Orthop 1996;20:253-256.
6. Martine-Gimeno C, Acero-Sanz J, Martin-Sastre R, Navarro-Vila C. Maxillofacial trauma: Influence of HIV-infection. J Craniomaxillofac Surg1992;20:297-302.
7. Campbell JA, Hoffman EB. Tuberculosis of the hip in children. J Bone Joint Surg Br 1995;77:319-326.
8. Govender S. The outcome of allografts and anterior instrumentation in spinal tuberculosis. Clin Orthop Relat Res 2002;398:60-66.
9. Oztürkmen Y, Karamehmetoğlu M, Leblebici C, Gökçe A, Caniklioğlu M. Cementless total hip arthroplasty for the management of tuberculosis coxitis. Arch Orthop Trauma Surg 2010;130(2):197-203.
10. Yoon TR, Rowe SM, Santosa SB, Jung ST, Seon JK. Immediate cementless total hip arthroplasty for the treatment of active tuberculosis. J Arthroplasty 2005;20(7):923-926.
11. Neogi DS, Yadav CS, Kumar A, Khan SA, Rastogi S. Total hip arthroplasty in patients with active tuberculosis of the hip with advanced arthritis. Clin Orthop Relat Res 2010;468(2):605-612.
12. Kim YH, Han DY, Park BM. Total hip arthroplasty for tuberculous coxarthrosis. J Bone Joint Surg Am 1987;69(5):718-727.
13. Bahebeck J, Eone DH, Nonga BN, Njie TK. Arthroplasty in HIV/SCD carrier. In: Fokter SK, editor. Recent Advances in Arthroplasty. InTech; 2012. Available from: http://www.intechopen.com/books/recent-advances-in-arthroplasty/arthroplasty-in-hiv-scd-carriers.
14. Harrison WJ, Lewis CP, Lavy CB. Wound healing after implant surgery in HIV-positive patients. J Bone Joint Surg Br 2002;84(6):802-806.
| How to Cite This Article: Daniel HE, Bayiha JE, Nana TC, Muluem OK, Bahebeck J. Total Hip Arthroplasty Indicated for a Tuberculous Coxitis Complicating a Controled Acquired Imunodefficiency Syndrom Condition: A Preliminary Report Concerning a Case. Journal of Orthopaedic Case Reports 2016 Nov-Dec;6(5):28-31. Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-616-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com