[box type=”bio”] What to Learn from this Article?[/box]
Custom made acrylic prosthesis is an effective alternative to endoprosthesis in the management of malignant proximal humerus tumors.
Case Report | Volume 6 | Issue 5 | JOCR November-December 2016 | Page 65-68| Kumar Amerendra Singh, Vijay Shankar, Simanchal P Mohanty DOI: 10.13107/jocr.2250-0685.636
Authors: Kumar Amerendra Singh[1], Vijay Shankar[1], Simanchal P Mohanty[1]
[1]Department of Orthopaedics, Kasturba Medical College, Manipal, Karnataka, India.
Address of Correspondence
Dr. Kumar Amerendra Singh,
Department of Orthopaedics, Kasturba Medical College, Manipal – 576 104, Karnataka, India.
E-mail: amerendra2@gmail.com
Abstract
Introduction: Proximal humerus is a common site for malignant bone tumors. The mainstay of treatment involves radical excision and reconstruction. Reconstructing the proximal humerus is quite challenging. The best modality of treatment is a modular endoprosthesis which is expensive. Here, we present two cases where the proximal humerus was reconstructed with acrylic prosthesis.
Case Report: A 19-year-old male and 51-year-old lady from India presented with painful swellings of the upper arm with a clinical diagnosis of Ewing’s sarcoma arising from the left humerus and secondary metastatic tumor of proximal end of right humerus, respectively. They were treated with radical excision of tumor, and the upper two-third of the humerus were reconstructed using custom made acrylic endoprostheses.
Conclusion: Reconstruction of proximal humeral defect with custom made acrylic prosthesis is less expensive and an effective alternative to modular endoprosthesis, which can be used in developing countries.
Keywords: Acrylic prosthesis, proximal humerus, malignant tumors
Introduction
Proximal humerus is not an uncommon site for malignant bone tumours [1]. Recent trend in the management of malignant bone tumours is in the form of radical excision and reconstruction.
Reconstruction of proximal end of humerus is quite challenging as the outcome is to satisfactorily restore shoulder, elbow and hand functions. A variety of modalities are available for reconstruction of these defects such as osteoarticular allografts, modular endoprosthesis, resection arthrodesis and other prosthetic composites [3]. At present, most preferred among these is a modular segmental endoprosthesis. However, in developing countries they are quite expensive and difficult to procure. A simpler and less expensive alternative includes a custom made endoprosthesis fabricated out of acrylic material. We present two such cases which provided satisfactory functional results.
Case presentation
Prosthesis preparation:
For preparation of this prosthesis an approximate size of the humeral head and its length was calculated from the radiographs of the normal side. An age and sex matched dry humerus specimen of similar size belonging to the same side was procured from the Anatomy Department. Length of the humerus to be resected was determined from preoperative MRI. A negative mould was prepared using the dry humerus specimen. The prosthesis was fabricated out of dental acrylic material using the negative mould. A humeral interlocking nail was incorporated into the acrylic prosthesis. Three holes were drilled into the proximal end of prosthesis for attachment of rotator cuff muscles and the entire construct was gas sterilized. After resection of tumour, the medullary canal of distal humerus was reamed for introduction of nail. Reamed material was sent for HPE examination. Bone cement was packed into the canal and the nail was locked following insertion. The rotator cuff muscles were anchored to the prosthesis through the premade holes.
Case 1:
A young man aged nineteen years presented with complains of pain over left arm since three months. He had a trivial fall three months back for which the limb was immobilised in a cast. Following removal of the cast, he noticed a swelling over left arm. He was afebrile; however there was history of loss of weight and appetite. Physical and systemic examination did not reveal any abnormalities. There were no other swellings elsewhere.
On examination, a firm, globular 10cmx5cmx 5cm was present over the anterolateral aspect of proximal one third of left arm. The swelling was tender and abnormal mobility was present.
There was no distal neurovascular deficit.
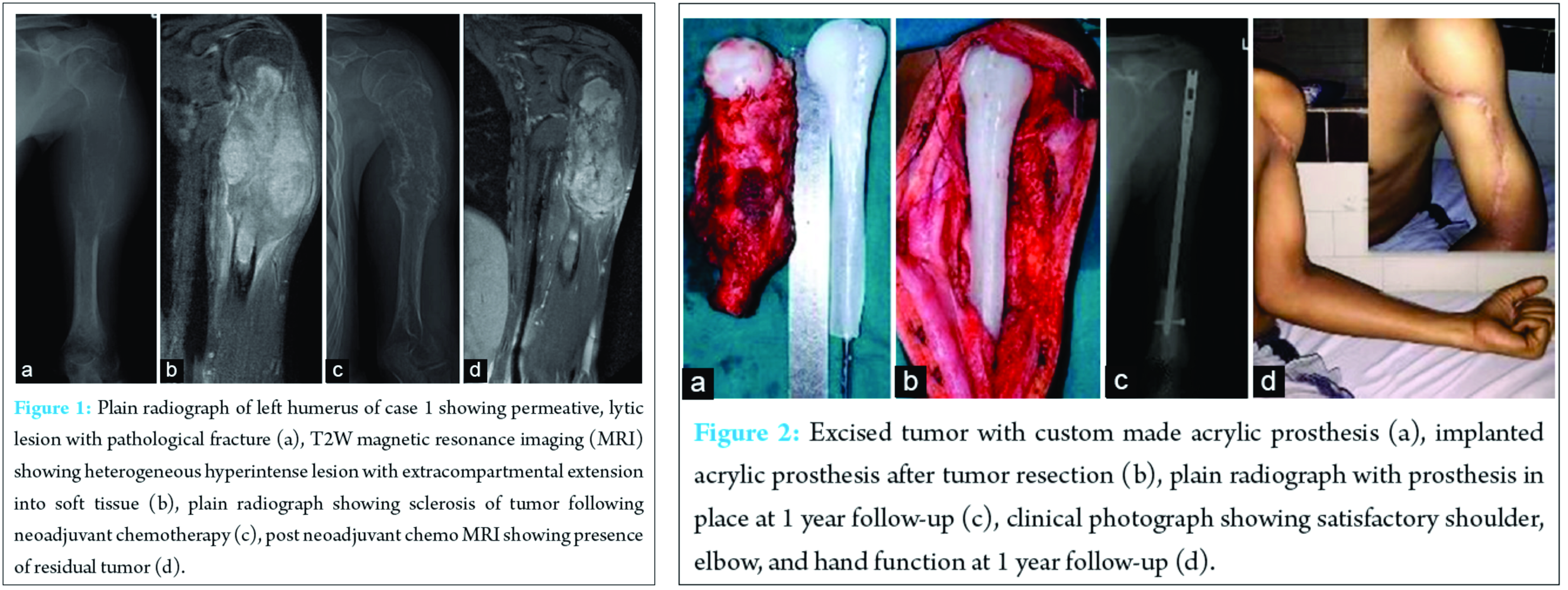
Routine blood investigations were normal. Plain radiographs of left humerus showed a permeative, destructive lesion involving the upper and middle one third with pathological fracture (Fig. 1A). Chest radiograph was normal. Magnetic resonance imaging revealed altered marrow signal intensity in the diaphysis and proximal metaphysis of left humerus. There was a large soft tissue component which was hypointense on T1, heterogeneously hyperintense on T2 and STIR images (Fig. 1B). He underwent an incisional biopsy. The histopathological (HPE) diagnosis was Ewing’s sarcoma. Immunohistochemistry showed positivity for CD99 and Bcl-2. Positron emission tomographic scans demonstrated no evidence of pulmonary metastasis. The tumour was staged as IIB according to Musculoskeletal Tumour Society Staging.
He underwent four cycles of neoadjuvant chemotherapy with Vincristine, Adriamycin and Cyclophosphamide (VAC). Even though clinically and radiologically the tumour showed features of regression, post chemotherapy MRI revealed presence of residual tumour (Fig. 1 C, D).
He underwent radical excision of the tumour (Malawer type 1 resection) [2]. The defect was reconstructed with custom made acrylic prosthesis (Fig. 2A, B). The entire tumour mass and the margins were sent for biopsy.
The specimen sent for HPE showed features of Ewing’s sarcoma; however margins were free of tumour. Postoperatively, he received sixteen cycles of adjuvant chemotherapy with VAC, Ifosphamide and Etoposide. At one year followup he was pain free with shoulder abduction of 20 degrees, external rotation of 40 degrees and flexion of 30 degrees. He had good elbow, wrist and hand movements with excellent power grip. (Fig. 2 C, D).
Case 2:
A 51 year old lady who had undergone total thyroidectomy and received a complete course of I131 ablation therapy for follicular carcinoma of thyroid five years ago presented with painful swelling over her right upper arm for past three months. The swelling was gradually increasing in size. At the time of presentation the pain was severe enough to disturb her sleep and activities of daily living. On examination, there was a diffuse swelling extending from the shoulder to middle one third of arm. The swelling was tender, firm in consistency with abnormal mobility.
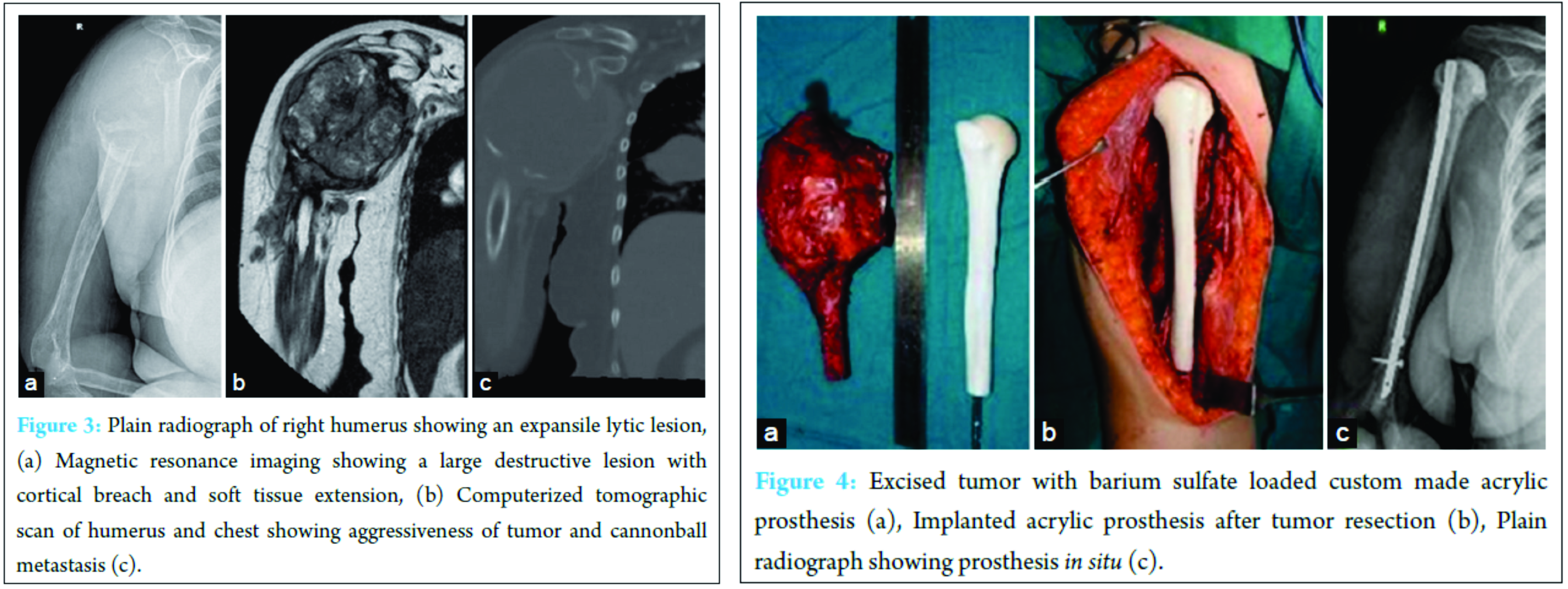
Routine blood investigations and thyroid function tests were within normal limits. Plain radiographs of right humerus showed an expansile lytic lesion causing complete destruction of the head, neck and proximal half of right humerus. (Fig. 3A) MRI revealed a large expansile, lytic lesion which was hyperintense on T2 and iso to hyperintense on T1 image. There was a breach in the cortex circumferentially with infiltration into muscles of proximal arm. (Fig. 3B)
Posteriorly, the lesion was seen to abut the radial nerve. Contrast enhanced computerised tomographic scan of chest showed multiple cannon ball type of metastasis. (Fig. 3C)
Radical excision of tumour (Malawer type 1 resection) was done and the upper end of humerus was reconstructed with a custom made barium sulphate loaded acrylic prosthesis. (Fig. 4)
The biopsy was positive for metastatic follicular carcinoma of thyroid. Postoperatively, patient developed transient radial nerve paralysis which slowly recovered. She was completely free of pain and by four weeks had satisfactory shoulder, elbow and hand function.
Discussion
Proximal humerus is a common site for malignant bone tumours [1]. In the pre-chemotherapy era tumours arising from the proximal humerus were treated with surgical ablation. However with the advent of radiotherapy and chemotherapy, limb salvage surgeries
have become the gold standard. The ultimate goal of surgical treatment is en-mass removal of the tumour, preservation of the limb with satisfactory shoulder, elbow and hand functions [3]. This can be achieved by osteoarticular allografts, acrylic prosthesis, allograft prosthesis composite, modular endoprosthesis etc. [3].
Allografts and modular endoprosthesis are expensive. They are not easily available in developing countries. The use of acrylic prosthesis for reconstruction following removal of bone tumours dates back to 1964 [4]. However when used for lower limb reconstruction, the failure rate is high. Being a nonweight bearing bone, humerus is subjected to less biomechanical stress [5].
Hence acrylic prostheses have a role in reconstruction of these defects. These prostheses are simpler, less expensive and hence more suitable in developing countries where most of the patients cannot afford a modular endoprosthesis.
Cement nail prosthesis where a Kuntcher’s nail wrapped in bone cement and used as a spacer has been described in the literature [5]. We utilized a similar concept where custom made acrylic prosthesis shaped according to the anatomy of the proximal humerus was used. Using this technique a satisfactory range of shoulder movements was obtained. Both cases were pain free following surgery with good upper limb function.
Proximal humerus is a common site for malignant bone tumours [1]. In the pre-chemotherapy era tumours arising from the proximal humerus were treated with surgical ablation. However with the advent of radiotherapy and chemotherapy, limb salvage surgeries have become the gold standard. The ultimate goal of surgical treatment is en-mass removal of the tumour, preservation of the limb with satisfactory shoulder, elbow and hand functions [3]. This can be achieved by osteoarticular allografts, acrylic prosthesis, allograft prosthesis composite, modular endoprosthesis etc. [3].
Allografts and modular endoprosthesis are expensive. They are not easily available in developing countries. The use of acrylic prosthesis for reconstruction following removal of bone tumours dates back to 1964 [4]. However when used for lower limb reconstruction, the failure rate is high. Being a nonweight bearing bone, humerus is subjected to less biomechanical stress [5].
Hence acrylic prostheses have a role in reconstruction of these defects. These prostheses are
simpler, less expensive and hence more suitable in developing countries where most of the patients cannot afford a modular endoprosthesis.
Cement nail prosthesis where a Kuntcher’s nail wrapped in bone cement and used as a spacer has been described in the literature [5]. We utilized a similar concept where custom made acrylic prosthesis shaped according to the anatomy of the proximal humerus was used. For preparation of this prosthesis an approximate size of the humeral head and its length was calculated from the radiographs of the normal side. An age and sex matched dry humerus specimen of similar size belonging to the same side was procured from the Anatomy Department. Length of the humerus to be resected was determined from preoperative MRI. A negative mould was prepared using the dry humerus specimen. The prosthesis was fabricated out of acrylic material using the negative mould. A humeral interlocking nail was incorporated into the acrylic prosthesis. Three holes were drilled into the proximal end of prosthesis for attachment of rotator cuff muscles and the entire construct was gas sterilized. After resection of tumour, the medullary canal of distal humerus was reamed for introduction of nail. Reamed material was sent for HPE examination.
Bone cement was packed into the canal and the nail was locked following insertion. The rotator cuff muscles were anchored to the prosthesis through the premade holes. Using this technique a satisfactory range of shoulder movements was obtained. Both cases were pain free following surgery with good upper limb function.
Conclusion
Recent trend in the management of aggressive and malignant bone tumors is radical excision and reconstruction with modular endoprosthesis. Limb salvage procedures for
proximal humeral tumours aim at restoration of satisfactory shoulder, elbow and hand function. Reconstruction of proximal humeral defect with custom made acrylic prosthesis is a less expensive and an effective alternative to modular endoprosthesis, which can be used in developing countries.
Clinical message
Treatment of malignant tumours of proximal end of humerus involves radical excision and reconstruction. Though many treatment modalities are available, custom made acrylic prosthesis is a simple and less expensive alternative providing good shoulder, elbow and hand function.
References
1. Dahlin DC. Bone tumors: general aspects and data on 6221 cases. Thomas, Springfield 1978.
2. Malawer MM, Sugarbaker PH: Musculoskeletal Cancer Surgery: Treatment of Sarcomas and Allied Disease. Kluwer Academic Publishers, 2001.
3. Rödl RW, Gosheger G, Gebert C, Lindner N, Ozaki T, Winkelmann W. Reconstruction of the proximal humerus after wide resection of tumours. J Bone Joint Surg (Br) 2002; 84:1004–1008.
4. Rainer I. Kotz. Progress in musculoskeletal oncology from 1922 – 2012. Int Orthop. 2014 May; 38(5): 1113–1122.
5. Kundu ZS, Gogna P, Gupta V, Kamboj P, Singla R, Sangwan SS. Proximal humeral reconstruction using nail cement spacer in primary and metastatic tum our of proximal humerus. Strategies Trauma Limb Reconstr. 2013 Nov; 8(3):149-54.
| How to Cite This Article: Singh KA, Shankar V, Mohanty SP. Reconstruction of Proximal Humerus Using Custom Made Acrylic Prosthesis in Malignant Bone Tumors. Journal of Orthopaedic Case Reports 2016 Nov-Dec ;6(5). Available from: https://www.jocr.co.in/wp/2016/11/10/2250-0685-636-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com