[box type=”bio”] What to Learn from this Article?[/box]
Large head THR using MIS technique in an above-knee amputee with ipsilateral hip arthritis, minimizes post-operative complications, and affords early rehabilitation.
Case Report | Volume 7 | Issue 2 | JOCR March – April 2017 | Page 3-6| Sanjeev Patnaik, Biswaranjan Nayak, Akshaya Kumar Sahoo, Nabin Kumar Sahu. DOI: 10.13107/jocr.2250-0685.722
Authors: Sanjeev Patnaik [1], Biswaranjan Nayak [1], Akshaya Kumar Sahoo [1], Nabin Kumar Sahu [1].
[1] Department of Orthopaedics, Apollo Hospital, Bhubaneswar, Odisha, India.
Address of Correspondence
Dr. Sanjeev Patnaik,
Department of Orthopaedics, Apollo Hospital, Bhubaneswar – 751 005, Odisha, India.
E-mail: sportho1973@yahoo.co.in
Abstract
Introduction: Total hip replacement (THR) is a highly successful operation in alleviating pain and improving the overall function of the hip, in end-stage arthritis of the hip, in otherwise fit patients. However, THR as a surgical option in post-traumatic hip arthritis with ipsilateral above-knee amputation is rarely reported.
Case Report: We are presenting a case report of a 30-year-old male, who had previously underwent an above-knee amputation due to road-traffic accident, presenting 24 h after the injury with segmental fracture femur and popliteal artery laceration, for which the limb could not be salvaged. He had an impacted anteroinferior dislocation of the ipsilateral hip with significant cartilage damage of the femoral head which required open reduction. Subsequently, he developed traumatic arthritis of the involved hip which required conversion to an uncemented THR, using a minimally invasive (MIS) anterolateral approach. The preoperative management, surgical technique, and postoperative rehabilitation are described to highlight the technical challenges, these lower limb amputees may present along with review of literature of such rare cases.
Conclusion: THR in an above-knee amputee with posttraumatic hip arthritis using MIS technique is an encouraging surgical option for early functional recovery and minimizing surgical complications.
Keywords: Total hip replacement, above-knee amputation, post-traumatic arthritis, minimally invasive surgery.
Introduction
Total hip replacement (THR) is a highly successful operation in alleviating pain and improving the overall function of the hip, especially in end-stage arthritis of the hip, in otherwise fit patients. However, THR as a surgical option in an ipsilateral above-knee amputation is rare with limited literature about the clinical outcomes [1, 2, 3]. In this article, we are presenting a case of a 30-year-old male patient who underwent cement-less THR of the ipsilateral above-knee amputated limb due to early development of traumatic arthritis of the hip. The cause of the arthritis was posttraumatic hip dislocation following a road-traffic accident with significant cartilage damage which presented late and required open reduction. He sustained segmental fracture of femur with popliteal artery laceration, for which an above-knee amputation was done. The challenges faced during surgery, the modifications in rehabilitation protocol to ambulate the patient along with a review of limited literature are presented.
Case Report
We present a case of 30-year-old male who had a road-traffic accident presenting to us from a remote peripheral center after 24 h of the injury. He sustained bilateral lower limb injuries. On presentation, he was conscious and coherent but in hypovolemic shock. He was managed as per advanced trauma life support guidelines and was made hemodynamically stable. Clinical examination revealed an unreduced right hip dislocation, fracture deformities of both the thighs, an open wound over lower third of right thigh with bruising and swelling, and an open wound over anterior right leg. The right lower limb continued to be cold and clammy after hemodynamic stabilization, with absent distal pulses below the knee. Trauma series X-rays were taken along with a computed tomography angiogram (Fig. 1) which revealed a segmental fracture of the right femur with anteroinferior dislocation of the hip, fracture of superior iliopubic rami, with obliteration of the femoral artery at the distal femur and a shaft femur fracture of the left thigh. After hematological and serological work up and multidisciplinary assessment and keeping in mind the delayed presentation (beyond 24 h), the decision to go for above-knee amputation of right lower limb was taken and the patient was planned for emergency surgery. On exploration, the popliteal artery was seen to be lacerated at multiple points with distal thrombosis and above-knee amputation was carried out. The right hip was impacted in the obturator foramen which could not be reduced by closed attempts, hence required open reduction, done by a posterior approach. The head of the femur had impaction injuries with full thickness cartilage loss in the superolateral region. An external fixator was given to stabilize the left femur fracture, which was later converted to interlocking nailing at 5th postoperative day. The patient had an uneventful recovery and underwent supervised physiotherapy. At 2-month follow-up, when the patient was advised for weight bearing with an above-knee prosthesis for amputated right lower limb along with axillary crutches, he complained of severe pain in the right hip and was unable to weight bear. Further 1 month of non-weight bearing was advised to heal the rami fracture. Radiographs of the right hip at 3-month follow-up showed an evidence of posttraumatic arthritis and deformed head of femur (Fig. 2). To alleviate his painful hip and mobilize the patient, a decision of THR was taken.
Surgical technique
The patient was put in a left lateral decubitus position on normal OT table, secured with anterior and posterior supports acting over the pelvis. Prepping and draping of the stump were done. The procedure was carried out through a minimally invasive (MIS) anterolateral approach as these patients have a high propensity for postoperative dislocation during early rehabilitation period with the above-knee orthosis. A 8 cm incision was made starting from trochanteric ridge midway from anterior and posterior trochanteric borders extending around 4 cm proximal to tip of the greater trochanter. Subcutaneous tissue and fascia lata were divided in line of incision. Intermuscular dissection was done digitally between the gluteus medius and tensor fascia lata. Anterior joint capsule was incised in line of femoral neck. Dislocation of the hip and positioning of the femur was aided by that placement of a bone clamp below the lesser trochanteric area for manipulation. The clamp also acted as a landmark for the insertion of the femoral stem in correct version (Fig. 3).
The residual femoral stump measured 165 mm, and hence, we selected a 130 mm cementless femoral stem without collar (Corail® DePuy – Synthes). A 54 mm porous coated un-cemented acetabular shell (Pinnacle®) was aligned with the transverse acetabular ligament and appropriate inclination, transfixed with two 6.5 mm cancellous screws and a 36 mm insert (Biolox® Delta Ceramax™) was used. After trials, a 36 mm ceramic femoral head (Biolox® Delta Ceramax™) was impacted and the hip was reduced. The capsule was repaired and wound closed in layers over a suction drain.
Results
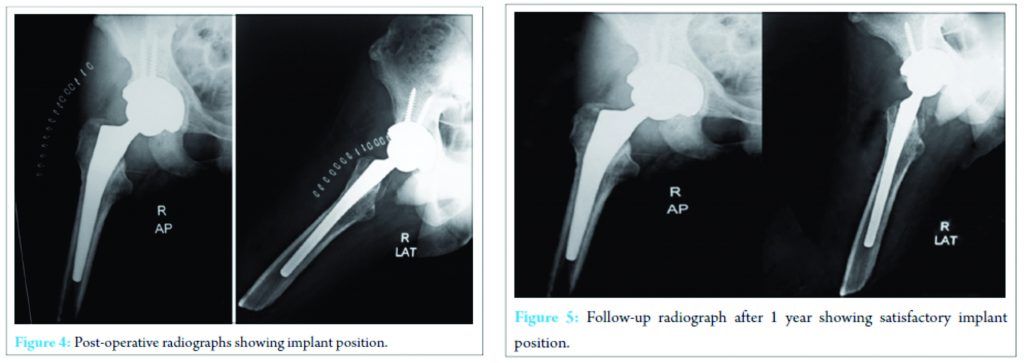
The patient tolerated the procedure well. The immediate postoperative period was uneventful. There was no infection, deep vein thrombosis, dislocation, or any other major complications. Postoperative radiographs showed proper placement of prosthesis (Fig. 4). He was allowed to be seated and perform isometric exercises after 48 hours of the procedure. He stayed in the hospital for 2 weeks till staple removal. During his hospitalization, he underwent supervised physiotherapy and was allowed full weight-bearing from postoperative day 2 with the help of previous exo-prosthesis and walking aid. He was followed up regularly till 12 months (Fig. 5). Harris hip score improved from preoperatively 36-80 at last follow-up. The patient continues to walk painlessly without any walking aid. X-ray at last follow-up shows well-incorporated femoral and acetabular components without any sign of osteolysis or subsidence.
Discussion
Secondary post traumatic arthritis in an ipsilateral above-knee amputee, especially in a younger individual, poses a catastrophe, both physiologically and psychologically. The incidence of hip osteoarthritis in amputated patients varies from 5% to 61% and in the long term, the risk to develop hip osteoarthritis compared with general population is double in the non-amputated limb and 6 times higher in the amputated limb and above-knee amputation has a greater propensity to develop arthritis than below-knee amputation [4]. Keeping the above consideration in mind, acementless THR was planned. The first 6 weeks post-THR in an amputee patient is critical with respect to standard hip precautions to avoid dislocation, especially while placing and removing their exoprosthesis [5]. Hence, the decision was taken to use a MIS anterolateral approach, which uses the intermuscular interval between the tensor fascia lata and the gluteus medius. It leaves the abductor muscles, the posterior capsule, and the short external rotators intact permitting acceleration of the postoperative rehabilitation with less perioperative complications, especially dislocation [6, 7]. We also decided to use large femoral head (36 mm) to minimize chances of dislocation [8, 9]. Careful preoperative planning is required, especially preoperative templating using radiographs with appropriate magnification to assess the length of the femoral stump and width of the medullary canal to ensure correct sizing of femoral stem to obtain a good primary stability and osteointegration of the prosthesis. Main challenges faced intraoperatively in such above-knee amputee cases are related to femoral manipulation, dislocation of femoral head, and subsequent relocation and ensuring proper implant positioning due to lack of references such as the knee or the leg axis to obtain appropriate version of the implant. Malpositioning of components is not desirable as it leads to higher risk of dislocation, compromised component survivorship, and altered gait kinematics [10]. To overcome these shortcomings, we used a femoral bone clamp just distal to the lesser trochanter to carry out the femoral manipulations and the lesser trochanter served as a guide for proper femoral anteversion during insertion of the femoral stem. Patients with lower extremity amputations in need of ipsilateral total hip arthroplasty present with additional challenges with regard to their acute postoperative care and need a modified rehabilitation program. Turney et al. demonstrated that below-knee amputees generally gain better mobility than above-knee amputees [11]. Above-knee amputees are prone to develop flexion contracture and prevention of such contractures by focusing on muscle strengthening exercises should be emphasized.
Conclusion
THR using MIS technique is an encouraging surgical option in ipsilateral post traumatic arthritis of hip, to alleviate pain and initiate early mobilization along with preserving the limited but precious functional capacity. Being an unusual case and due to limited literature of similar cases, there are no guidelines or evidence that could direct the therapeutic plan. Larger series are needed with long-term follow-up to obtain conclusive results.
Clinical Message
Total hip replacement using minimally invasive technique in a posttraumatic arthritic hip with above-knee amputation is an encouraging surgical option for early functional outcome and minimizing surgical morbidity.
References
1. Leonard M, Nicholson P. Total hip arthroplasty in a patient with arthrogryphosis and an ipsilateral above knee amputation. Hip Int 2010;20(4):559-561.
2. Sathappan SS, Wee J, Ginat D, Teicher M, Meere P, Di Cesare PE. Total hip arthroplasty in above-knee amputees: A case report. Am J Orthop (Belle Mead NJ) 2011;40(2):E17-E19.
3. Diamond OJ, Mullan CJ, McAlinden MG, Brown JG. Total hip arthroplasty following an ipsilateral above knee amputation. Hip Int 2013;23(1):104-107.
4. Kulkarni J, Adams J, Thomas E, Silman A. Association between amputation, arthritis and osteopenia in British male war veterans with major lower limb amputations. Clin Rehabil 1998;12(4):348-353.
5. Nejat EJ, Meyer A, Sánchez PM, Schaefer SH, Westrich GH. Total hip arthroplasty and rehabilitation in ambulatory lower extremity amputees – A case series. Iowa Orthop J 2005;25:38-41.
6. Laffosse JM, Chiron P, Molinier F, Bensafi H, Puget J. Prospective and comparative study of the anterolateral mini-invasive approach versus minimally invasive posterior approach for primary total hip replacement. Early results. Int Orthop 2007;31(5):597-603.
7. Berger RA. Mini-incision total hip replacement using an anterolateral approach: Technique and results. Orthop Clin North Am 2004;35:143-151.
8. Howie DW, Holubowycz OT, Middleton R; Large Articulation Study Group. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: A randomized controlled trial. J Bone Joint Surg Am 2012;94(12):1095-1102.
9. Amstutz HC, Le Duff MJ, Beaulé PE. Prevention and treatment of dislocation after total hip replacement using large diameter balls. Clin Orthop Relat Res 2004;108-116.
10. Malagelada F, Coll Rivas M, Jiménez Obach A, Auleda J, Guirao L, Pleguezuelos E. Total hip replacement in an ipsilateral above-the-knee amputation: Surgical technique, rehabilitation, and review of the literature. Int J Low Extrem Wounds 2013;12(1):39-43.
11. Turney BW, Kent SJ, Walker RT, Loftus IM. Amputations: No longer the end of the road. J R Coll Surg Edinb 2001;46:271-273.
 |
 |
 |
 |
| Dr Sanjeev Patnaik | Dr Biswaranjan Nayak | Dr Nabin Kumar Sahu | Dr Akshaya Kumar Sahoo |
| How to Cite This Article: Patnaik S, Nayak B, Sahoo AK, Sahu NK. Minimally Invasive Total Hip Replacement in an Ipsilateral Post-traumatic above-knee Amputation: A Case Report. Journal of Orthopaedic Case Reports 2017 Mar-Apr;7(2):3-6 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com