[box type=”bio”] What to Learn from this Article?[/box]
Dual mobility cups can be used to provide increased stability for patients undergoing total hip arthroplasty, but intraprosthetic dislocation can still occur. In the setting of a dislocated total hip arthroplasty with a dual-mobility cup treated with closed reduction, surgeons should scrutinize post-reduction radiographs for signs of intraprosthetic dislocation and consider revision of components if acetabular cup position is the cause of dislocation.
Case Report | Volume 7 | Issue 2 | JOCR March – April 2017 | Page 21-24| Vineet Tyagi, Oluwaseun Akinbo. DOI: 10.13107/jocr.2250-0685.732
Authors: Vineet Tyagi[1], Oluwaseun Akinbo[1]
[1] Department of Orthopaedics and Rehabilitation, Yale School of Medicine, New Haven, CT, USA.
Address of Correspondence
Dr. Vineet Tyagi, 47 College Street, New Haven, CT, USA.
E-mail: vineet.tyagi@yale.edu
Abstract
Introduction: The concept of a dual mobility (DM) cup has been in existence for more than 40 years and was initially popularized in Europe. Only recently has it started to garner attention in the United States. Its design, consisting of a small femoral head articulating within a larger polyethylene (PE) insert, which articulates with an outer shell, has found increasing use in patients that are at risk for post-operative dislocations. This case report describes a case of recurrent total hip arthroplasty (THA) dislocation managed with the implantation of a DM cup with an acute intraprosthetic dislocation of the DM construct.
Case Report: A 52-year-old woman underwent an uneventful left THA through a posterior approach. Within 6 weeks of her surgery, she had four dislocations, managed with closed reductions. She then underwent an open revision of her acetabular component with conversion to a DM construct. 5 weeks after her revision, she had another dislocation treated with closed reduction in the operating room, with the resultant eccentric location of the femoral head in the acetabular component. Computed tomography (CT) confirmed intraprosthetic dislocation with the PE liner lodged in the gluteal tissue. She was taken to the operating room with a plan to revise her acetabular component to another DM construct, but with an increase in the anteversion despite initial anteversion being “appropriate” on CT imaging. Intraoperatively, the PE liner was embedded in gluteal tissue as depicted on the CT. The abductors were intact. There was no impingement in extension and maximal external rotation when trialed with a conventional head/liner construct. A new DM construct was then implanted.
Conclusion: Intraprosthetic dislocation is a rare occurrence and unique complication to DM constructs. It is not common in the short-term setting postoperatively to our knowledge, and this case report represents an early report of intraprosthetic dislocation in the literature. Care should be taken during reduction of dislocated DM constructs to avoid intraprosthetic dislocations. Open revisions can be managed with revisions to another DM construct or to a constrained liner construct to maximize stability.
Keywords: Arthroplasty, dislocation, hip, intraprosthetic dislocation, retentive failure, total.
Introduction
Dislocations represent one of the more common post-operative complications seen after total hip arthroplasty (THA) with estimates ranging from 0.2% to 7% in primary cases and as high as 25% in revision surgeries [1]. In the early 1970s, Giles Bousquet developed a dual mobility (DM) acetabular cup with the goal of reducing dislocation rates. The DM design consists of two articulations: A large diameter polyethylene (PE) articulation with a metal cup and a smaller articulation between a modular femoral head and the PE liner [2]. In a DM construct, when impingement of the smaller articulation occurs, an additional range of motion is available through the articulation of the PE liner within the metal cup. Thus, DM constructs increase the head-neck ratio, and also increase the jump distance; this effectively decreases the dislocation rate of THA with this construct [3].
While introduced over 40 years ago in Europe, only recently has the DM construct been introduced in the United States market. There are currently several different DM constructs available in the United States to include the anatomic DM (Stryker Orthopaedics, Mahwah, New Jersey) and modular DM (Stryker Orthopaedics, Mahwah, New Jersey), the POLARCUP (Smith & Nephew, Memphis, Tennessee), and the active articulation (Biomet Orthopaedics, Warsaw, Indiana). Although the goal of these constructs is to reduce the dislocation, there are a few reports in the literature that detail a complication unique to DM constructs – intraprosthetic dislocation. Intraprosthetic dislocation, also known as retentive failure, is a form of dislocation that occurs when the femoral head has dissociated from the mobile-bearing PE liner often times causing the large PE liner to be lodged in soft tissue. This is typically a medium to long-term complication [3, 4].
Case Report
A 52-year-old woman with a history of alcohol abuse underwent an uneventful left THA through a posterior approach. This was complicated by four dislocations, managed with closed reductions, within 6 weeks of her surgery. She underwent an open revision of her acetabular component with conversion to a DM construct (Stryker, Mahwah, New Jersey).
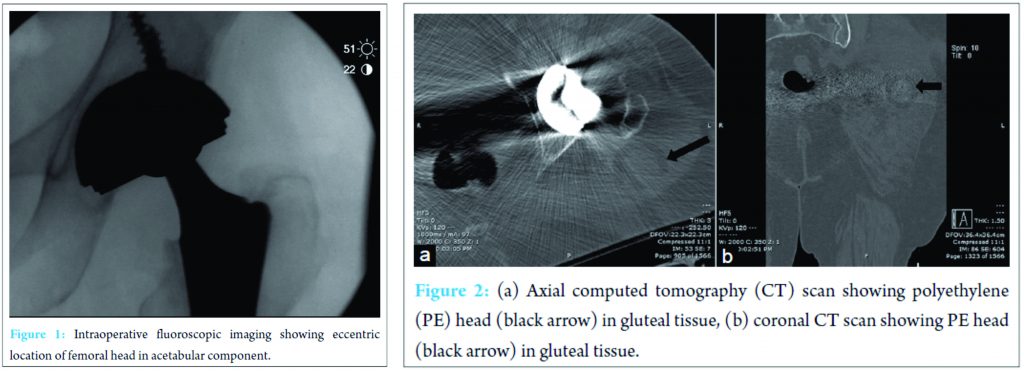
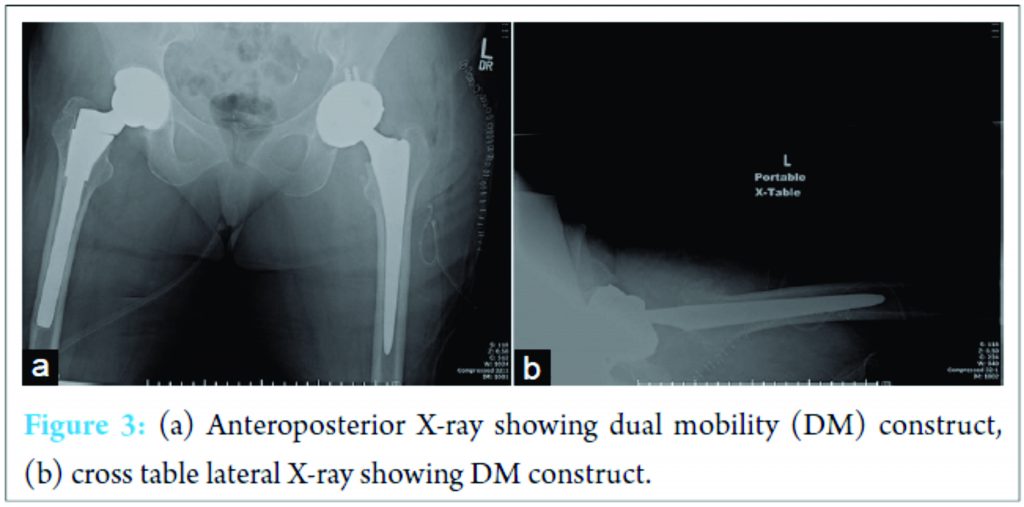
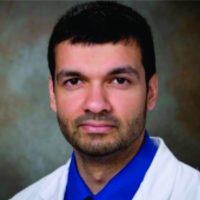
Five weeks after her revision procedure, her left leg was noted to be shorter than the contralateral leg 4 days after admission to an outside hospital for altered mental status. Radiographs confirmed a dislocation. A closed reduction was attempted in the operating room with the resultant eccentric location of the femoral head in the acetabular component (Fig. 1). She was transferred to our facility for definitive treatment. Computed tomography (CT) confirmed intraprosthetic dislocation with the PE liner lodged in the gluteal tissue (Fig. 2a and b). Anteversion of the acetabular component was measured to be about 15°. She was taken to the operating room with plan to revise her acetabular component to another Stryker DM construct, but with an increase in the anteversion despite initial anteversion being “appropriate” on CT imaging. Her femoral stem (Synergy; Smith and Nephew, Memphis Tennessee) was well fixed and appropriately anteverted; it was left in place. Intraoperatively, the PE liner was embedded in gluteal tissue as depicted on the CT. There was no evidence of damage to the liner. The abductors were intact. There was no impingement in extension and maximal external rotation (after implantation of new acetabular component in increased anteversion) when trialed with a conventional head/liner construct. A new DM construct was then implanted (Fig. 3a and b) with a new femoral head; post-operative recovery was uneventful. The patient did well for 18 months, was able to lose her ambulatory aid when walking, and able to walk without significant pain issues. Unfortunately, she developed a chronic infection after 18 months and was managed with a resection arthroplasty and implantation of an antibiotic spacer.
Discussion
Intraprosthetic dislocation is usually a medium to late-term complication [3, 4]. In these cases, it is thought to be secondary to wear at the liner/head interface decreasing the retaining power of the PE liner and resulting in dislocation of the prosthetic head/PE liner [4]. There are only a few reports of early intraprosthetic dislocations in the literature. In these series, the incidence of such an event ranges from 2% to 4% [5]. Banka et al. reported one case of an early dislocation in a 70-year-old woman who underwent revision with a DM cup after having recurrent dislocations. She suffered a dislocation of her DM cup, and radiographs showed the eccentric placement of the femoral head within the cup. She ultimately underwent repeat revision surgery for implantation of a constrained liner [3]. Samona et al. reported dislocation of a DM cup <1 year after implantation [6]. The patient required closed reduction and subsequently underwent revision surgery for persistent pain and clicking symptoms. The PE liner was found to be fragmented intraoperatively. Guyen et al. reported two dislocations out of 54 patients with DM cups at a minimum follow-up of 2.2 years [7]. This case could very well represent one of the earliest cases of intraprosthetic dislocation in literature. Indications for the use of DM cups in the United States are evolving, but it is agreeable that they significantly decrease dislocation rates in patients at risk for increased dislocations. Tarasevicius et al. reported dislocation rates in patients who underwent THA for femoral neck fractures with conventional cups compared to DM cups [8]. Conventional cups saw dislocations in 14.3% of patients, compared to no dislocations in the DM cup group. Adam et al. reported three dislocations out of 214 patients who underwent THA with a DM cup after sustaining a displaced femoral neck fracture [9]. In patients who underwent THA after resection of a hip tumor, the use of a DM cup led to lower rates of dislocation than reported in the literature [4]. In patients with cerebral palsy and resulting spasticity who underwent THA for osteoarthritis, Sanders et al. reported a dislocation rate of 0% at a mean follow-up of 39 months, which was significantly lower than rates reported in the literature for similar patient populations [10, 11]. Our patient’s initial revision was with a DM construct with acetabular component positioning within the so-called “safe zone” of Lewinnek et al. with anteversion of 15° ± 10° and inclination of 40° ± 10° [12]. However, it is now being accepted that majority of THA dislocations occur within the Lewinnek safe zone, and the ideal cup position for some patients may lie outside the safe zone [13]. Thus, at the time of re-revision, the decision was made to increase her anteversion out of the “safe zone.” This decision was bolstered by the fact that her native cup was uncovered anteriorly on CT suggesting that her native acetabular anteversion might be more than what was in the acetabular component (Fig. 2a). Intra-operatively, this increase in anteversion was gotten by making sure the edge of the new cup was in line with the anterior wall (Fig. 3b). This increase in the anteversion did not cause any intraoperative impingement with a conventional head/liner construct before implanting a DM construct. In this patient, it is possible that her alcohol abuse history (and altered mental status) contributed to her dislocation, as this is a known risk factor for complications after THA. However, the manner with which the DM construct was used in this case constitutes an off-label use (Stryker DM with Smith and Nephew femoral head and Synergy stem), and it is theoretically possible that this could have contributed to the intra-prosthetic dislocation. As such, it is difficult to conclusively say that the patient’s dislocation of a DM construct was completely due to patient factors, surgical technique, or implant issues.
Conclusion
Intraprosthetic dislocation is a rare occurrence and unique complication to DM constructs. It very rarely occurs in the acute post-operative period to our knowledge; this case report represents one of the earliest reports of intraprosthetic dislocation in the literature. Care should be taken in reducing dislocated DM constructs so as not to cause intraprosthetic dislocations and post-reduction radiographs should be gotten and properly scrutinized for intraprosthetic dislocations. Open revisions can be managed with revisions to another DM construct or to a constrained liner construct to maximize stability.
Clinical Message
DM cups can be used to provide increased stability for patients undergoing THA, but intraprosthetic dislocation can occur secondary to failure of retentive PE liner, aseptic loosening, or after closed reduction of a dislocation. In the setting of a dislocated THA with a dual-mobility cup treated with closed reduction, surgeons should scrutinize post-reduction radiographs for signs of intraprosthetic dislocation and consider revision of components if acetabular cup position is the cause of dislocation.
References
1. Patel PD, Potts A, Froimson MI. The dislocating hip arthroplasty: Prevention and treatment. J Arthroplasty 2007;22 4 Suppl 1:86-90.1. Patel PD, Potts A, Froimson MI. The dislocating hip arthroplasty: Prevention and treatment. J Arthroplasty 2007;22 4 Suppl 1:86-90.
2. McArthur BA, Nam D, Cross MB, Westrich GH, Sculco TP. Dual-mobility acetabular components in total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2013;42(10):473-478.
3. Banka TR, Ast MP, Parks ML. Early intraprosthetic dislocation in a revision dual-mobility hip prosthesis. Orthopedics 2014;37(4):e395-e397.
4. Philippeau JM, Durand JM, Carret JP, Leclercq S, Waast D, Gouin F. Dual mobility design use in preventing total hip replacement dislocation following tumor resection. Orthop Traumatol Surg Res 2010;96(1):2-8.
5. Philippot R, Boyer B, Farizon F. Intraprosthetic dislocation: A specific complication of the dual-mobility system. Clin Orthop Relat Res 2013;471(3):965-970.
6. Samona J, Flanagan B, Walter N. Acute disassembly and dissociation of a dual-mobility next-generation prosthesis. Orthopedics 2016;39(5):e980-e983.
7. Guyen O, Pibarot V, Vaz G, Chevillotte C, Béjui-Hugues J. Use of a dual mobility socket to manage total hip arthroplasty instability. Clin Orthop Relat Res 2009;467(2):465-472.
8. Tarasevicius S, Busevicius M, Robertsson O, Wingstrand H. Dual mobility cup reduces dislocation rate after arthroplasty for femoral neck fracture. BMC Musculoskelet Disord 2010;11:175.
9. Adam P, Philippe R, Ehlinger M, Roche O, Bonnomet F, Molé D, et al. Dual mobility cups hip arthroplasty as a treatment for displaced fracture of the femoral neck in the elderly. A prospective, systematic, multicenter study with specific focus on postoperative dislocation. Orthop Traumatol Surg Res 2012;98(3):296-300.
10. Sanders RJ, Swierstra BA, Goosen JH. The use of a dual-mobility concept in total hip arthroplasty patients with spastic disorders: No dislocations in a series of ten cases at midterm follow-up. Arch Orthop Trauma Surg 2013;133(7):1011-1016.
11. De Martino I, Triantafyllopoulos GK, Sculco PK, Sculco TP. Dual mobility cups in total hip arthroplasty. World J Orthop 2014;5(3):180-187.
12. Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 1978;60(2):217-220.
13. Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What safe zone? The vast majority of dislocated THAs are within the lewinnek safe zone for acetabular component position. Clin Orthop Relat Res 2016;474(2):386-391.
 |
 |
| Dr. Vineet Tyagi | Dr. Oluwaseun Akinbo |
| How to Cite This Article: Tyagi V, Akinbo O. Early Intraprosthetic Dislocation of a Dual Mobility Acetabular Construct after Total Hip Arthroplasty. Journal of Orthopaedic Case Reports 2017 Mar-Apr;7(2):21-24 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com