[box type=”bio”] What to Learn from this Article?[/box]
Synovial chondromatosis of hip, although rare, should be considered as a differential diagnosis in a child less than 10 years.
Case Report | Volume 7 | Issue 2 | JOCR March – April 2017 | Page 37-39| Manesh Chacko Philip, Sajeer Usman. DOI: 10.13107/jocr.2250-0685.740
Authors: Manesh Chacko Philip[1], Sajeer Usman[1]
[1] Department of Orthopaedics, Jubilee Mission Medical College Hospital, Thrissur, Kerala, India.
Address of Correspondence
Dr. Sajeer Usman,
Department of Orthopaedics, Jubilee Mission Medical College Hospital, Thrissur – 680 005, Kerala, India. Phone: +91-9539060696.
E-mail: drsajeerusman@gmail.com
Abstract
Introduction: Primary synovial chondromatosis (SC) is a disease of the synovium occurring in the third to fifth decade of life with the peak incidence in the fifth decade and commonly involves the knee in 50% cases. The diagnosis of SC is primarily radiological and intraoperative. Primary SC of the hip is rare, and their prevalence is not known.
Case Report: A 7-year-old female child presented with pain and limp left hip for 6 weeks. She had a stiff hip gait. Clinical examination revealed a fixed abduction, flexion deformity, and restricted internal rotation with apparent lengthening of 2 cm. The ultrasonography revealed synovial effusion with synovial deposits. Magnetic resonance imaging revealed features of tuberculous synovitis, inflammatory synovitis, or a rare possibility of SC. Arthrotomy was performed following failed hip aspiration. Multiple chondral loose bodies were noted on incision of capsule. Partial synovectomy was also performed. The synovium histopathology revealed multiple synovial chondral inclusions. A final diagnosis of SC was made.
Conclusion: We report this case of primary SC, 7-year-old female patient with symptoms of hip pain, limp, and fixed deformities restricting hip function as a first of its kind in the mentioned age group. Hence, although rare SC may be considered as one of the differential diagnosis in hip symptoms in children <10 years of age.
Keywords: Synovial chondromatosis, synovial chondromatosis in a child, synovial chondromatosis of hip.
Introduction
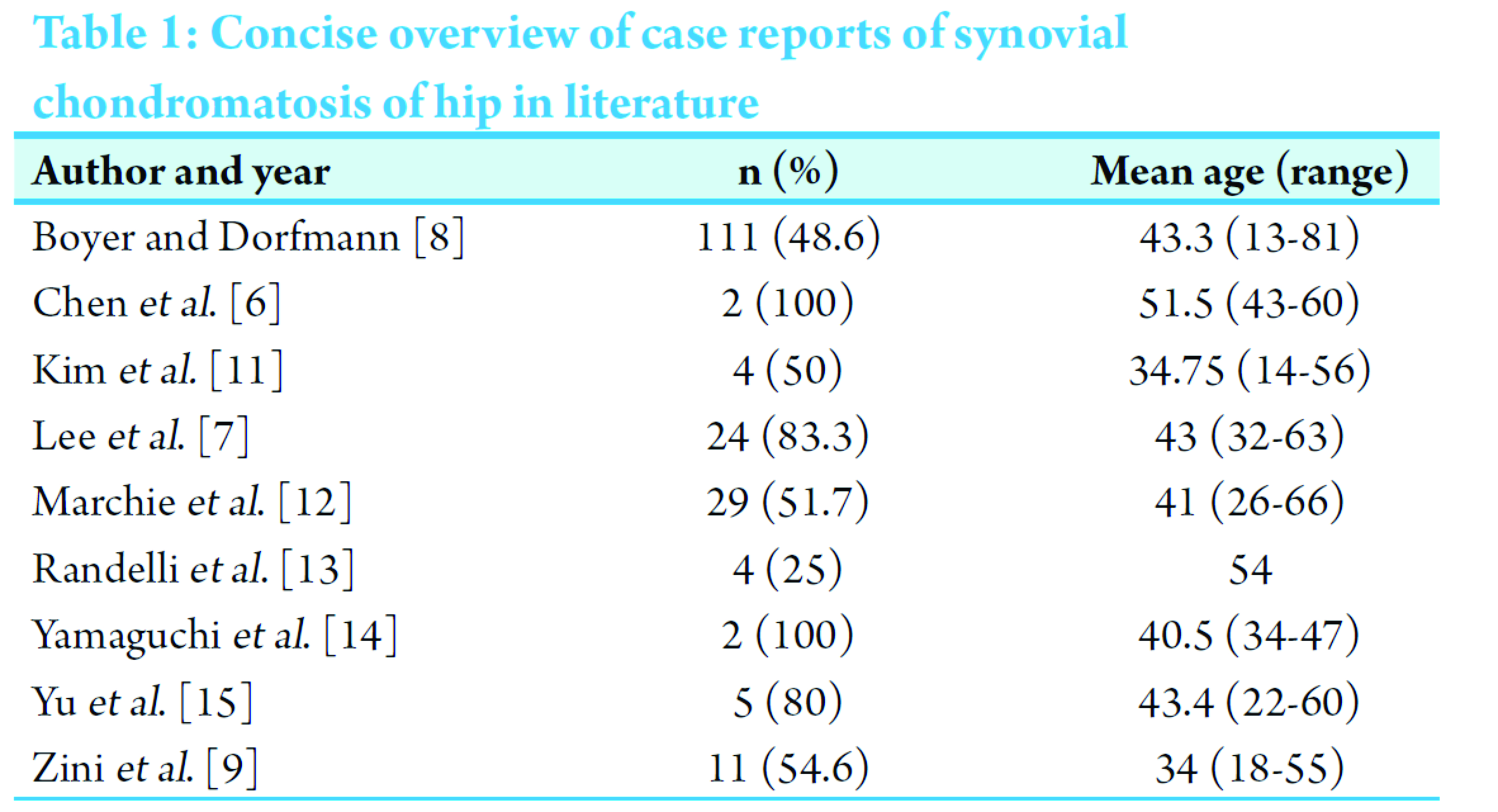
Primary synovial chondromatosis (SC) or osteochondromatosis is also known as Reichels syndrome first described in 1900 as a disease of the synovium occurring in the third to fifth decade of life with the peak incidence in the fifth decade and commonly involving the knee in 50% of cases. The diagnosis of SC is primarily radiological and intraoperative [1]. The accepted pathogenesis of the submesothelial foci of cartilaginous bodies is that they are formed by metaplasia of pleuripotential cells in the synovial membrane. These nodules can ossify and attach to the synovium by a vascular pedicle. They may break free and become loose bodies, and when nourished by synovial fluid, they can continue to proliferate [2]. Primary SC of the hip is rare, and their prevalence is not known. In a case series of 105 cases, only 5 cases involved the hip. They reported that 2 of 53 cases of SC were in the hips [3]. In a recent review of relevant articles, addressing SC of the hip across all available dates up to and including February 16, 2014. They found a total of 197 patients whose age ranged from 13 to 81 years [4]. To the best of our knowledge, there are no reports of SC of hip reported in children <12 [5] (Table 1).
Case Report
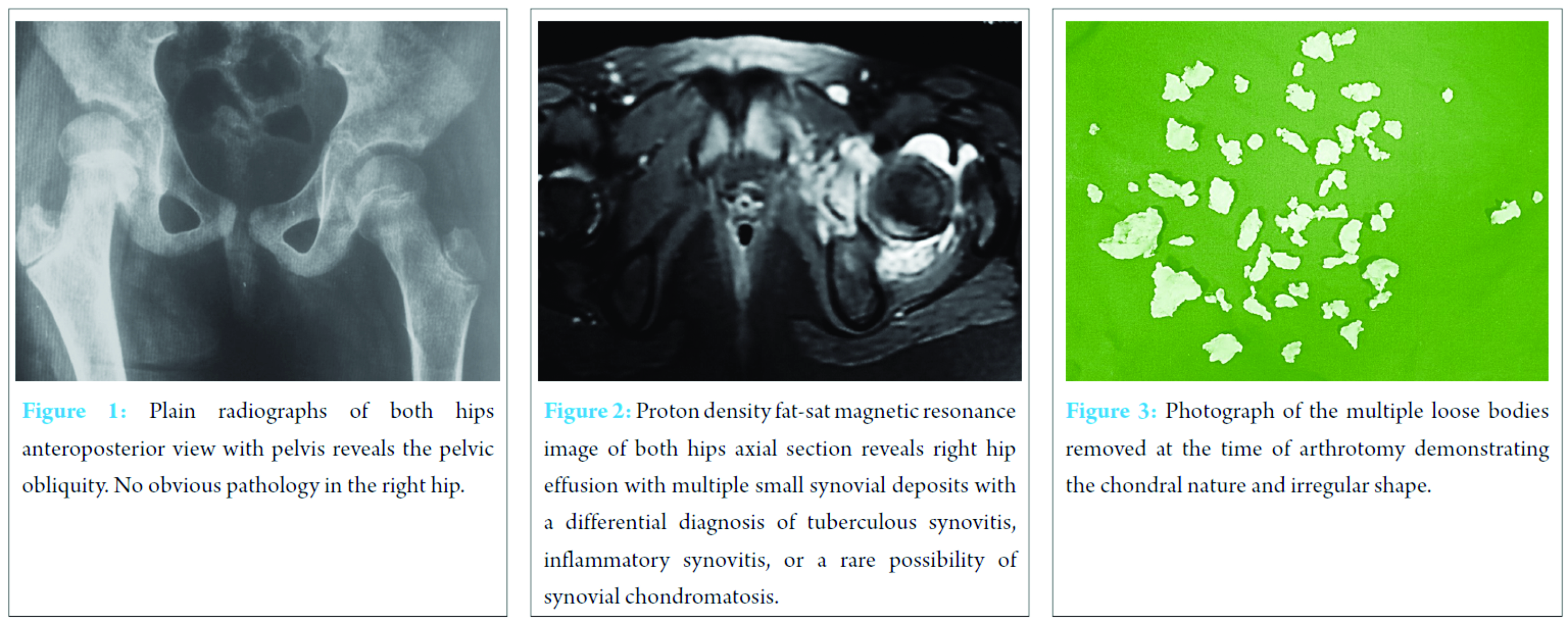
A 7-year-old female child presented to our outpatient department with pain and limp left hip for 6 weeks. She had a stiff hip gait. Clinical examination revealed a fixed abduction, flexion deformity, and restricted internal rotation with apparent lengthening of 2 cm. Plain radiographs revealed no abnormality except for pelvic obliquity (Fig. 1). Blood investigation did not reveal an inflammatory or infective cause including granulomatous infection. The child was put on traction suspecting transient synovitis before presentation. The ultrasonography revealed synovial effusion with synovial deposits. Magnetic resonance imaging revealed an effusion in the hip with synovial deposits with a differential diagnosis of tuberculous synovitis, inflammatory synovitis, or a rare possibility of SC (Fig. 2). On hospital admission for evaluation, the child was noted to have evening fever spikes. With the differential diagnosis of stage 1 tuberculosis hip or subacute infection, a decision was taken to perform a hip aspiration followed by arthrotomy if necessary in view of the severe and persistent clinical symptoms. The patient was placed in supine position. Hip aspiration failed to aspirate adequate fluid and decision was made to perform an arthrotomy through an anterolateral approach. On incision of the capsule, multiple chondral loose bodies were found and removed (Fig. 3). A partial synovectomy was done, and the wound closed in layers over a negative suction drain.
The synovial fluid analysis was inconclusive and failed to isolate any organism. The synovium histopathology revealed multiple synovial chondral inclusions. The loose bodies where found to be chondral and a final diagnosis of SC were made. The post-operative period was uneventful with child being allowed partial to full weight bearing in 2 weeks. The gait improved and she was walking normally after 6 weeks.
At the end of 1-year follow-up, there was no recurrence and clinical examination revealed a normal gait with no fixed deformities.
Discussion
Clinical symptoms in SC of hip are non-specific, and a clinical diagnosis is difficult to arrive at. Pain, stiffness, limited motion, clicking, locking, or limping may be present. If left untreated or not recognized, late complications such as secondary degenerative osteoarthritis, capsular contraction, subluxation, or pathologic femoral neck fracture may follow [6]. This case of SC has its relevance because of the age at presentation, especially in a female and the location of involvement, as SC is commonly seen in males in the third to fifth decade of life with involvement of the knee being the most common [7]. Management of such cases is based on the symptoms which may be recurrent monoarticular synovitis, swelling, pain, or mechanical symptoms [8]. Cartilaginous nodules which arise from the synovium are classical in SC which passes through three stages: Stage 1 – Active intrasynovial disease where the disease is limited to the synovial membrane by formation of chondral synovial inclusions. Stage 2 – Synovitis with synovial inclusions and chondral loose bodies in the joint. Stage 3 – Multiple loose bodies in the joint but synovium is quiescent [2]. Controversy exists regarding the treatment of SC. Theoretically, the best chance to reduce recurrence is intervention in Stage 3, but pressure erosions are seen in the later stages when the osteochondral loose bodies are fully formed, a delay in surgical intervention is not advisable. Because of its diffuse involvement, removal of entire synovium ensures the least chance of recurrence in Stage 1 or Stage 2. Removal of the loose bodies results in reduction of mechanical symptoms. Removal of the entire synovium is almost always not possible. The only other way is performing a loose body removal and almost total synovectomy in the presence of symptoms [9]. Arthroscopic removal of loose bodies has been reported as an effective method to remove the loose bodies. It offers excellent visualization of both central and peripheral compartments and allows tissue biopsy and subtotal synovectomy. Despite remarkable improvements in arthroscopic techniques to access the central and peripheral compartments, certain technical limitations exist including the inability to distract the hip, restriction of access to the posteromedial and posterolateral portion of the peripheral compartment and is more reliable when the size of the loose body is <10 mm [10]. For SC of the hip, arthroscopic removal of osteochondral fragments with synovectomy is both safe and effective, with a mean recurrence rate of 7.1% [4].
Conclusion
We report this case of primary SC, 7-year-old female patient with symptoms of hip pain, limp, and fixed deformities restricting hip function as a first of its kind in the mentioned age group. Hence, although rare SC may be considered as one of the differential diagnosis in hip symptoms in children <10 years of age.
Clinical Message
Clinical symptoms in SC of hip are non-specific, and a clinical diagnosis is difficult to arrive at. The incidence of the same is not reported in a female child in the age group below 10. SC although rare should be included as one of the differential in a child presenting with an acute hip pathology. The diagnosis and management of the same may be complicated by the overlapping symptoms with other differentials in the mentioned age group.
References
1. Knoeller SM. Synovial osteochondromatosis of the hip joint. Etiology, diagnostic investigation and therapy. Acta Orthop Belg 2001;67(3):201-210.
2. Hardacker J, Mindell ER. Synovial chondromatosis with secondary subluxation of the hip. A case report. J Bone Joint Surg Am 1991;73(9):1405-1407.
3. Mussey RD Jr, Henderson MS. Osteochondromatosis. J Bone Joint Surg Am 1949;31A(3):619-627.
4. de Sa D, Horner NS, MacDonald A, Simunovic N, Ghert MA, Philippon MJ, et al. Arthroscopic surgery for synovial chondromatosis of the hip: a systematic review of rates and predisposing factors for recurrence. Arthroscopy 2014;30(11):1499-1504.
5. Raza A, Kailash K, Malviya A. Rare cause of hip pain in a young girl. BMJ Case Rep 2014;2014. Pii. Bcr2014203802.
6. Chen CY, Chen AC, Chang YH, Fu TS, Lee MS. Synovial chondromatosis of the hip: management with arthroscope-assisted synovectomy and removal of loose bodies: report of two cases. Chang Gung Med J 2003;26(3):208-214.
7. Lee JB, Kang C, Lee CH, Kim PS, Hwang DS. Arthroscopic treatment of synovial chondromatosis of the hip. Am J Sports Med 2012;40(6):1412-1418.
8. Boyer T, Dorfmann H. Arthroscopy in primary synovial chondromatosis of the hip: description and outcome of treatment. J Bone Joint Surg Br 2008;90(3):314-318.
9. Zini R, Longo UG, de Benedetto M, Loppini M, Carraro A, Maffulli N, et al. Arthroscopic management of primary synovial chondromatosis of the hip. Arthroscopy 2013;29(3):420-426.
10. Rath E, Amar E, Doron R, Matsuda DK. Hip Arthroscopy for synovial chondromatosis: Tips and tricks. Arthrosc Tech 2014;3(6):e709-e712.
11. Kim SJ, Choi NH, Kim HJ. Operative hip arthroscopy. Clin Orthop Relat Res 1998;353:156-165.
12. Marchie A, Panuncialman I, McCarthy JC. Efficacy of hip arthroscopy in the management of synovial chondromatosis. Am J Sports Med 2011;39 Suppl:126S-131S.
13. Randelli F, Randelli P, Banci L, Arrigoni P. Intra-articular loose body removal during hip arthroscopy. Orthopedics 2010;33(7):476.
14. Yamaguchi T, Naito M, Asayama I, Fujisawa M, Ishiko T, Kambe T, et al. Arthroscopic surgery for synovial chondromatosis of the hip: A report of two cases. J Orthop Traumatol 2003;4:90-91.
15. Yu YH, Chan YS, Lee MS, Shih HN. Open and arthroscopic surgical management of primary synovial chondromatosis of the hip. Chang Gung Med J 2010;34:101-108.
 |
 |
| Dr. Manesh Chacko Philip | Dr. Sajeer Usman |
| How to Cite This Article: Philip MC, Usman S. Synovial Chondromatosis: A Rare Differential Diagnosis of Hip Pain in a Child. Journal of Orthopaedic Case Reports 2017 Mar-Apr;7(2):37-39. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com