[box type=”bio”] What to Learn from this Article?[/box]
Synovial chondromatosis is a rare condition and complete removal of chondromatosis tissue is important to prevent local recurrence, especially for the extra-articular form.
Case Report | Volume 7 | Issue 2 | JOCR March – April 2017 | Page 62-65| Jonathan A Isbell, Andrew C Morris, Ibukunoluwa Araoye, Sameer Naranje, Ashish B Shah DOI: 10.13107/jocr.2250-0685.752
Authors: Jonathan A Isbell[1], Andrew C Morris[1], Ibukunoluwa Araoye[1], Sameer Naranje[1], Ashish B Shah[1]
[1]Department of Orthopaedic, Division of Orthopedic Surgery, University of Alabama at Birmingham, Birmingham, Alabama 35205, USA.
Address of Correspondence
Dr. Ashish B Shah,
Department of Orthopaedic, Division of Orthopedic Surgery, University of Alabama at Birmingham, Birmingham, Alabama 35205, USA.
E-mail: ashishshah@uabmc.edu
Abstract
Introduction: Synovial chondromatosis is a rare, benign monoarticular condition characterized by the metaplastic formation of cartilaginous nodules from the synovium of joints (intra-articular), tendons and bursae (extra-articular). These nodules have the potential to detach and form loose bodies within the joint space. The most common locations are the large joints such as the knees, hips, elbows, and shoulders, with less common locations being the foot and ankle joints. Synovial chondromatosis primarily occurs in men between the third and fifth decades of life, and it typically presents as chronic joint pain with swelling, decreased joint range of motion, and osteoarthritis. Treatment is usually centered on excision and retrieval of nodules and loose bodies. Prognosis is usually good with a low-moderate likelihood of recurrence.
Case Report: We report the very rare case of a 27-year-old male with recurrent intra- and extra-articular ankle synovial chondromatosis, who also reported symptoms consistent with tarsal tunnel syndrome. His initial presentation was left ankle pain which was managed by open surgical debridement. Two years after, he re-presented with continued pain and tingling along the plantar aspect of his foot. On his second presentation, a dual approach was taken with arthroscopic as well as open debridement. He reported resolution of his symptoms postoperatively as well as at 3 years of follow-up.
Conclusion: Simultaneous extra- and intra-articular chondromatosis of the ankle is very rare and can be difficult to treat. It is important to recognize this disease as a rare but plausible cause of tarsal tunnel syndrome. Treatment may be complicated with early or late recurrence despite complete excision, highlighting the need for intentional follow-up of all cases.
Keywords: Ankle arthritis, osteochondromatosis, Reichel syndrome, recurrent synovial chondromatosis, tarsal tunnel syndrome.
Introduction
Synovial chondromatosis is a rare, benign condition characterized by the formation of cartilaginous nodules within the synovium of joints. It is usually monoarticular and occurs most commonly in larger joints, with over 50% of cases occurring in the knee [1]. These cartilaginous changes represent metaplastic changes of the synovium itself, and increased levels of chondrocalcin have been reported in the synovial fluid of synovial chondromatosis patients [2]. Other commonly affected joints include the hip, elbow, and shoulder. Smaller joints such as the ankle joint and metatarsophalangeal joints are less commonly affected [2, 3, 4, 5]. Synovial chondromatosis has a male predilection (2:1 male to female ratio) and typically occurs in the third to fifth decade of life [2, 6, 7]. The primary treatment strategy is surgery with either open debridement or arthroscopic debridement with partial or total synovectomy. Currently, the arthroscopic approach is favored for intra-articular cases because it leads to less joint stiffness, possibly because of earlier return to mobility of the joint. On the other hand, the open surgical approach is more favorable for extra-articular cases given the smaller working space involved in extra-articular areas [8]. With either the open or arthroscopic approach, there remains a possibility of recurrence needing further surgery [9]. Such cases present a management challenge and usually benefit from a dual approach (open plus arthroscopic debridement).
Although most cases of synovial chondromatosis are intra-articular – arising from the joint synovium – synovial chondromatosis rarely also arises in extra-articular structures such as tendon sheaths and bursae [8]. Such extra-articular involvement has been reported in the hand [10, 11] as well as the foot and ankle joints [3, 4, 12, 13]. While extra-articular involvement is rare in and of itself, combined extra-synovial and intra-synovial chondromatosis represents an even rarer entity with few reports of such occurrences in the foot and ankle [14, 15]. We report the case of a 27-year-old male patient with recurrent ankle intra- and extra-synovial chondromatosis who was treated successfully using both arthroscopic and open debridement (dual approach).
Case Report
A 27-year-old male presented for evaluation of a recurrence of progressively worsening left ankle pain and swelling. Four years prior, he underwent orthopedic evaluation for a painful mass in the same ankle. On that account, he eventually underwent open biopsy and synovectomy of the left ankle as well as resection of an extra-articular left ankle mass in 2011. Multiple osteochondral bodies were found and removed intraoperatively and sent for histopathologic examination. Synovial chondromatosis was diagnosed following histopathology.
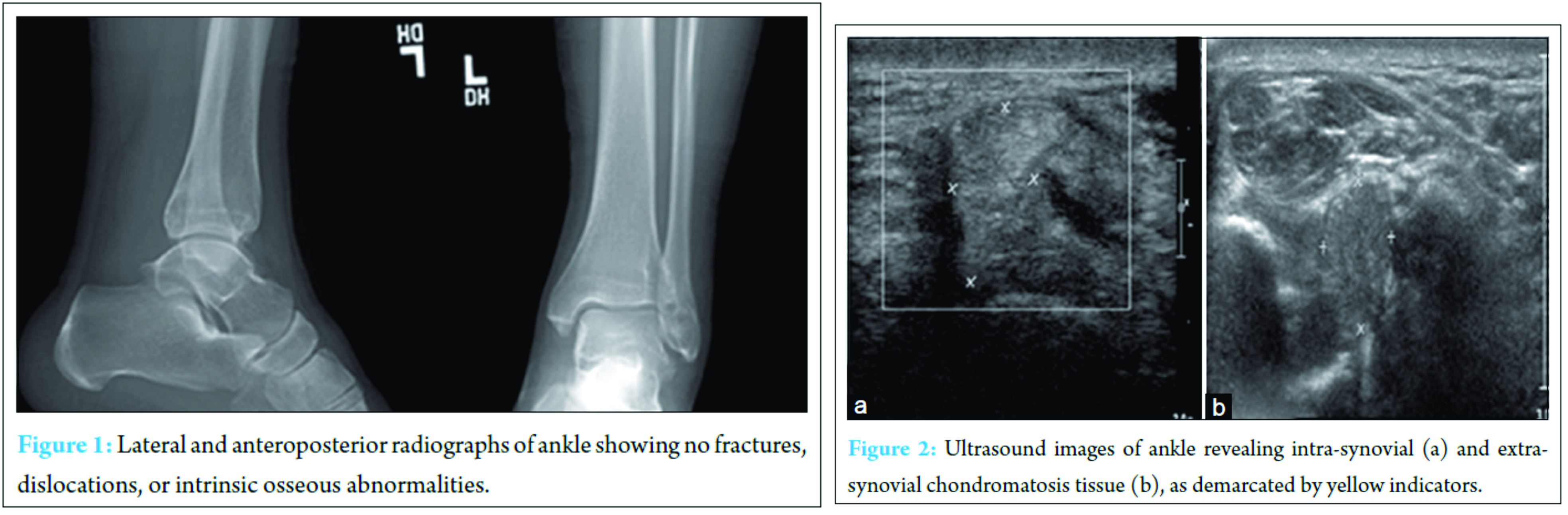
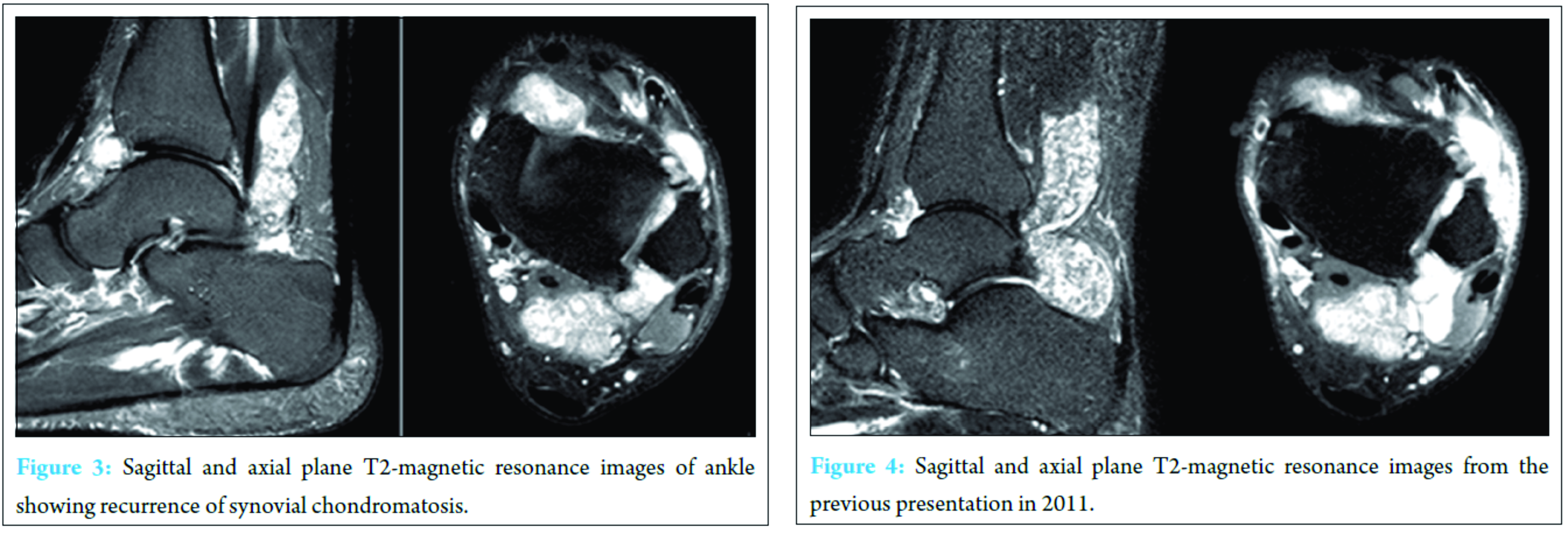
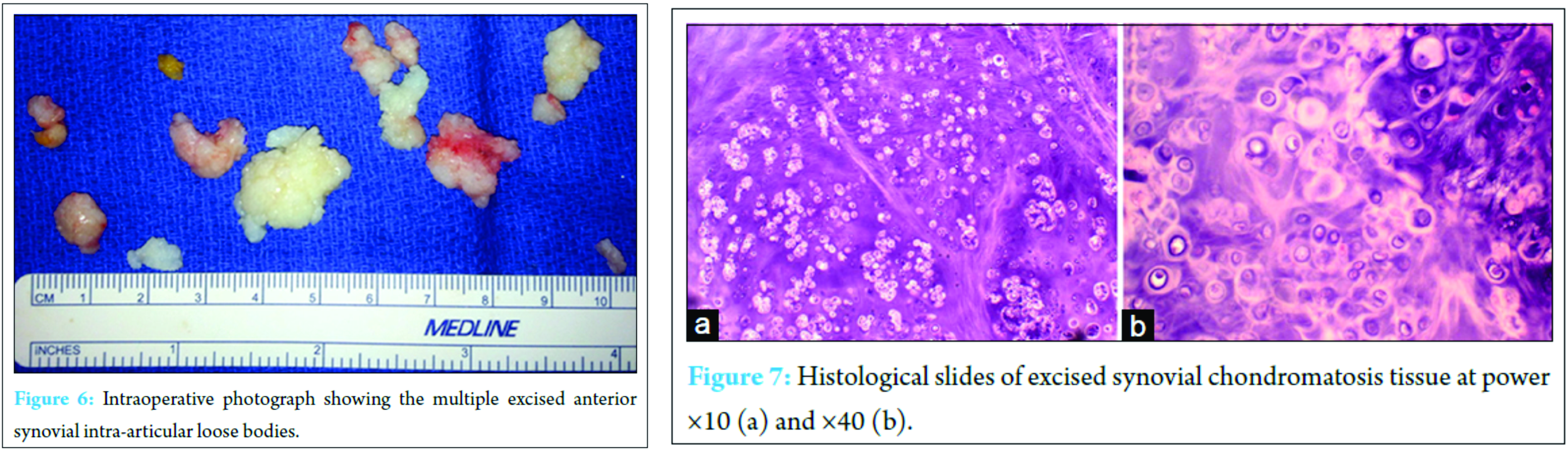
Two years after that first operative intervention, the patient returned with left ankle pain and swelling aggravated by shoe-wearing, weight bearing, and climbing stairs. He also reported symptoms consistent with tarsal tunnel syndrome in the same foot – tingling and burning along the plantar aspect of his foot. Physical examination at this time demonstrated palpable fullness of the ankle joint with minimal restriction in range of motion as well as exquisite tenderness to palpation anterolaterally. A palpable mass was noted along the anterolateral aspect of the ankle. His motor and sensory exams were within normal limits and range of motion of the ankle, and subtalar joints were within normal limits. Radiographs obtained demonstrated opacity overlying the pre-Achilles fat pad and adjacent soft tissues of the posterior ankle (Fig. 1). There was moderate erosion of the anterolateral aspect of the distal tibia. No fractures, dislocations, or intrinsic osseous abnormalities were noted. Ultrasound of the left ankle revealed distention of the joint capsule anteriorly and posteriorly at the tibiotalar joint with intra-articular debris as well as hyperemia of the synovium (Fig. 2). The anterolateral gutter also had intra-articular debris and was distended. Magnetic resonance imagining (MRI) demonstrated numerous large, lobulated, heterogeneously enhancing lesions posteriorly surrounding the flexor hallucis longus (FHL) tendon, and extending into the anterior tibiotalar joint (Fig. 3). There was minimal involvement of the sinus tarsi; however, cranial extension between the distal tibiofibular syndesmosis was noted along with stable erosion of the anterolateral aspect of the distal tibia. The tendons and ligaments of the left ankle were intact, and the articular cartilage was unremarkable. No soft tissue swelling, edema, or bony involvement was identified. These findings were consistent with the MRI findings from his primary presentation 2 years ago (Fig. 4). Extensive ankle joint T2-signal abnormality was consistent with recurrence of synovial chondromatosis. Following this rediagnosis, the patient was scheduled for ankle arthroscopy with joint decompression and synovial debridement.
The patient was prepped and draped in the usual sterile fashion. Portals were established into the ankle joint anteromedially and anterolaterally with transillumination positioned lateral to the branch of the superficial peroneal nerve. On entry into the joint space, a considerable amount of scar tissue formation and tissue inflammation was appreciated. A thorough debridement was performed using a 2.7 mm scope and a 3.5 mm protected aggressive shaver. All chondromatosis tissue was visualized Fig. 5a and b; however, to remove all of the intra-articular loose bodies and debris, the anterolateral portal incision was extended by 0.5 cm and the tissue was removed in a piecemeal fashion through the portal. Close attention was paid to avoid leaving any soft tissue debris in the intra-articular space or surrounding soft tissue. Attention was then focused on the posterior aspect of the ankle joint. A separate incision was made along the posterolateral aspect of the ankle joint in the interval between the peroneal tendons laterally and the FHL medially (Fig. 5c).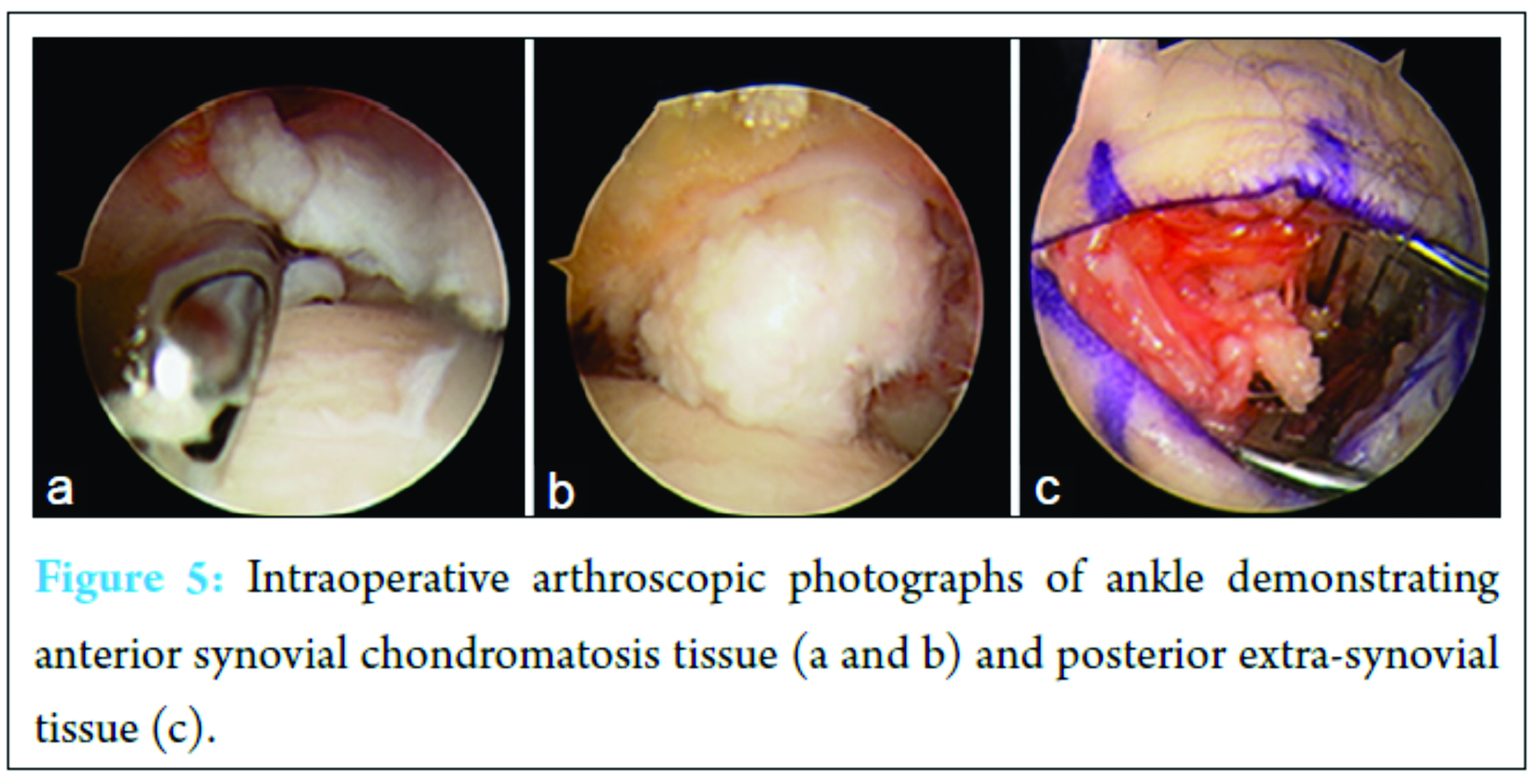
Discussion
Synovial chondromatosis represents chondral metaplasia of the synovium of a joint. Normal synovial tissue lacks chondrocytes and thus the ability to form cartilage. Metaplasia of the synovium confers this cartilage-forming potential leading to cartilage formation [16]. These metaplastic lesions can become pedunculated and eventually break free from the synovial tissue forming loose bodies. These loose bodies are nourished through diffusion of nutrients from the synovial fluid and can occasionally become calcified and even ossified [8]. Thus, in the early stages of the disease, these loose bodies may be radiolucent on radiographs before undergoing calcification, which is a late feature or may not be present [8]. Synovial chondromatosis typically presents with symptoms of clicking, decreased range of motion, and mild joint pain that worsens with activity.
Intra-articular synovial chondromatosis is uncommon in the foot and ankle [8, 10, 16]. However, cases have been reported describing a wide range of presenting symptoms ranging from an asymptomatic incidental finding to chronic ankle instability [17, 18]. In addition to the rarity of synovial chondromatosis in the foot and ankle, recurrence of synovial chondromatosis is also relatively rare. In our case, he presented with recurrence of symptoms 2 years after open resection of the primary occurrence/diagnosis of synovial chondromatosis of the ankle. He also demonstrated symptoms consistent with tarsal tunnel syndrome. Making this case even more interesting is the fact that our patient presented with a combination of intra- and extra-synovial chondromatosis, a very rare co-occurrence. Oakley et al. [19] reported the case of a 29-year-old male with extra-synovial involvement of the FHL tendon who presented with progressive ankle discomfort and a normal physical examination. Similar to our patient, this patient was successfully treated with open debridement of the posterior aspect of the ankle.
While synovial chondromatosis has practically no potential for metastasis, failure to treat this condition in a timely manner carries risk of complications such as osteoarthritis as well as a minimal risk for malignant transformation to chondrosarcoma [7]. In addition, this condition warrants close observation even after resection owing to the risk of recurrence, especially for extra-synovial chondromatosis [16]. This risk of recurrence also warrants optimal effort for complete resection of all pathologic tissue. With open resection and synovectomy for intra-articular disease, it can be difficult to visualize all loose bodies inside the joints, and as a consequence, remnant loose bodies are likely to continue to grow. However, with an arthroscopic approach, it is easier to visualize and extract intra-articular loose bodies, minimizing the risk for recurrence of symptoms. Furthermore, arthroscopic debridement was found to have a shorter recovery time compared to traditional arthrotomy owing to the reduced joint immobilization time [13]. In our case, the patient was effectively managed arthroscopically for recurrent intra-articular synovial chondromatosis and with open excision for extra-articular disease.
Conclusion
Synovial chondromatosis of the ankle is rare. This case report demonstrates the importance of understanding the wide range of presenting symptoms as well as the need for adequate excision and extraction of all nodules due to the non-negligible recurrence rate of synovial chondromatosis.
Clinical Message
Synovial chondromatosis is a rare condition. It can present intra‑articularly or extra-articularly. The intra-articular form is the most common in the knees, hip, elbow, and shoulder joints. The extra-articular form is the most common in the hands and feet. Complete removal of chondromatosis tissue is important to prevent local recurrence, especially for the extra-articular form.
References
1. Bloom R, Pattinson JN. Osteochondromatosis of the hip joint. J Bone Joint Surg Br 1951;33-B(1):80-84.
2. Bynum CK, Tasto J. Arthroscopic treatment of synovial disorders in the shoulder, elbow, and ankle. J Knee Surg 2002;15(1):57-59.
3. Gulati A, Williamson DM. Synovial chondromatosis: A rare cause of a dislocated metatarso-phalangeal joint. Foot Ankle Surg 2010;16(2):e21-e23.
4. Ozmeric A, Aydogan NH, Kocadal O, Kara T, Pepe M, Gozel S. Arthroscopic treatment of synovial chondromatosis in the ankle joint. Int J Surg Case Rep 2014;5(12):1010-1013.
5. Ryan JD, Garwood C, Lickiss J. Synovial chondromatosis surrounding the first metatarsophalangeal joint: A case report. Foot Ankle Spec 2016;9(2):174-178.
6. Fuerst M, Zustin J, Lohmann C, Rüther W. Synovial chondromatosis. Orthopade 2009;38(6):511-519.
7. Yao MS, Chang CM, Chen CL, Chan WP. Synovial chondrosarcoma arising from synovial chondromatosis of the knee. JBR-BTR 2012;95(6):360-362.
8. Kirchhoff C, Buhmann S, Braunstein V, Weiler V, Mutschler W, Biberthaler P. Synovial chondromatosis of the long biceps tendon sheath in a child: A case report and review of the literature. J Shoulder Elbow Surg 2008;17(3):e6-e10.
9. Craft RO, Smith AA, Duncan SF. Recurrent synovial chondromatosis of the distal interphalangeal joint: Case report. J Hand Surg Am 2009;34(2):301-303.
10. Cebesoy O, Isik M, Subasi M, Karsli B, Pamukcu U. Extra-articular tenosynovial chondromatosis mimicking a neoplastic disease in the first web space of the hand. Oman Med J 2012;27(4):316-318.
11. Gil-Albarova J, Morales-Andaluz J, Castiella T, Seral F. Tenosynovial chondromatosis of the third finger. Arch Orthop Trauma Surg 2000;120(3-4):239-240.
12. Chen A, Shih SL, Chen BF, Sheu CY. Primary synovial osteochondromatosis of the first metatarsophalangeal joint. Skeletal Radiol 2002;31(2):122-124.
13. Doral MN, Uzumcugil A, Bozkurt M, Atay OA, Cil A, Leblebicioglu G, et al. Arthroscopic treatment of synovial chondromatosis of the ankle. J Foot Ankle Surg 2007;46(3):192-195.
14. Pathak S, Joseph C, Aravinda M, Sonar S, Vinodh K, Rajan D. A case of primary intra-articular and extra articular synovial chondromatosis of ankle and foot. Internet J Orthop Surg 2006;4(1):1-6.
15. Van P, Wilusz PM, Ungar DS, Pupp GR. Synovial chondromatosis of the subtalar joint and tenosynovial chondromatosis of the posterior ankle. J Am Podiatr Med Assoc 2006;96(1):59-62.
16. Fetsch JF, Vinh TN, Remotti F, Walker EA, Murphey MD, Sweet DE. Tenosynovial (extraarticular) chondromatosis. Analysis of 37 cases of an underrecognized clinicopathologic entity with a strong predilection for the hands and feet and a high local recurrence rate. Am J Surg Pathol 2003;27(9):1260-1268.
17. Brodsky JW, Jung KS, Tenenbaum S. Primary synovial chondromatosis of the subtalar joint presenting as ankle instability. Foot Ankle Int 2013;34(10):1447-1450.
18. Scholl DM, Taddie KL. Asymptomatic synovial chondromatosis of the ankle: An incidental finding. J Foot Ankle Surg 2010;49(6):565.e13-e17.
19. Oakley J, Yewlett A, Makwana N. Tenosynovial osteochondromatosis of the flexor hallucis longus tendon. Foot Ankle Surg 2010;16(3):148-150.
 |
 |
 |
 |
|
| Dr. Jonathan A Isbell | Dr. Andrew C Morris | Dr. Ibukunoluwa Araoye | Dr. Sameer Naranje | Dr. Ashish B Shah |
| How to Cite This Article: Jonathan A Isbell, Andrew C Morris, Ibukunoluwa Araoye, Sameer Naranje, Ashish B Shah Recurrent Extra- and Intra-articular Synovial Chondromatosis of the Ankle with Tarsal Tunnel Syndrome: A Rare Case Report. Journal of Orthopaedic Case Reports 2017 Mar-Apr;7(2):62-65. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com