[box type=”bio”] What to Learn from this Article?[/box]
A test of integrity of all arthroscopic instruments used during operation, at least at the end of very operation, is essential.
Case Report | Volume 7 | Issue 2 | JOCR March – April 2017 | Page 78-81| Uli Schmiddem, N Hawi, E M Suero, R Meller. DOI: 10.13107/jocr.2250-0685.760
Authors: Uli Schmiddem[1], N Hawi[1], E M Suero[1], R Meller[1]
[1] Trauma Department, Medical School Hannover, Germany.
Address of Correspondence:
Dr. Uli Schmiddem,
Department of Orthopaedic Trauma,
Medical School Hannover, Carl-Neuberg-Street 1, 30625 Hannover, Germany.
E-mail: ulischmiddem@yahoo.de
Abstract
Introduction: We report a case of a lost metal platelet from a radiofrequency ablation probe (VAPR VUE Radiofrequency System, Cool Pulse 90, DePuy, Synthes, Switzerland) in the shoulder joint during elective arthroscopic cuff repair. To the best of our knowledge, this kind of an incident during elective arthroscopy has not been described in the literature so far. In addition, we present an algorithm on how to deal with such an incident.
Case Report: A 69-year-old woman underwent an arthroscopic subacromial decompression and rotator cuff repair for a torn supraspinatus tendon. While performing the subacromial decompression and after swapping the portals from lateral to posterior, the metal platelet of the electrocautery device got detached from the instrument and lost in the operation field. Several attempts to visualize the lost platelet with the camera failed. Finally, intraoperative fluoroscopic imaging was used to detect the platelet. To confirm the definitive whereabouts of the platelet, two spinal needles were positioned perpendicular to another under x-ray control, both pointing at the missing platelet. After determining the exact location, the platelet could finally be visualized with the camera and removed. Due to this incident, the operation time was extended extensively, and the patient as well as the theatre team was exposed to an unnecessary amount of radiation.
Conclusion: This report indicates that an extraordinary incident such as the detachment of a component of the arthroscopic equipment during surgery is possible and should be kept in mind by the surgeon. Therefore, we believe that it is essential to perform a test of integrity at least at the end of every operation. In addition, we are presenting an algorithm on how to deal with the situation of a lost foreign body during arthroscopy, which can be applied to any joint.
Keywords: Shoulder arthroscopy, complication, lost foreign body, radiofrequency ablation instrument.
Introduction
Arthroscopy has become the gold standard for examining the articular joint surfaces and intra-articular structures. Since it is minimal invasive, complications in general are rare compared to open surgery. Common complications include infection, intra-articular damage, vascular injury with secondary hemarthrosis, nerve injury, extra-articular extravasation of fluids in the surrounding soft tissues, and post-operative pain [1, 2, 3]. More uncommon complications include instrument breakage, dermal burns, and compartment syndrome [4, 5, 6, 7]. In addition, there is a well-known risk of thromboembolic incidents peri- and post-operatively [8]. Reports of intra-articular foreign bodies in the shoulder are rare. There are a few case reports, one reporting a bullet located in the intra-articular space after a gunshot wound [9]. To the best of our knowledge, there are no reports about lost components of surgical equipment in the shoulder joint during surgery. In this case report, we describe the complication of a detached component from the electrocautery unit of a radiofrequency ablation probe (VAPR VUE Radiofrequency System, Cool Pulse 90, DePuy, Synthes, Switzerland) during elective shoulder arthroscopy. Furthermore, we illustrate an algorithm on how to deal with this incident.
Case Report
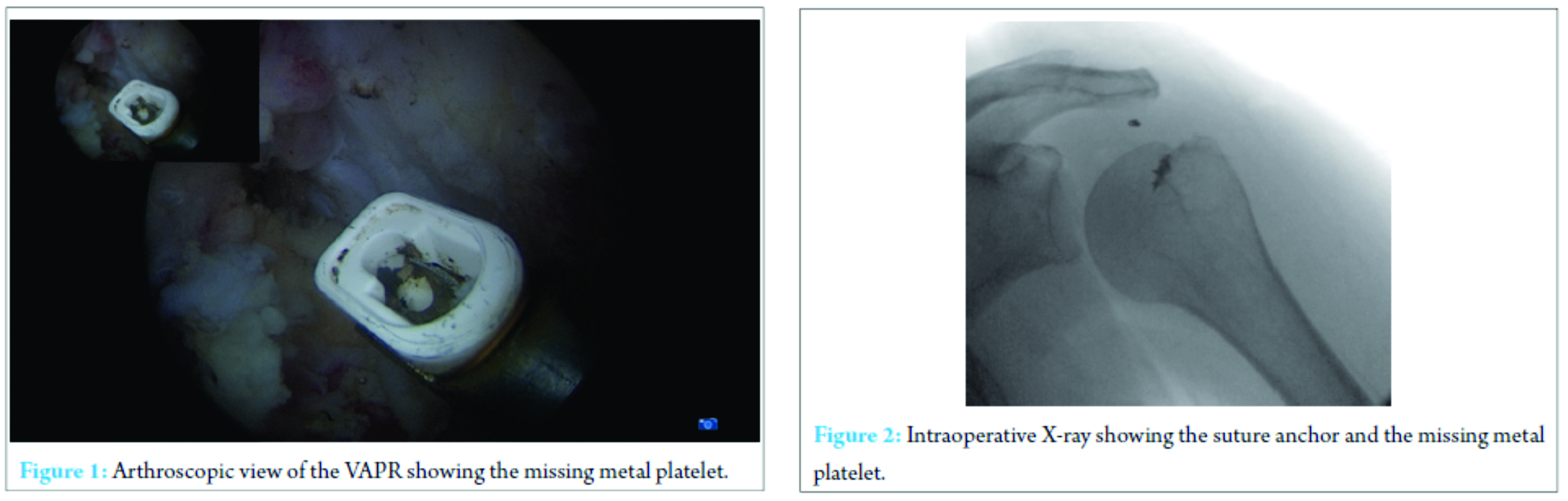
A 69-year-old woman, in good health overall, presented to our clinic with complaints of left shoulder pain. The clinical examination showed weakness and pain in response to the supraspinatus tendon, highly suspicious for a tear of the tendon. Positive impingement signs were documented. A magnetic resonance imaging scan revealed a full-thickness tear of the anterior fibers of the supraspinatus tendon. It was decided to perform an arthroscopic reconstruction of the supraspinatus tendon with suture anchors combined with a subacromial decompression. Pre-operative, a single-shot antibiotic therapy with cefazolin 2 g i.v. was provided in the induction room. Under general anesthesia and in beach chair position, a standard dorsal portal was established to perform the diagnostic arthroscopy. No arthroscopy cannulas were used. Subacromial bursectomy and moderate acromioplasty were performed through the anterolateral portal with the electrocautery device and the acromionizer. The full-thickness tear of the supraspinatus tendon (C-shaped, 2×1.5 cm) was verified. No other pathologies were found. A double-loaded anchor was introduced to the footprint of the supraspinatus tendon (Mitek Sports Medicine and Healix Peek Suture Anchor). Both strands were pulled through the tendon and acted as a medial row fixation in a planned double-row fixation technique. An adequate reducton of the tear could be a achieved. The radiofrequency ablation probe (VAPR VUE Radiofrequency System, Cool Pulse 90, DePuy, Synthes, Switzerland) was introduced through the lateral portal to debride the insertion point for the lateral row anchor. After swapping portals with the camera to finalise the debridement of the posterior aspect of the subacromial bursa of the posterior bursa, the metal platelet from the electrocautery unit of the radiofrequency ablation probe was found to be missing (Fig. 1).
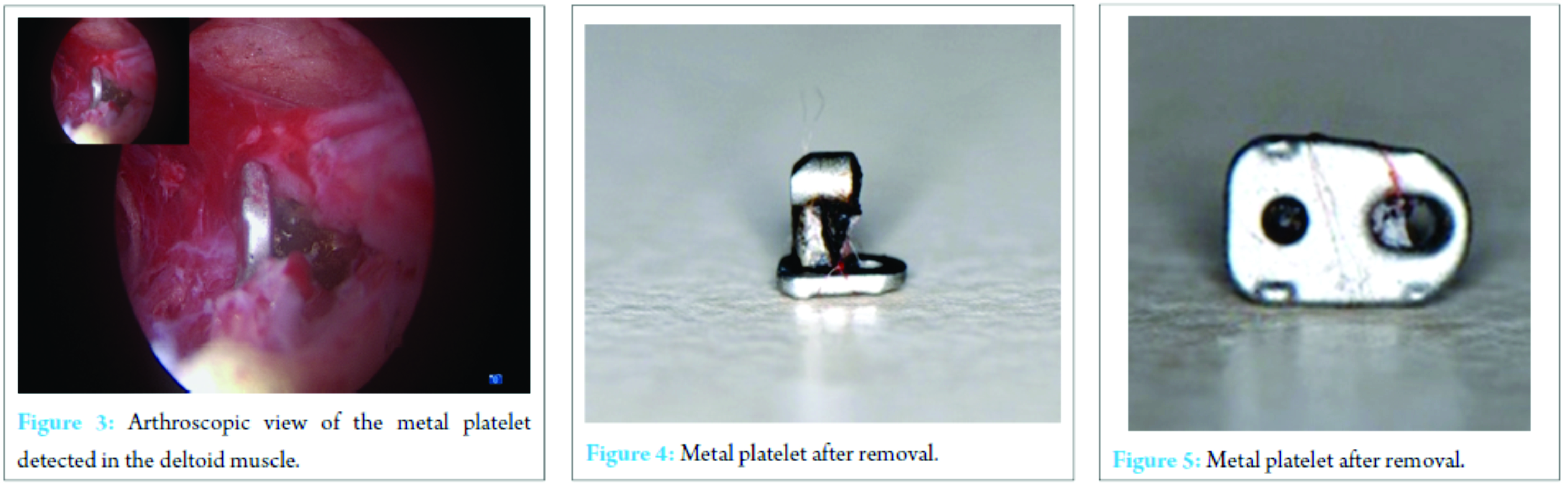
It could neither be visualized outside the operating field nor could it be detected inside the shoulder. After an extensive search inside and outside the joint failed, it was decided to use intraoperative fluoroscopic imaging to detect the platelet. As a result of this, the surgeons and the scrub nurse had to unscrub, put on leads und scrub again. The image intensifier visualized the platelet within the shoulder (Fig. 2). However, the precise whereabouts of the platelet were not known, since we could not determine whether the platelet was lost while removing the electrocautery device from the anterolateral portal or while reinserting it in the dorsal portal. A shoulder anterior-posterior glenoid view was taken. By the means of an 18-gauge needle, the location of the missing foreign body was marked. The needle was projected precisely onto the platelet in a line with the path of X-rays until the needle and the platelet presented themselves as one dot on the image intensifier screen. The needle was left in this position. Subsequent, a second radiograph was adjusted in a direction as perpendicular as possible to the first radiograph. The location of the foreign body was again marked in the same way using another 18-gauge needle. The intersection of the needles indicated the position of the missing platelet. The location appeared to be intramuscular, within the deltoid muscle in the course of the dorsal portal. This area was then arthoscopically explored in detail. The plate was finally visualized within the muscle fibers of the deltoid muscle and was removed under view with the grasping forceps (Fig. 3, 4, 5).
Once the removal of the plate was completed, we continued with the operation without any further complications. However, due to this incident, the operation time was extended extensively and the patient as well as the theatre team was exposed to an unnecessary amount of radiation. The patient stayed for 3 days in hospital before being discharged home. The post-operative rehabilitation was not altered by the reported complication.
Discussion
Arthroscopy has become a popular and safe diagnostic and therapeutic method to address various pathologies of the shoulder joint. Besides the well-known complications such as neurovascular injuries, infection, or iatrogenic cartilage damage [1, 10, 11, 12, 13], there are also rare complications such as instrument breakage, dermal burns, or compartment syndrome [4, 7, 8]. Failure of an arthroscopic instrument, with the result of a detached component lost in the operation field, is a very rare complication and has not been reported so far as to our knowledge. With this case report, we want to highlight that the detachment of a component of a surgical instrument during arthroscopy is possible. Therefore, we believe that it is essential to perform a test of integrity after pulling the arthroscopy instruments out of the portals. At least a test of integrity should be performed at the end of every operation. In case of a lost foreign body during arthroscopy, some authors recommend the following procedure. The inflow and outflow of water should be stopped immediately to prevent flushing the lost body in non-accessible areas of the joint [14]. If the foreign body can be visualized with the camera, it should be grasped using the largest available grasping forceps and then be removed. Particularly mentioned in the literature is the Kocher forceps and the pituitary rongeur [5]. Our algorithm in case of lost foreign bodies during arthroscopy is different than the previously described procedure. We believe that the inflow and outflow of water should be maintained as not to risk a loss of visualization. In our opinion, it is more important to maintain the best possible view the unlikely risk of flushing the foreign body to non-accessible areas of the joint. In shoulder arthroscopy, almost all areas are accessible. If neccessary, an additional portal has to be established. If the foreign body cannot be visualized using the camera, fluoroscopic imaging intensifying can be used to detect it if the foreign object is radiopaque. In our practice, we image the joint in two perpendicular projections and mark the position of the foreign body with needles. It is of importance that the needles are pointing straight in the line of the straight in line with the path of rays and pointing directly on the foreign object. When the direction of the image intensifier is adjusted correctly, the spinal needle and the foreign body should appear to be one overlapping spot on the screen. This way the intersection of the two needles marks the position of the foreign body. Previous case reports have described incidents of lost foreign bodies, which could not be removed despite all kind of efforts. For instance, Griffin and Villar described an unsuccessful attempt to remove the broken jaw of a forceps during a hip arthroscopy [15]. The jaw was eventually pushed into the actebular fossa and was left there without any negative effects for the patient. In some publications, it is recommended to push foreign bodies that cannot be removed into not weight bearing areas of the joint as an ultimate solution; an arthrotomy should not be performed. By performing an emergency arthrotomy, there is a great risk of causing more harm because of intra- and extra-articular damage compared to leaving the foreign body in place. Furthermore, operation time and anesthesia time are extended [5, 16]. However, the increased probability of osteoarthritis because of intra-articular foreign bodies must be taken seriously. Therefore, from our point of view, it should always be attempted by any means to detect and remove foreign bodies in arthroscopic shoulder procedures. We refrain from leaving them in the operating field.
Conclusion
This case report describes the incident of a lost component of a radiofrequency ablation probe in the shoulder joint during elective arthroscopic shoulder surgery. It also reports an algorithm on how to deal with the situation. To the best of our knowledge, it is the first description of the loss of a component of an electrocautery unit from a radiofrequency ablation device during elective shoulder arthroscopy. At least at the end of every operation, a test of integrity of all used arthroscopic devices should be conducted.
Clinical Message
Even if the complication of a lost component of an arthroscopic instrument during arthroscopy is a rare complication, the possibility of this incident should be kept in mind by the surgeon. Therefore, at least at the end of every operation, a test of integrity of all used arthroscopic devices should be conducted.
References
1. Moen TC, Rudolph GH, Caswell K, Espinoza C, Burkhead WZ Jr, Krishnan SG, et al. Complications of shoulder arthroscopy. J Am Acad Orthop Surg 2014;22(7):410-419.1. Moen TC, Rudolph GH, Caswell K, Espinoza C, Burkhead WZ Jr, Krishnan SG, et al. Complications of shoulder arthroscopy. J Am Acad Orthop Surg 2014;22(7):410-419.
2. Dick W, Glinz W, Henche HR, Ruckstuhl J, Wruhs O, Zollinger H. Complications of arthroscopy. A review of 3714 cases (author’s transl). Arch Orthop Trauma Surg 1978;92(1):69-73.
3. Case of injury of the arm: Requiring amputation at the shoulder joint. Prov Med Surg J (1840) 1841;2(28):28-30.
4. Milankov M, Savic D, Miljkovic N. Broken blade in the knee: A complication of arthroscopic meniscectomy. Arthroscopy 2002;18(1):E4.
5. Allum R. Complications of arthroscopy of the knee. J Bone Joint Surg Br 2002;84(7):937-945.
6. Curtin B, Friebe I. Dermal burn during hip arthroscopy. Orthopedics 2014;37(8):e746-e749.
7. Troxell CR, Morgan CD, Rajan S, Leitman EH, Bartolozzi AR. Dermal burns associated with bipolar radiofrequency ablation in the subacromial space. Arthroscopy 2011;27(1):142-144.
8. Greene JW, Deshmukh AJ, Cushner FD. Thromboembolic complications in arthroscopic surgery. Sports Med Arthrosc 2013;21(2):69-74.
9. Galland A, Lunebourg A, Airaudi S, Gravier R. A bullet in the supraspinatus compartment successfully removed by arthroscopy: Case report and review of the literature. Case Rep Orthop 2015;2015:3.
10. Ashraf A, Luo TD, Christophersen C, Hunter LR, Dahm DL, McIntosh AL, et al. Acute and subacute complications of pediatric and adolescent knee arthroscopy. Arthroscopy 2014;30(6):710-714.
11. Hagino T, Ochiai S, Watanabe Y. Complications after arthroscopic knee surgery. Arch Orthop Traumatol Surg 2014;134(11):1561-1564.
12. Salzler MJ, Lin A, Miller CD. Complications after arthroscopic knee surgery. Am J Sports Med 2014;42(2):292-296.
13. Noud PH, Esch J. Complications of arthroscopic shoulder surgery. Sports Med Arthrosc 2013;21(2):89-96.
14. Papavasiliou AV, Bardakos NV. Complications of arthroscopic surgery of the hip. Bone Joint Res 2012;1(7):131-144.
15. Griffin DR, Villar RN. Complications of arthroscopy of the hip. J Bone Joint Surg Br 1999;81(4):604-606.
16. Grand JG, Roig JA, de Swarte M. Instrument breakage as a complication of elbow arthroscopy in a dog. Aust Vet J 2014;92(4):128-131.
 |
 |
 |
| Dr. Uli Schmiddem | Dr. N Hawi | Dr. E M Suero |
| How to Cite This Article: Schmiddem U, Hawi N, Suero EM, Meller R. Combined Fluoroscopic and Arthroscopic Detection and Removal of a Foreign Body Lost During Elective Shoulder Arthroscopy: A Case Report. Journal of Orthopaedic Case Reports 2017 Mar-Apr;7(2):78-81. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com