[box type=”bio”] What to Learn from this Article?[/box]
Although being a congenital lesion, lumbosacral transitional vertebrae and Bertolotti’s syndrome may be presented in elderly population with sciatica and low back pain.
Case Report | Volume 7 | Issue 3 | JOCR May – June 2017 | Page 9-12| Stylianos Kapetanakis, Constantinos Chaniotakis, Constantinos Paraskevopoulos, Pavlos Pavlidis. DOI: 10.13107/jocr.2250-0685.782
Authors: Stylianos Kapetanakis[1], Constantinos Chaniotakis[2], Constantinos Paraskevopoulos[2], Pavlos Pavlidis[3]
[1] Department of Spine and Deformities, Interbalkan European Medical Center, Thessaloniki, Greece.
[2] Department of Anatomy, Medical School, Democritus University of Thrace, Alexandroupolis, Greece.
[3] Laboratory of Forensic Sciences, Medical School, Democritus University of Thrace, Alexandroupolis, Greece.
Address of Correspondence
Dr. Stylianos Kapetanakis,
Medical School of Alexandroupolis, Dragana-681 00. Greece.
E-mail: stkapetanakis@yahoo.gr
Abstract
Introduction: Castellvi Type III lumbosacral transitional vertebrae (LSTV) is an unusual case of Bertolotti’s syndrome (BS) due to extraforaminal stenosis, especially manifesting in elderly patients.
Case Report: We report a case of BS in a 62 years old Greek female. The signs of the clinical examination are low back pain, sciatica, hypoesthesia, and pain to the contribution of L5 nerve. Imaging techniques revealed an LSTV Type III a (complete sacralization between LSTV and sacrum).
Conclusion: Despite the fact that LSTV is a congenital lesion, the clinical manifestation of BS may present in the elderly population. The accumulative effect of the gradual degeneration of intervertebral foramen (stenosis) may lead to the compression of extraforaminal portion of the nerve root.
Keywords: Bertolotti’s syndrome, lumbosacral transitional vertebrae, low back pain, extraforaminal stenosis, classification of lumbosacral transitional vertebrae.
Introduction
In 1917, Mario Bertolotti described the presence of an anatomical variation of the most caudal lumbar vertebrae, with an abnormally enlarged transverse process which articulated or fused unilaterally or bilaterally with the sacrum basis or iliac crest. This “mega” apophysis or the so called lumbosacral transitional vertebrae (LSTV), when associated with chronic, persistent low back pain (LBP) or sciatica, composes the “Bertolotti’s Syndrome” (BS) [1, 2, 3, 4, 5]. The prevalence of LSTV varies from 3% to 35% in the general population [1, 2, 6, 7, 8, 9]. Although a 13% of the patients with LSTV are asymptomatic, the incidence of BS is diagnosed in 4-8% of patients with LBP. BS is more frequently encountered in patients <30 years old, in a percentage of 18.5% [2, 3, 4]. The etiology of LBP in BS is multifactorial. LBP is associated with changes at the intervertebral disk, such as early degeneration or herniation, at the spinal canal above the level of the LSTV, at the contralateral facet joints in cases of unilateral fusion, or extraforaminal changes at the site of articulation between LSTV and sacrum ala/iliac crest [3, 4, 5, 6]. We present an unusual case of Castellvi Type III an LSTV, which causes extraforaminal stenosis and impingement of the L5 nerve root, leading to BS.
Case Report
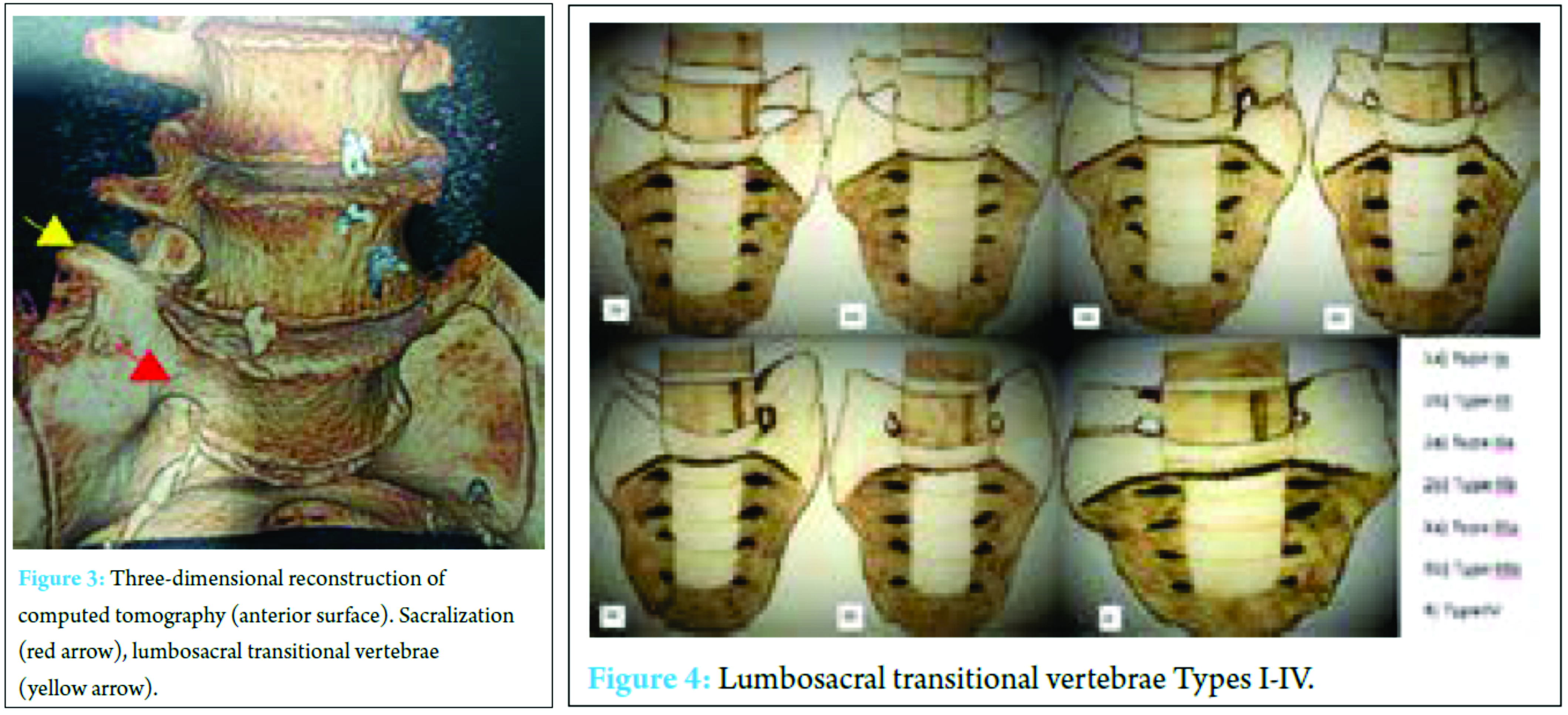
A 62-years-old woman presented to our Department in November 2016, with a history of LBP for 3 months and sciatica for the previous month. She mentioned the systematic use of analgesics (paracetamol), with no subsequent pain relief. Her past medical history was unremarkable for comorbidities, except of the presence of a cardiac pacemaker, due to sinus bradycardia. The use of magnetic resonance imaging (MRI) was, thus, contraindicated. The patient was subjected to a complete clinical examination and laboratory testing. During the physical examination, hypoesthesia and pain found at the distribution of L5 nerve, without signs of muscular weakness in the lower extremity (all reflexes were normal). Afterward, plain radiograph of lumbar spine region depicted a unilateral LSTV on the right side, which was in contact with the base of sacrum (Fig. 1). 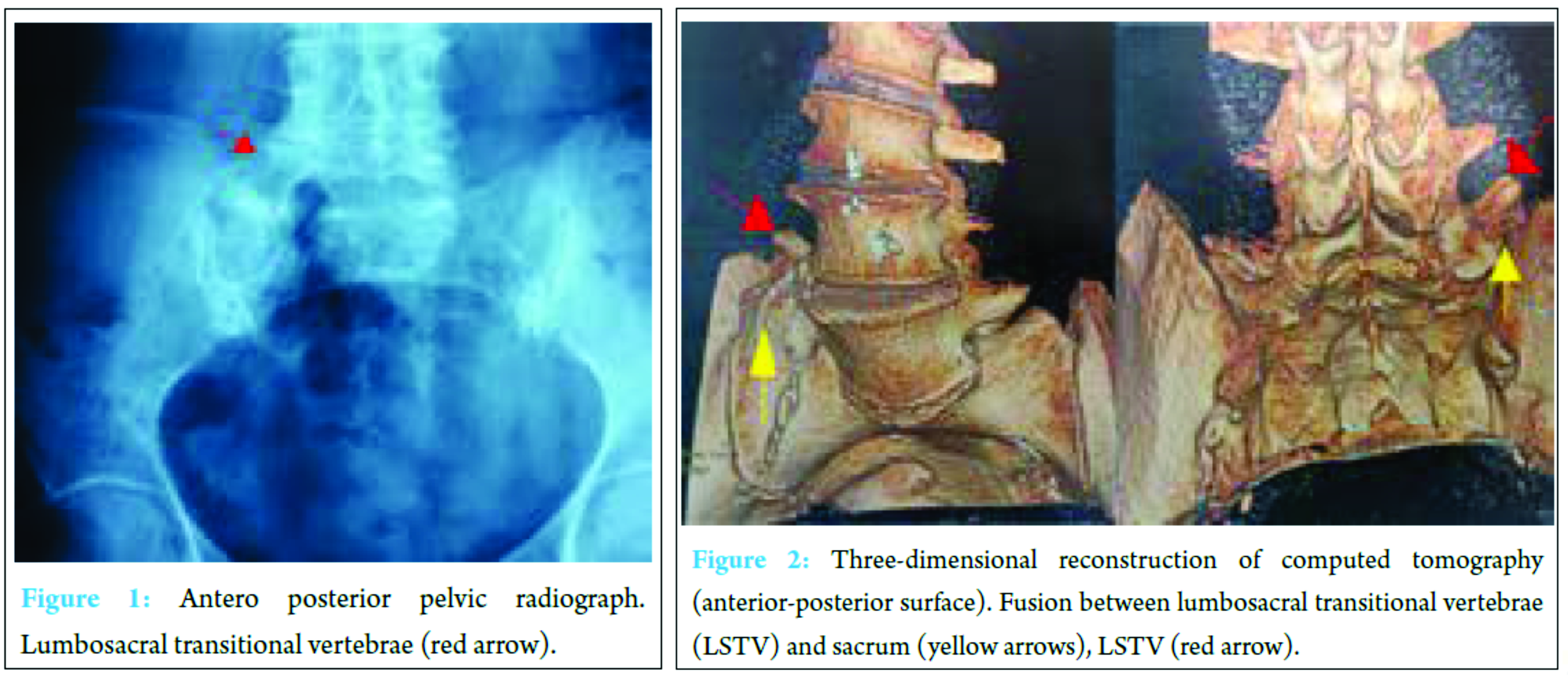
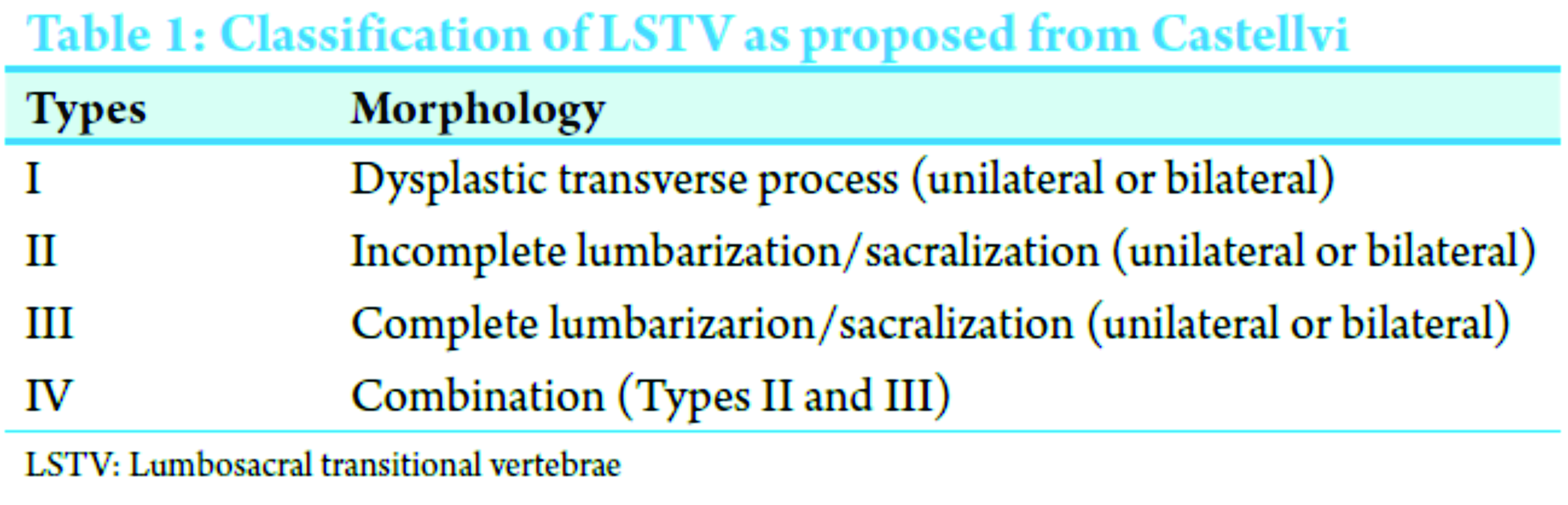
3D CT scan images revealed a complete unilateral sacralization (Type III a, according to Castellvi et al. classification). Nevertheless, the findings were consistent with extraforaminal stenosis due to the accumulative effect of the gradual degeneration of intervertebral foramen and subsequent nerve root compression at the corresponding level. Inflammatory markers were normal in the blood routine examination. Our findings from physical examination and CT scan imaging were suggestive of BS. The patient was initially prescribed with nonsteroidal anti-inflammatory drugs (NSAIDs) for 7 days, followed by a 2-week therapy with methylprednisolone. She was subjected to follow-up to detect any deterioration of the neurological symptomatology or the LBP. In follow-up, she did not report any symptoms, and in the clinical examination, we found a light mubness at the distribution of L5 nerve.
Discussion
According to Castellvi et al., LSTV is classified with a Ferguson radiograph, which allows a 30° angled anteroposterior (AP) view of the lumbosacral joint, into four types (Fig. 4) based on its morphological characteristics (Table 1).
Type I exhibits unilateral (I a) or bilateral (I b) dysplastic transverse processes, measuring at least 19 mm at the craniocaudal axis. Type II includes incomplete unilateral (II a) or bilateral (II b) lumbarization/sacralization with an enlarged transverse process that has a diarthrosis between itself and the sacrum. Type III involves unilateral (III a) or bilateral (III b) lumbarization/sacralization with complete osseous fusion of the transverse process (es) to the sacrum. Type IV describes a unilateral Type II transition with the coexistence of a Type III at the contralateral side [1, 4, 5, 6]. As it was remarked in the literature, Types II-IV appear to be related with BS, while Type I remains asymptomatic and in the majority of cases incidentally found. The prevalence of Type III corresponds to a percentage of 8.3-11.5% [1, 8]. The anatomical variations of LSTV are present in varying frequencies, and their prevalence seems to alter among males and females [1, 8]. Especially, Nardo et al. commented on the higher prevalence of LSTV among males rather than females. According to various authors, the appearance of LSTV is associated with adjacent level disc degeneration, potentially due to the distribution of abnormal biomechanical stresses above the fusion [1, 2, 10, 11]. Otani et al. noticed that the prevalence of disc herniation was higher in patients positive to LSTV (17%), compared to the control group without LSTV (11%) [10]. Castellvi et al. claimed that disc degeneration seems to be associated with LSTV. In addition to this, the incidence of disc degeneration was higher in the supradjacent level to LSTV (63.5%) and lower in the infradjecent level to LSTV (34%) [1]. Elster found that the incidence of disc degeneration and spinal stenosis was significantly higher in the disc superior the LSTV, compared to other discs [2]. In addition, Aihara et al. investigated the role of the iliolumbar ligament in the disc degeneration. According to the study, the iliolumbar ligament was thinner and weaker in the level above LSTV, in patients who suffered from disc degeneration in this exact level [11]. The knowledge of the pathophysiology can explain the mechanism of the disc degeneration. The presence of LSTV interrupts the anatomy of the spine. Altered anatomy imposes difficulties in the surgical approach of the lumbosacral region [5]. Chithriki et al. conducted a prospective study of 441 patients, estimating the prevalence of LSTV at 8, 4%. In patients with sacralization of the L5 vertebra, the level of aortic bifurcation was found at L3 in 59%, at L4 in 23% and at the mid-vertebral level L3/L4 in 14%, while in those with lumbarization of the S1 vertebra, at L4 in 47%, at the mid-vertebral L4/L5 level in 33% and at the L5 in 13% [7]. Furthermore, Kim et al. concluded that the Tuffier’s line (line connecting the highest points of iliac crests) was not found in its ordinary position, which is at the L4 or L5 body. The finding is of great clinical significance during needle insertion in the lumbar region [12]. Weiner et al. mentioned that the junction between common iliac veins and inferior vena cava was located lower than its ordinary location at the L5 intervertebral level, anteriorly to the vertebral body and right to the midline, leading to potential complication during the anterior approach of the L4-L5 intervertebral disc [13]. The diagnosis of BS is based on clinical examination and imaging of the lumbosacral spine (AP radiographs, CT, MRI, and skeletal scintigraphy). AP radiographs are useful for identifying the presence of LSTV but are nonspecific to determine whether the source of pain is related to LSTV [5, 7, 9, 11, 14]. On the other hand, MRI scans are highly reliable [3, 6, 9, 12]. CT-scan provides information on the degenerative lesions of the osseous structures (hypertrophy or bone sclerosis) [4]. In addition to CT-scan, there is single-photon emission computed tomography/CT for the detection of bone abnormalities due to stress [4, 5, 14, 15]. MRI reveals the disc herniation or potential edema of the articulation of the LSTV with the sacrum, which may coexist in patients suffering from BS [4. 10, 11, 14]. 3D MRI and CT are highly reliable for diagnosing L5 nerve compression due to extraforaminal stenosis by LSTV [4]. Skeletal scintigraphy depicts an increase on bone metabolic activity in certain foci [4, 5, 14]. The therapeutic approach of BS is conservative treatment and surgery [5, 6, 9, 14, 15]. The first-line therapeutic option is the conservative treatment, which consists of physical therapy, NSAIDs, corticosteroids and muscular relaxants [4, 5, 6, 14, 15]. Especially, corticosteroids and local anesthetic drugs can be injected into the articulation for both diagnosis (determination whether or not the pain originates from the pseudarthrosis) and treatment [6, 14, 15]. If so, and if conservative therapy is unsuccessful, surgical resection or fusion of LSTV is required [6, 14, 15].
Conclusion
Despite the fact that LSTV is a congenital lesion, the clinical manifestation of BS may present in the elderly population. The accumulative effect of the gradual degeneration of intervertebral foramen (stenosis) may lead to the compression of extraforaminal portion of the nerve root. Spine physicians should bear in mind that the symptomatology from LSTV may not only be presented in young population. BS should be a part of differential diagnosis in patients with LBP and spinal stenosis in the most caudal level of spine.
Clinical Message
LSTV is a congenital lesion that leads to subsequent nerve root impingement and BS. Although it is more commonly encountered in young people, it should be included in the differential diagnosis in elderly population who present with LBP and sciatica.
References
1. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 1984;9(5):493-495.1. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 1984;9(5):493-495.
2. Elster AD. Bertolotti’s syndrome revisited. Transitional vertebrae of the lumbar spine. Spine (Phila Pa 1976) 1989;14(12):1373-1377.
3. Quinlan JF, Duke D, Eustace S. Bertolotti’s syndrome. A cause of back pain in young people. J Bone Joint Surg Br 2006;88(9):1183-1186.
4. Neelakantan S, Anandarajan R, Shyam K, Philip B. Multimodality imaging in Bertolotti’s syndrome: An important cause of low back pain in young adults. BMJ Case Rep 2016;2016. pii: Bcr2016217121.
5. Jancuska JM, Spivak JM, Bendo JA. A review of symptomatic lumbosacral transitional vertebrae: Bertolotti’s syndrome. Int J Spine Surg 2015;9:42.
6. Konin GP, Walz DM. Lumbosacral transitional vertebrae: Classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol 2010;31(10):1778-1786.
7. Chithriki M, Jaibaji M, Steele RD. The anatomical relationship of the aortic bifurcation to the lumbar vertebrae: A MRI study. Surg Radiol Anat 2002;24(5):308-312.
8. Nardo L, Alizai H, Virayavanich W, Liu F, Hernandez A, Lynch JA, et al. Lumbosacral transitional vertebrae: Association with low back pain. Radiology 2012;265(2):497-503.
9. Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg 2007;73(6):687-695.
10. Otani K, Konno S, Kikuchi S. Lumbosacral transitional vertebrae and nerve-root symptoms. J Bone Joint Surg Br 2001;83(8):1137-1140.
11. Aihara T, Takahashi K, Ogasawara A, Itadera E, Ono Y, Moriya H. Intervertebral disc degeneration associated with lumbosacral transitional vertebrae: A clinical and anatomical study. J Bone Joint Surg Br 2005;87(5):687-691.
12. Kim JT, Bahk JH, Sung J. Influence of age and sex on the position of the conus medullaris and Tuffier’s line in adults. Anesthesiology 2003;99(6):1359-1363.
13. Weiner BK, Walker M, Fraser RD. Vascular anatomy anterior to lumbosacral transitional vertebrae and implications for anterior lumbar interbody fusion. Spine J 2001;1(6):442-444.
14. Dizdarevic I, Bishop M, Sgromolo N, Hammoud S, Atanda A Jr. Approach to the pediatric athlete with back pain: More than just the pars. Phys Sportsmed 2015;43(4):421-431.
15. Mercader Rodríguez B, Sánchez RF, Domenech Abellán E, Parra JZ, Canovas CS, Castellón Sánchez MI. Bertolotti syndrome: A little known cause of low-back pain in childhood. J Pediatr 2015;166(1):202.
 |
 |
 |
 |
| Dr. Stylianos Kapetanakis | Dr. Constantinos Chaniotakis | Dr. Constantinos Paraskevopoulos | Dr. Pavlos Pavlidis |
| How to Cite This Article: Kapetanakis S, Chaniotakis C, Paraskevopoulos C, Pavlidis P. An Unusual Case Report of Bertolotti’s Syndrome: Extraforaminal Stenosis and L5 Unilateral Root Compression (Castellvi Type III an LSTV). Journal of Orthopaedic Case Reports 2017 May-June;7(3):9-12. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com