[box type=”bio”] What to Learn from this Article?[/box]
Pyknodysostosis though a rare disorder, proper pre-operative planning is mandatory to prevent complication.
Case Report | Volume 7 | Issue 3 | JOCR May – June 2017 | Page 54-58| G Subramanya Gandhi, V Vijayanarasimhan, Lionel John, S Kailash, E Sathish Balaji. DOI: 10.13107/jocr.2250-0685.804
Authors: G Subramanya Gandhi[1], V Vijayanarasimhan[1], Lionel John[1], S Kailash[1], E Sathish Balaji[1]
[1] Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India.
Address of Correspondence:
Dr. G Subramanya Gandhi,
Prestige Bella Vista Apartments, Tower 2A, Unit 2183, 18th Floor, Iyyapanthangal, Chennai – 600 056, Tamil Nadu, India.
E-mail: subbu719@gmail.com
Abstract
Introduction: Pyknodysostosis is congenital osteosclerotic skeletal dysplasia of a rare entity. It is an autosomal recessive disease which presents with short stature and generalized osteosclerosis of skeleton as result of decreased bone turnover. Here, the authors report a case of pyknodysostosis who presented to our emergency room with a pathological fracture in the shaft of the femur for which operative intervention was carried out.
Case Report: A 30-year-old female presented to our emergency room with a history of trivial injury to right thigh region and was diagnosed as fracture in her right femur shaft region. After a detailed clinical, radiological, and blood investigations, the patient was taken up for operative modality of intervention in the form of plate osteosynthesis. As the medullary canal was narrow and bone was osteosclerotic, the option of closed intramedullary interlocking nailing was ruled out. Hence, we proceeded with open reduction and internal fixation with plate osteosynthesis using a board dynamic compression plate. Post-operative period was uneventful. Patient underwent non-weight bearing mobilization for 2 months. At 10-week post-operative follow-up, the patient presented with pain over surgical site and radiological examination showed no signs of union. The patient underwent additional plating augmented with bone grafting using grafts harvested from iliac crest and synthetic bone graft. The patient developed deep-seated infection immediate post-operative period for which she was treated with wound debridement, and appropriate intravenous antibiotics were given 2 weeks and orally for 4 weeks. At 6-month follow-up, the patient is able to carry her day-to-day activity with complete recovery and radiological signs of union. The patient had classical clinical features suggestive of pyknodysostosis. Patient has 2 siblings of same family (one brother and sister) with similar clinical and radiological features.
Conclusion: Recognition of these clinical and radiological signs is important to make the diagnosis of pyknodysostosis and prevent possible complications. Additional care must be taken in treating these patients.
Keywords: Pyknodysostosis, pathological femur fracture, osteomyelitis.
Introduction
In 1962, Maroteaux and Lamy first described pyknodysostosis as a rare genetic disorder [1]. Disease had also been called by other name Toulouse-Lautrec syndrome, after the French artist Henri de Toulouse-Lautrec, who suffered from it [1]. It is an autosomal recessive osteochondrodysplasia [2]. Here the authors report 3 siblings of same family who had clinical and radiological features of short stature, acroosteolysis, frequent episodes of fracture, skull deformities, poor dentition and generalized osteosclerosis.
Case Report
A 30-year-old female presented to our hospital with trivial injury to her right thigh, following which she had pain over right thigh and unable to weight bear on the involved lower limb. Other associated injuries were ruled out at the time of admission in the emergency room. Physical examination revealed swelling, tenderness, and deformity over the middle-third of her right thigh region without neurovascular deficit. Patient was stabilized initially in our emergency department, and radiograph of right femur showed displaced transverse fracture in the femoral shaft (Fig. 1). The other radiographic findings were diffuse osteosclerosis and narrow medullary canal. The patient gave a history of earlier episodes of fracture for which conservative treatment in form of native splinting had been done. Thus, a diagnosis of pathological fracture was made. On general examination, the patient had short stature and dysmorphic facies with radiological signs of generalized osteosclerosis and narrow medullary canal. A detailed history, clinical, and radiological examination was carried out. She was second child of four siblings. The first child died days after delivery, of unknown cause, and other two younger siblings had similar clinical features (Fig. 2). Parents had a first-degree consanguinity. The antenatal history was not significant. Milestone and intelligence attainted appropriate for age. There was a history of frequent episodes of upper respiratory tract infection, snoring during sleep since childhood. The patient also gave a history of hard of hearing on the right side. The patient went through regular general medical checkups, and there was no significant treatment history.
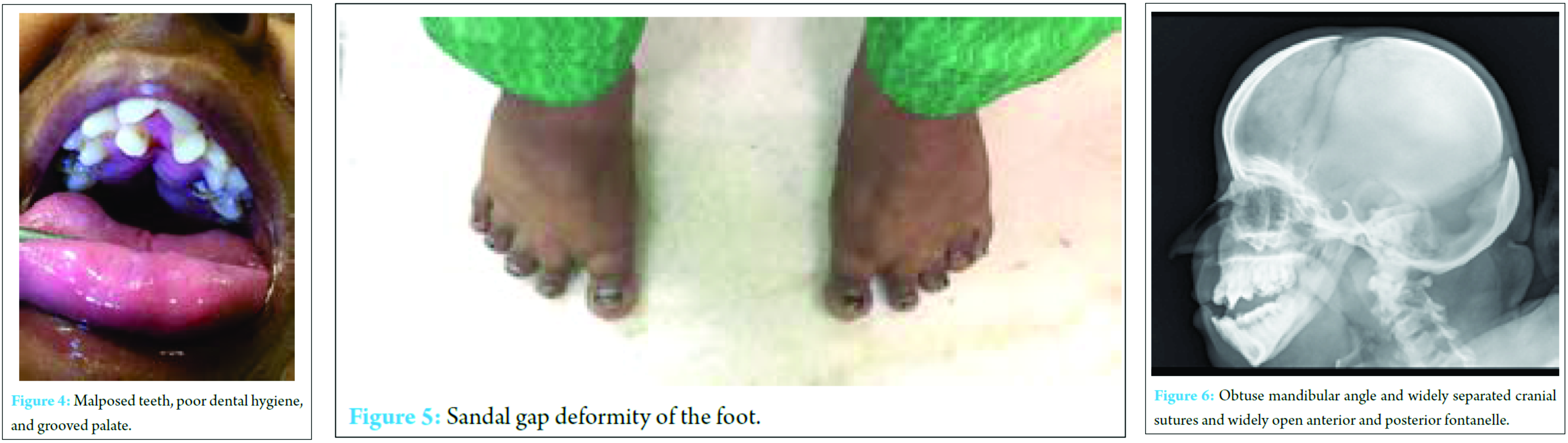
On general physical examination, weight of patient was 63 kg; her standing height was 126 cm; her upper segment and lower segment length were 64 and 62 cm, chest expansion of 3 cm, respectively, with a head circumference of 49 cm. Other clinical features include dysmorphic facies, frontal and parietal bossing, beaked nose, midfacial hypoplasia, short hands and feet with dysplastic nail (Fig. 3), grooved palate (Fig. 4), dental caries, impacted and malposed tooth, and sandal gap deformity of the foot (Fig. 5). Radiograph of the skull was found to be widely open anterior and posterior fontanelle, with obtuse mandibular angle and separated cranial sutures (Fig. 6). Radiograph of the hand showed aplastic terminal phalanges with acroosteolysis. Abovementioned clinical and radiographic findings suggested pyknodysostosis as the most likely diagnosis. The patient was taken up for surgery within a week from injury. An intramedullary interlocking nailing was contemplated initially for fracture fixation.
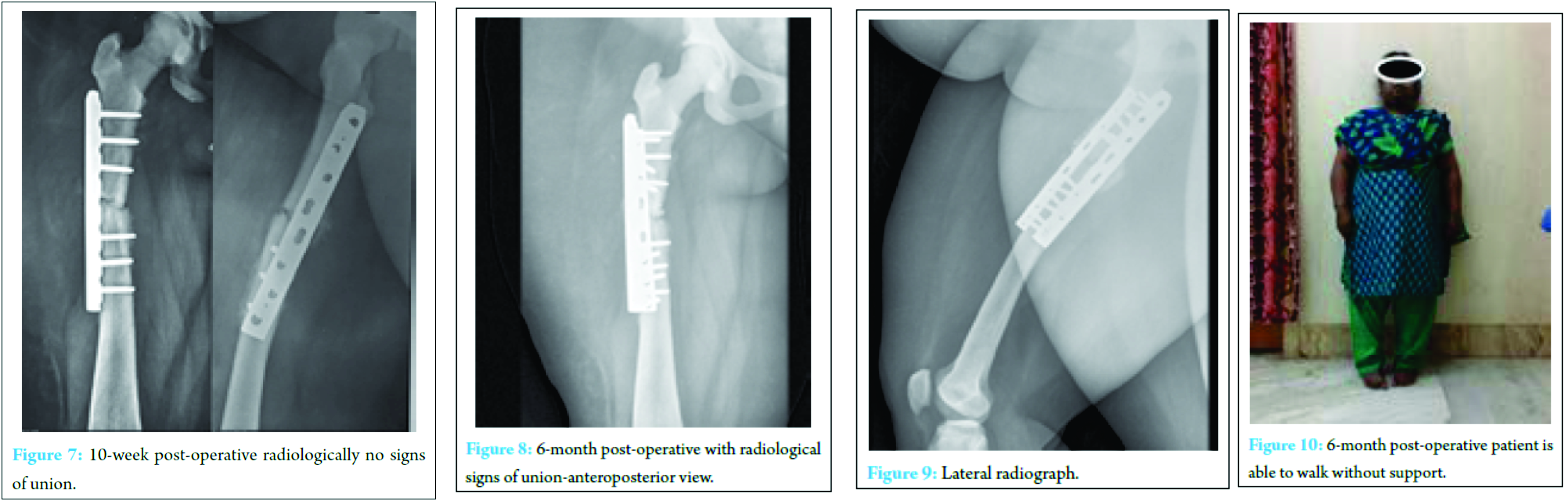
However, for this case, we preferred plate osteosynthesis because of the altered anatomy of the bone with a narrow medullary canal and severe osteosclerosis. Under Spinal anaesthesia, through lateral approach to the middle third of femur, a 12 cm incision was made. After deep dissection, fracture site was identified and exposed. After reducing fractures fragments an “8 holed broad dynamic compression plate with 3 proximal and 3 distal screws in compression mode was used for fracture fixation (Fig. 7).”
The difficulty encountered in the intra-operative period include, a difficulty in drilling the cortices and excess blood loss. The wound was closed in layers after adequate hemostasis. The immediate post-operative period was uneventful, and the patient discharged on the 14th post-operative day. The patient was discharged with advice of non-weight bearing walking with the help of walker support for minimum of 2 months and advised to review in the out-patient department for follow up every fortnight. At 10-week post-operative, after patient has been started on partial weight bearing walking, the patient reported with the complaints of pain over surgical site. On radiological examination, patient was found to have no signs of union at the fracture. Patient was immobilized for one month, but even after that, there were no signs of union. Hence, an additional stabilization procedure was done in the form of plating with autogenous cancellous bone grafting. Bone graft harvested from ipsilateral iliac crest was inadequate, and there was heavy bleeding from donor site so that an additional synthetic bone graft substitute was used. In the immediate post-operative period, patient developed deep seated infection which showed organism grown was staphylococcus aureus for which wound debridement was done. Patient was started on Intravenous antibiotics of Linezolid 600 mg twice a day after obtaining culture and sentivity report for period of 2 weeks, followed by oral antibiotics for 4 weeks. Patient was discharged 4 weeks later after complete subsidence of infection. Patient was advised physiotherapy in form of static and dynamic Quadriceps strengthening exercises,followed by hip and knee mobilization exercises and strict non weight bearing for 2 months. . At 3-month post-operative follow-up, there were signs of union clinically and radiologically (Fig. 8 and 9). The patient at present in the 6-month post-operative period with fracture united and on full weight bearing carrying out her daily activities without difficulty (Fig. 10).
Discussion
Pyknodysostosis is caused by mutation in gene which is found to code the enzyme cathepsin K, it is a lysosomal storage disease of the bone [3], usually diagnosed at an early age with incidence estimated to be 1.7 per 1 million births [4]. Characteristic clinical and radiological signs of Pyknodysostosis help us to differentiate it from other osteosclerotic conditions [5]. The genetic study was not performed in our patient.Osteopetrosis and cleidocranial dysostosis have a few common findings [6]. In Osteopetrosis it is characterized by generalized increased osteosclerosis. Death has also been reported in the malignant forms which are recessive, there will be obli•teration of medullary canal leading to severe aplastic anemia [7]. Patients with cleidocranial dysostosis is usually present normal stature [8]. Most of other features are similar to that of pyknodysostosis as in our patient except that, there was no anemia or organomegaly. In our patient, the audiometry showed senorineural hearing loss which is exceptional in pyknodysostosis. The fundus examination of the patient showed refractive errors too. Until now, there is no specific treatment for this condition has been described but only symptomatic management [9]. The commonly described complications in these patients are frequent fractures due to increased fragility and poor dental hygiene for which proper precautionary and management should be done [10]. In literature, Osteomyelitis [11, 12] which is one of the dreadful complication has been reported due to impaired blood supply following surgery in these conditions, was present in our case also due to nature of the disease. These patients have been found to have significant improvement in final height by administrating growth hormone therapy [13, 14]. Psychological management was given to our patient to help her to accept her dysmorphic appearance. Prenatal diagnosis by direct sequencing of the gene from fetal DNA, when the mutation is known might be required [15].
Conclusion
The clinical and radiological features are important for the diagnosis of this disease. It is important to make the diagnosis as early as possible to plan the treatment. Our patient has a significant clinical history of all three siblings of same family been affected by pyknodysostosis which is one of very rare presentation. Our patient also showed sensorineural hearing deficit and sandal gap deformity of the foot which is not frequently reported in the previous literature.
Clinical Message
We should consider proper pre-operative planning, for these cases having in mind, they are more prone for infection. Although pyknodysostosis condition is a rare entity, the incidence of fracture and its related complications is not uncommon. In this case, we encountered both long bone fracture following a trivial injury and post-operative infection. Hence, anticipating such complication and optimal management will lead to a better quality life in these patients.
References
1. Maroteaux P, Lamy M. The malady of Toulouse-Lautrec. JAMA 1965;191(9):715-717.1. Maroteaux P, Lamy M. The malady of Toulouse-Lautrec. JAMA 1965;191(9):715-717.
2. Alves N, Oliveira RJ, Deana NF, Sampaio JC. A morphological features of pyknodysostosis with emphasis on clinical and radiographic maxillofacial findings. Int J Morphol 2013;31(3):921-924.
3. Donnarumma M, Regis S, Tappino B, Rosano C, Assereto S, Corsolini F, et al. Molecular analysis and characterization of nine novel CTSK mutations in twelve patients affected by pyknodysostosis. Mutation in brief #961. Online. Hum Mutat 2007;28(5):524.
4. Fujita Y, Nakata K, Yasui N, Matsui Y, Kataoka E, Hiroshima K, et al. Novel mutations of the cathepsin K gene in patients with pyknodysostosis and their characterization. J Clin Endocrinol Metab 2000;85(1):425-431.
5. Kneal E, Sante LR. Osteopetrosis (marble bones); Report of a case with special reference to early roentgenologic and pathological findings. AMA Am J Dis Child 1951;81(5):693-707.
6. Ebtesam M, Matrawy K, Shwel Y. Pyknodysostosis: Clinical andradiological two new Egyptian families. J Pediatr Sci 2012;4(1):e124.
7. Turan S. Current research on pyknodysostosis. Intractable Rare Dis Res 2014;3(3):91-93.
8. Nardi J, Meslier N. Pyknodysostosis and obstructive sleep apneasyndrome. Méd du sommeil 2010;7(2):63-65.
9. Muto T, Michiya H, Taira H, Murase H, Kanazawa M. Pyknodysostosis. Report of a case and review of the Japanese literature, with emphasis on oral and maxillofacial findings. Oral Surg Oral Med Oral Pathol 1991;72(4):449-455.
10. Barnard B, Hiddema W. Pyknodysostosis with the focus on clinical and radiographic findings. S Afr J Radiol 2012;16(2):74-76.
11. Mujawar Q, Naganoor R, Patil H, Thobbi AN, Ukkali S, Malagi N. Pyknodysostosis with unusual findings: a case report. Cases J 2009;2(2):6544.
12. Fukada H, Uehara S, Ando S, Shinoda K. Case of pyknodysostosis-its oral aspects. J Nihon Univ Sch Dent 1967;9(4):164-169.
13. Karamizadeh Z, Ilkhanipoor H, Bagheri F. Effect of growth hormone treatment on height velocity of children with pycnodysotosis. Iran J Pediatr 2014;24(2):161-165.
14. Azagui Y, Zaidane A, Belmoubarek A, Ahed K, Haddoun AR, Ouarab M. Diaphyseal femur fracture in pyknodysostosis: A case report. Rev Mar Rhum 2013;24:52-55.
15. Elmore SM. Pyknodysostosis: A review. J Bone Joint Surg 1967;49(1):153-162.
 |
 |
 |
 |
 |
| Dr. G Subramanya Gandhi | Dr. V Vijayanarasimhan | Dr. Lionel John | Dr. S Kailash | Dr. E Sathish Balaji |
| How to Cite This Article: Gandhi GS, Vijayanarasimhan V, John L, Kailash S, Balaji ES. Fracture Management in Pyknodysostosis – A Rare Case Report. Journal of Orthopaedic Case Reports 2017 May-June;7(3):54-58. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com