[box type=”bio”] What to Learn from this Article?[/box]
Excellent implant survivorship figures do not necessarily mean that an implant is excellent.
Case Report | Volume 7 | Issue 3 | JOCR May – June 2017 | Page 76-79| Tamas Halasi, Declan Reidy, Shane Guerin. DOI: 10.13107/jocr.2250-0685.814
Authors:
Tamas Halasi[1], Declan Reidy[1], Shane Guerin[1]
[1] Department of Orthopaedic Surgery, Cork University Hospital, Wilton, Cork, Ireland.
Address of Correspondence
Dr. Tamas Halasi,
Department of Orthopaedic Surgery, Cork University Hospital, Wilton, Cork, Ireland.
E-mail: dr.tamas.halasi@gmail.com
Abstract
Introduction: The Smith-Petersen vitallium mold arthroplasty was a real landmark in arthroplasty surgery as this was the first technique which produced predictable and satisfactory results.
Case Report: We present the longest known follow-up of any hip arthroplasty in literature. The arthroplasty was performed in 1949 in London on a 30-years-old female patient with congenital hip dysplasia, and it was revised in 2014 after 65 years.
Conclusion: Total hip arthroplasties nowadays give better functional results, but the fact that the patient got 65 years of the relatively good function is noteworthy and is a tribute to Dr. Marius Nygaard Smith-Petersen.
Keywords: Smith-Petersen, vitallium, arthroplasty, follow-up, orthopedic.
Introduction
The first arthroplasty surgeons tested various materials and techniques before the nowadays used design was developed. Smith-Petersen introduced his vitallium mold arthroplasty in 1938 [1], and follow-up studies have shown high levels of patient satisfaction [2]. We now report the longest known follow-up of any hip arthroplasty in literature. We feel that this 65-year long story of one of the pioneers of arthroplasty deserves appreciation and closure.
Case Report
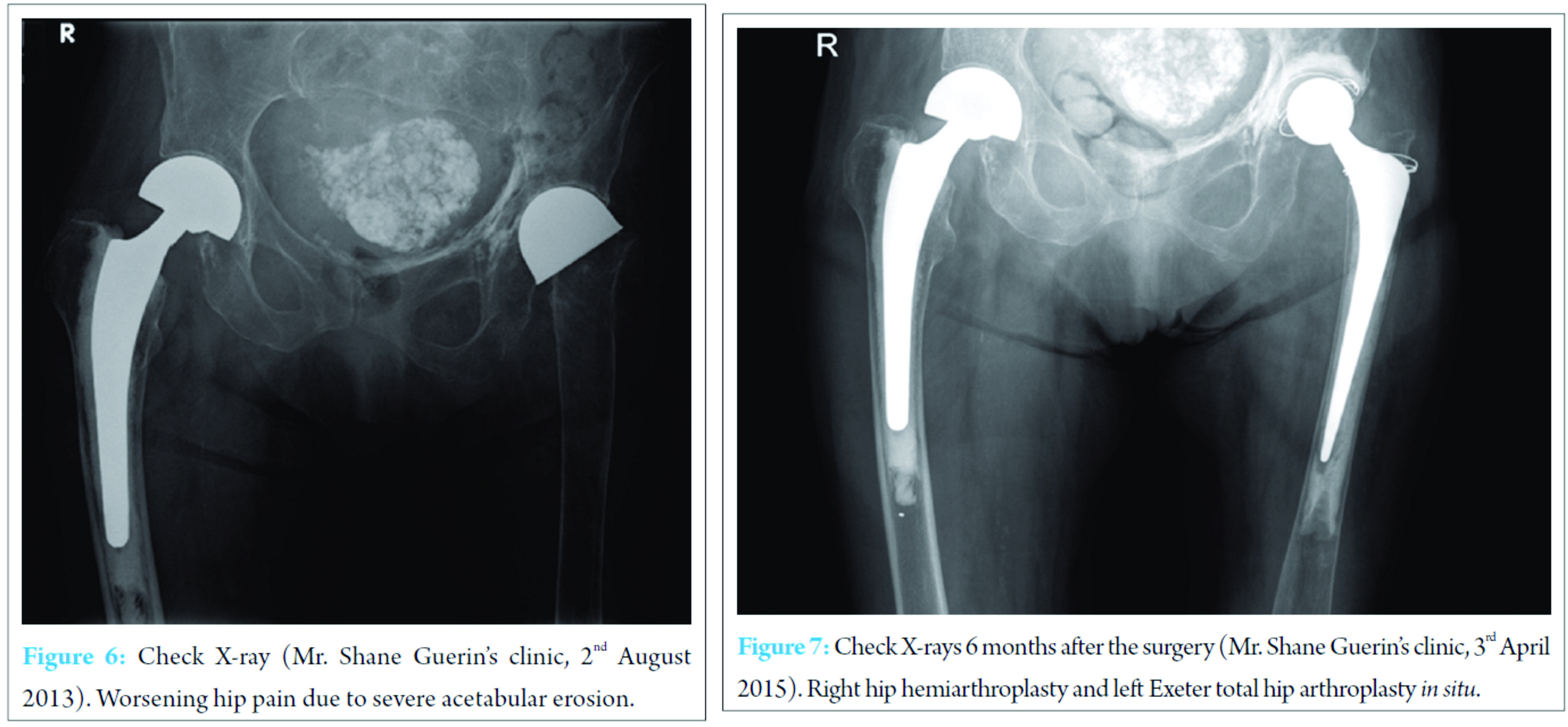
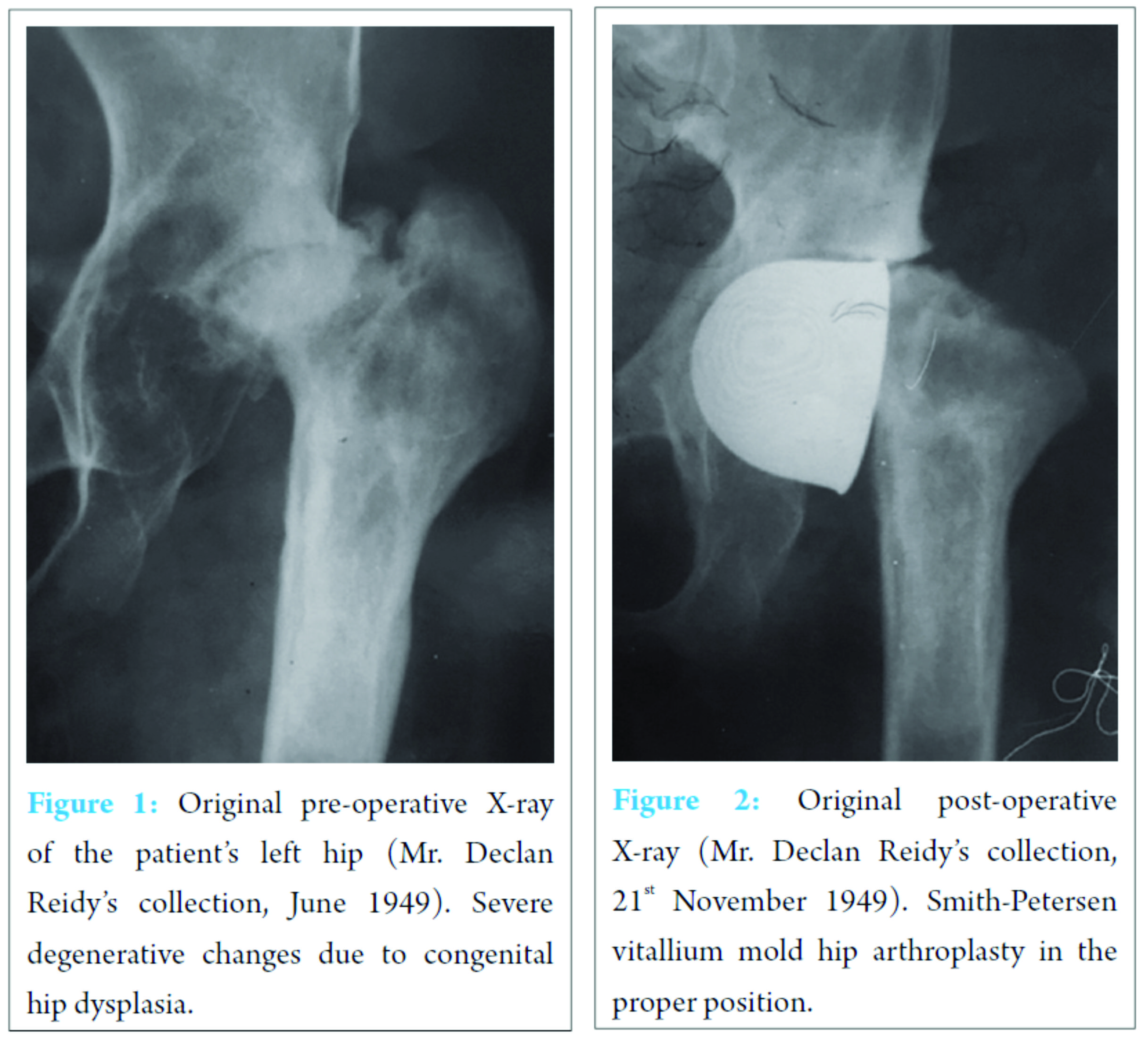
E. H. was born in 1919 with congenital dysplasia of her left hip. She had had multiple operations on it, but she still developed gross degenerative changes by the age of 30 (Fig. 1). Mr. W. Alexander Law, an orthopedic surgeon, performed a Smith-Petersen vitallium mold hip arthroplasty in October 1949 in London Hospital (Fig. 2).
Discussion
The first arthroplasty surgeons around the turn of the 19th century experimented with various materials. Initially, ivory was used to replace the damaged femoral head; later interpositional arthroplasty became more popular placing various tissues (pig bladder, fascia lata, and skin) between articulating surfaces. Unfortunately, these techniques produced poor prosthesis survival rates and unsatisfactory functional results [5]. Dr. Marius Nygaard Smith-Petersen was born in 1886 in Norway, he graduated from Harvard Medical School, and after that, he lived and worked in Boston until his death in 1953. He introduced the mold arthroplasty in 1923 [1]. The idea came from a case where he removed an embedded piece of glass from a man’s back, and he observed that a reactive synovial-like membrane had developed around it. His original design was a hollow glass hemisphere which was placed over the femoral head to stimulate cartilage regeneration of the hip joint on both sides of the glass. His intention was to remove the glass after the cartilage was restored, but unfortunately, glass was not durable enough, and it quickly failed for almost every patient. He started to experiment with different materials, and finally, his dentist suggested vitallium, a new cobalt-chrome alloy which had just been introduced in dentistry at the time [6]. The first vitallium mold arthroplasty was performed in 1938. In the following decades, his team performed more than 500 procedures [1], and it quickly became a popular operation worldwide. The results were promising [2], and the indications were broad including intracapsular hip fractures, osteoarthritis, rheumatoid arthritis, Perthes disease, congenital hip dislocations, and even septic arthritis. This was a real landmark in arthroplasty surgery as this was the first technique and material which produced predictable and satisfactory results. There were various attempts through the years to modify the Smith-Petersen vitallium mold arthroplasty. The Judet brothers developed their similar prosthesis in 1948. They used acrylic instead of vitallium and they also introduced the intramedullary stem component. Their initial results were promising; the longest known follow-up of Judet prosthesis is 47 years [7]. The femoral stem gave the arthroplasty additional stability, but it was also sensitive to wear and loosening [8]. The Smith-Petersen arthroplasty was still superior to the new acrylic based prosthesis in hip pain relief and patient satisfaction rate [9]. Vitallium has been proven to be an excellent choice of material, and similar cobalt-chrome alloys are still in use in orthopedic implants. These two prostheses were the most popular and most durable designs until the introduction of the modern low-friction hip replacement techniques by Sir John Charnley in the 1960s. His design – metal femoral stem, polyethylene acetabular component and acrylic bone cement – is considered to be the first real total hip arthroplasty and it is identical, in principle, to the prostheses used nowadays [5]. There are only a few case reports describing comparably long follow-ups of hip arthroplasties. Radcliffe and Geary in 1997 reported a patient with 46-year survival of a Smith-Petersen mold arthroplasty [10]. In 2006 Wright et al. reported a case with 56-year follow-up [11], in the same year Landham et al. presented a case with 48-year follow-up [12.] In 2008 Northover and Maqsood reported a patient with 58-year follow-up [13]. At 65 years our case is the longest survival recorded. What these case reports had in common is that all these patients lived a long and fairly active life and they were very happy with their functional results for a surprisingly long time despite their significant leg length discrepancies..
Conclusion
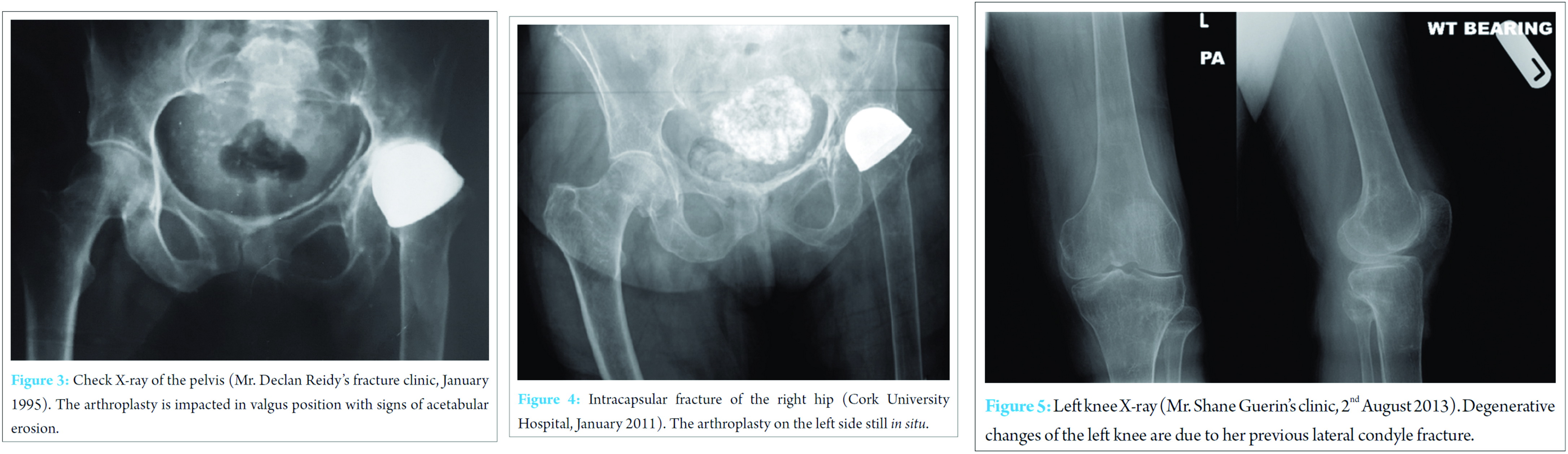
We can assume that total hip arthroplasties nowadays give better functional results, but there were no formal scoring systems 50-60 years ago to provide objective and comparable data with the modern techniques. Revision rates were also lower, but it does not only reflect the great results of these early mold arthroplasties. A half century ago arthroplasty revision surgery results were not as good as nowadays, so surgeons had a higher threshold for performing it. Furthermore, patient expectations and needs were lower so they could settle with less than perfect results. This amount of limb shortening would make the outcome unacceptable to modern surgeons and patients. It is hard to explain why the above-mentioned prostheses stood the test of time. The Smith-Petersen mold arthroplasty does not seem to align with the current principles of hip replacement surgery, however, these cases demonstrated remarkable long-term results. We might never find an exact answer to this contradiction; nonetheless, we believe that the careful work of these pioneers of hip arthroplasty surgery contributed not only to the excellent results of these particular patients but also to the outstanding results of all current hip arthroplasty techniques. In our case, the acetabular erosion and the consequent limb shortening yielded a suboptimal clinical result, but the fact that the patient got 65 years of the relatively good function is noteworthy and is a tribute to Dr. Marius Nygaard Smith-Petersen.
Clinical Message
Excellent implant survivorship figures do not necessarily mean that an implant is excellent!
References
1. Smith-Petersen MN. Evolution of mould arthroplasty of the hip joint. J Bone Joint Surg Br 1948;30B(1):59-75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18864947. [Last accessed on 2016 Nov 10].1. Smith-Petersen MN. Evolution of mould arthroplasty of the hip joint. J Bone Joint Surg Br 1948;30B(1):59-75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18864947. [Last accessed on 2016 Nov 10].
2. Law WA, Manzoni A. Smith-Petersen mould arthroplasty of the hip: Results after 12-21 years. Proc R Soc Med 1970;63(6):583.
3. Mahalingam K, Reidy D. Smith-Petersen vitallium mould arthroplasty: A 45-year follow-up. J Bone Joint Surg Br 1996;78(3):496-497.
4. Baker JF, Vioreanu MH, Khan HA. Smith-Petersen vitallium mould arthroplasty: A 62-year follow-up. J Bone Joint Surg Br 2011;9B3(9):1285-1286.
5. Knight SR, Aujla R, Biswas SP. Total Hip Arthroplasty-over 100 years of operative history. Orthop Rev (Pavia) 2011;3(2):e16.
6. Hernigou P. Smith-Petersen and early development of hip arthroplasty. Int Orthop 2014;38(1):193-198.
7. Tennent TD, Eastwood DM. Survival of the Judet hip prosthesis. J R Soc Med 1998;91(7):385-386.
8. Judet R, Judet J. Technique and results with the acrylic femoral head prosthesis. J Bone Joint Surg Br 1952;34-B(2):173-180.
9. Denham RA, Law WA. Arthroplasty of the hip. J Bone Joint Surg Br 1957;39B(4):614-622. Available from: http://www.ncbi.nlm.nih.gov/pubmed/13491625. [Last accessed on 2016 Nov 10]
10. Radcliffe SN, Geary NP 46-year survival of a Smith-Petersen mold arthroplasty. J Arthroplasty 1997;12(5):584-585.
11. Wright DM, Alonso A, Rathinam M, Sochart DH. Smith-Petersen mould arthroplasty: An ultra-long-term follow-up. J Arthroplasty 2006;21(6):916-917.
12. Landham PR, Abbas N, Jähnich H. The oldest surviving arthroplasty? J R Soc Med 2006;99(12):640.
13. Northover JR, Maqsood M. 58-year follow-up of a vitallium mold hip arthroplasty: A case report and lit rev. Acta Orthop 2008;79(6):731-733.
 |
| Dr. Tamás Halasi |
| How to Cite This Article: Halasi T, Reidy D, Guerin S. Longest Known Follow-up of a Hip Arthroplasty: The Last Chapter of a 65-Year Long Story. Journal of Orthopaedic Case Reports 2017 May-June;7(3):76-79. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com