[box type=”bio”] Learning Points for this Article: [/box]
We report a case of severe genu valgum in Ellis-van Creveld syndrome using a two-step procedure, this technique allowed for the correction of the joint architecture and associated complications are minimal.
Case Report | Volume 7 | Issue 4 | JOCR July – August 2017 | Page 13-16 | Tomomi Kamada, Naohiko Mashima, Hiroshi Imai, Jun Takeba, Hiromasa Miura. DOI: 10.13107/jocr.2250-0685.828
Authors: Ravi Gupta[1], Anubhav Malhotra[1], Munish Sood[2], Gladson David Masih[1]
[1] Department of Orthopaedics, Government Medical College and Hospital, Chandigarh. India.
[2] Department of Orthopaedics, Trained in Arthroscopy Command Hospital, Chandi Mandir, Panchkula, Haryana, India.
Address of Correspondence
Dr. Ravi Gupta
Department of Orthopaedics, Sports Injury Centre, Government Medical College and Hospital, Chandigarh. India.
E-mail: ravikgupta2000@yahoo.com
Abstract
Introduction: Ellis-van Creveld syndrome (EVC) is a very rare genetic disorder involving a severe, relentlessly progressive genu valgum deformity of the knee and it is usually difficult to correct all of the deformities by elevation of the depressed lateral tibial plateau alone. We are reporting one such case treated using two-step operative technique (first, gradual correction using Taylor spatial frame (TSF) and second, tibia elevation through intra-articular osteotomy).
Case Report: We report a case of 10-year-old female with severe genu valgum in EVC using two-step operative technique. First, performing soft tissue release and gradual correction using a TSF. Second, tibia elevation through intra-articular osteotomy resulted in improved joint congruity. At final follow-up, the patient has a good functional result and the Mikulicz line proceeded physiologically to the joint center.
Conclusion: This two-step technique allowed for the correction of the joint architecture and associated complications are minimal. For severe genu valgum in EVC, joint congruity is improved by the elevation of the anterolateral aspect of the tibia through intra-articular osteotomy. Performing soft tissue release followed by gradual correction allows for correction of the valgus and external rotation deformities without causing neuroparalysis.
Keywords: Ellis-van Creveld syndrome, severe genu valgum, intra-articular osteotomy.
Introduction
Ellis-van Creveld syndrome (EVC) is a very rare genetic disorder involving a severe, relentlessly progressive genu valgum deformity of the knee [1, 2]. Only a few reports exist regarding operative correction of the knee deformity in EVC, many of which describe a bony realignment performed in one step using soft tissue release and extra-articular osteotomy [3, 4]. Herein, we report a case of genu valgum in EVC. Using a two-step procedure, we first performed a soft tissue release and gradual correction of the valgus and external rotation deformities using a Taylor Spatial Frame (TSF; Smith & Nephew Inc., Memphis, TN), followed by tibial hemiplateau elevation performed using intra-articular osteotomy.
Case Report
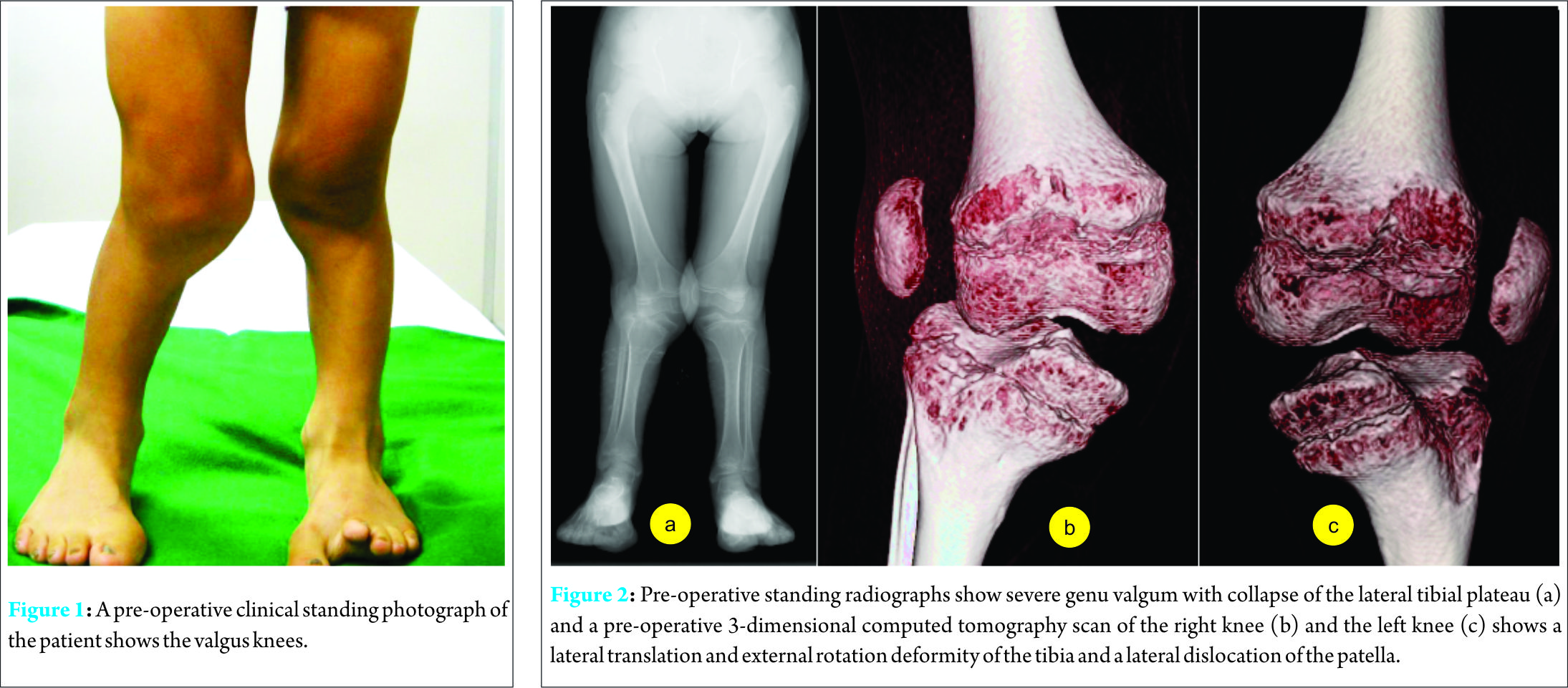
A 10-year-old female with severe bilateral genu valgum associated with EVC syndrome (Fig. 1) experienced gait disturbance and increasing right knee pain. On physical examination, the motion of the right and left knees ranged from 20° to 110° and from 10° to 130°, respectively. In addition, both patellae were dislocated laterally, and the medial knee showed substantial instability. Radiographic examinations of both knees, including a computed tomographic scan, showed genu valgum, lateral, and anterior depression of the proximal lateral tibial plateau, external rotation deformity of the lower leg, and lateral patellar dislocation (Fig. 2). The tibiofemoral angle of the right and left knees was 150° and 162°, respectively.
Surgical technique
Surgery was performed under general anesthesia with the patient in the supine position. The right knee had more severe pain, and thus, was operated on first. Correction was performed in three steps. In the first step, extensive soft tissue release was performed. In the second step, the valgus and external rotation deformities were gradually corrected using a TSF. In the third step, the lateral articular surface of the tibia was elevated using intra-articular osteotomy.
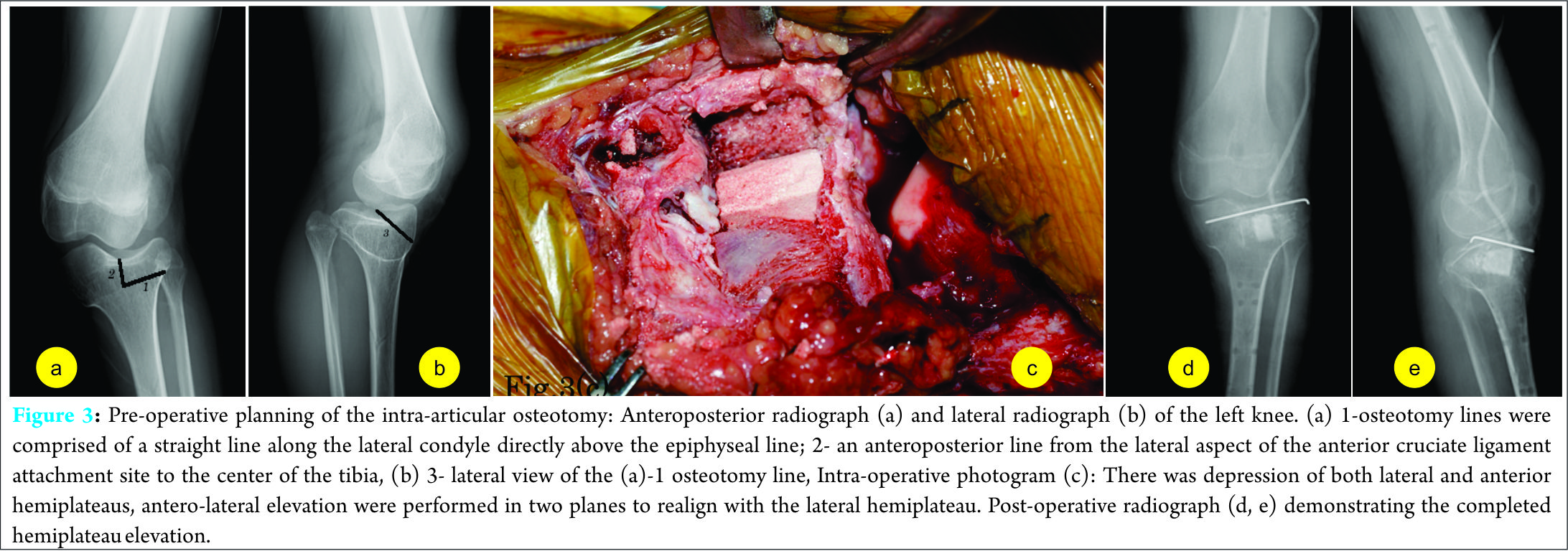
Initially, soft tissue release was performed. A typical, long curvilinear surgical incision measuring approximately 10 cm was made on the lateral aspect of the patella. Extensive release and mobilization of the quadriceps muscle, iliotibial band, lateral knee capsule, and the lateral retinaculum contracture were performed. Then, Z-plasty of the biceps tendon was performed to obtain reduction of the patella. Finally, TSF frames were fixated to the distal femur and proximal fibula across the knee joint with tensioned wires and half pins. The TSF was mounted such that the proximal ring master tab was aligned with the femoral trochlear notch in the anterior-posterior plane. The distal ring anti-master tab was centered over the mal-aligned tibial tubercle. After mounting the frame on the lower extremity, the mounting parameters were recorded and entered into TSF-dedicated computer software along with the deformity parameters. All corrections were made gradually after a latency phase of 4 days. The patient was instructed to perform gradual adjustments of the six struts of the TSF once per day. Correction was continued until the tibiofemoral angle was overcorrected to 180?, which occurred on the 7th week. After the completion of the correction, the external fixator was temporarily removed under general anesthesia, and intra-articular osteotomy was performed ( Fig.3 ). A skin incision was made at the same site as the previous operation. For the right knee, which had been operated on first, intraepiphyseal osteotomy was performed with image intensifier control because the physis was open. The osteotomy lines were comprised of a straight line along the lateral condyle directly above the epiphyseal line and an anteroposterior line from the lateral aspect of the anterior cruciate ligament attachment site to the center of the tibia. For the left knee, the physis was closed, thus osteotomy was performed distally during the same procedure. After the lateral plateau was sufficiently elevated in both frontal and sagittal planes, an appropriately sized bone graft was inserted. Tricortical bone harvested from the ilium was used for the right knee, and bone prosthesis was used for the left knee. Tricortical bone harvested from the ilium was used for the right knee, and a ß-tricalcium phosphate (ß-TCP) was grafted for the left knee. For postoperative fixation, an external fixator was used on the right side for 6 weeks, and an internal (Kirschner wire) and external fixation were used on the left side for 5 weeks. After the operation, partial weight-bearing was gradually permitted, and full weight-bearing was permitted at post-operative week 8th.
Follow-up
At a follow-up assessment, 4 years on the right side and 2 years on the left side from the each latest surgery, the patient was walking with a normal gait and no knee pain. Knee motion ranged from 0° to 100° on the right side, and from 0° to 120° on the left side. Post-operative long-leg weight-bearing radiographs and a simple radiograph showed correction of the valgus deformity. In the full standing Merchant view, the Mikulicz line proceeded physiologically to the joint center (Fig. 4). The tibiofemoral angle of the right and left knees was 174° and 172°, respectively.
Discussion
The current case demonstrates two important clinical issues. For severe genu valgum in EVC, joint congruity is improved by the elevation of the anterolateral aspect of the tibia through intra-articular osteotomy. Performing soft tissue release followed by gradual correction allows for correction of the valgus and external rotation deformities without causing neuroparalysis. These two points are each further discussed below. The articular surface of the left knee looks uneven in the radiograph compared with the right knee. It is due to an irregularity on the articular surface of the left knee because the left knee was operated on after the right knee. The difference in the type of the bone graft used also might have been a contributing factor. Since ß-TCP is softer than autologous bone, we suspect that the correction was slightly reversed after weight bearing was initiated.
Intra-articular osteotomy
In this case, tibia elevation through intra-articular osteotomy resulted in improved joint congruity. Many previously reported techniques involve correction by extra-articular osteotomy [3, 5, 6]. Because intra-articular osteotomy is technically demanding and has a potential complication of a propagation of the osteotomy into an intra-articular fracture. Intra-articular osteotomy performed for genu valgum in EVC has only been reported by Paley and Tetsworth [7] and Feldman et al. [8]. Feldman et al. [8] reported that intra-articular osteotomy performed to correct genu valgum in eight knees with lateral compartment deficiency achieved excellent clinical outcomes in all of the knees. The peculiar lateral sloping and depression of the lateral tibial plateau was present in all reported cases of EVC [4, 6, 9]. Furthermore, Weiner et al. [9] reported that proximal tibial deformities include not only a simple depression of the lateral aspect but also deformities of the proximal lateral tibial plateau slopes in a variable fashion including laterally forward or, to a lesser extent, posteriorly. Thus, extra-articular osteotomy does not restore the normal anatomy of the joint since the medial tibial plateau is relatively normal and the deformity is largely confined to the lateral tibial plateau. We believe that all the main deformities in EVC, including not only a lateral compression but also an anterior defect of the lateral tibial plateau, can be corrected by performing this osteotomy with great care.
Soft tissue release and gradual correction with TSF
In the current case, soft tissue release and gradual correction using TSF allowed for the correction of not only the valgus deformity of the knee joints but also the external rotation deformity and flexion contracture, which are difficult to correct by osteotomy alone, without causing neuroparalysis. Fukuda et al. [10] reported that the main cause of valgus deformity in EVC is depression of the lateral aspect of the tibial plateau and soft tissue tightness, including the fascia lata, lateral collateral ligament, biceps femoris, gastrocnemius, and capsule. Given that many reports exists regarding recurrence after osteotomy alone was performed to correct genu valgum in EVC [5], soft tissue contracture may be an important factor for the correction. Furthermore, soft tissue release results in decompression of the peroneal nerve, which avoids permanent nerve dysfunction secondary to acute valgus correction. Neurovascular complications have been reported to be as high as 20% after osteotomy of the tibia in children [11]. Acute correction of the bilateral femur deformity was performed with gradual correction of the tibiae, and the patient did not experience nerve palsy and achieved an almost normal mechanical axis.
Conclusions
Intra-articular osteotomy improved joint congruity in the current case involving severe genu valgum in EVC. By performing soft tissue release and gradual correction before osteotomy, both valgus and external rotation deformities were corrected without causing neuroparalysis. One limitation of this study is that it involved only one patient followed for a relatively short period of time. Additional primary assessments with longer follow-up periods are needed to assess the efficacy of this technique. While it is usually difficult to correct all of the deformities in severe genu valgum by elevation of the depressed lateral tibial plateau alone, our two-step technique allowed for the correction of the joint architecture and has resulted in a successful outcome.
Clinical Message
For severe genu valgum in EVC, this two-step correction technique was safety and allowed for the correction of the joint architecture. By performing soft tissue release and gradual correction before osteotomy, the valgus and external-rotation deformities could be corrected.
References
1. Avolio A Jr, Berman AT, Israelite CL. Ellis-van creveld syndrome (chondroectodermal dysplasia). Ortopedics 1994;17:735-7.1. Avolio A Jr, Berman AT, Israelite CL. Ellis-van creveld syndrome (chondroectodermal dysplasia). Ortopedics 1994;17:735-7.
2. Ellis RW, van Creveld S. A syndrome characterized by ectodermal dysplasia, polydactyly, chondro-dysplasia and congenital morbus cordis: Report of three cases. Arch Dis Child 1940;15(82):65-84.
3. Shibata T, Kawabata H, Yasui N, Nakahara H, Hirabayashi S, Nakase T, et al. Correction of knee deformity in patients with Ellis-van Creveld syndrome. J Pediatr Orthop B 1999;8(4):282-4.
4. Eylon S, Simanovsky N, Porat S. The pathology of valgus knee in Ellis-van – Creveld syndrome and its surgical treatment. Comparison to the equivalent pathogy in Blount’s disease. J Bone Joint Surg Br 2008;90-B Supp?:512.
5. Jöckel JA, Reichel H, Nelitz M. Correction of knee deformity in patients with Ellis-van Creveld syndrome: A case report and review of the literature. Knee 2012;19(3):218-22.
6. Morsy A, Tsuchiya H, Matsubara H, Kabata T, Tomita K. Ilizarov deformity correction of the lower limbs in Ellis-van Creveld syndrome. J Orthop Sci 2007;12(5):505-9.
7. Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Relat Res 1992;65-71
8. Feldman DS, Goldstein RY, Kurland AM, Sheikh Taha AM. Intra-articular osteotomy for genu valgum in the knee with a lateral compartment deficiency. J Bone Joint Surg Am 2016;98(2):100-7.
9. Weiner DS, Jonah D, Leighley B, Dicintio MS, Holmes Morton D, Kopits S. Orthopaedic manifestations of chondroectodermal dysplasia: The Ellis-van Creveld syndrome. J Child Orthop 2013;7(6):465-76.
10. Fukuda A, Kato K, Hasegawa M, Nishimura A, Sudo A, Uchida A. Recurrent knee valgus deformity in Ellis-van Creveld syndrome. J Pediatr Orthop B 2012;21(4):352-5.
11. Steel HH, Sandrow RE, Sullivan PD. Complications of Tibial osteotomy in children for genu varum or valgum. Evidence that neurological changes are due to ischemia. J Bone Joint Surg Am 1971;53(8):1629-35.
 |
 |
 |
 |
 |
| Dr. Tomomi Kamada | Dr. Naohiko Mashima | Dr. Hiroshi Imai | Dr. Jun Takeba | Dr. Hiromasa Miura |
| How to Cite This Article: Kamada T, Mashima N, Imai H, Takeba J, Miura H. Successful Two-step Correction for Severe Genu Valgum in Ellis-van Creveld Syndrome: A Case Report. Journal of Orthopaedic Case Reports 2017 July-Aug;7(4):13-16 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com