[box type=”bio”] Learning Points for this Article: [/box]
Aspergillus osteomyelitis, a rare condition with very high mortality rates and increased incidence in immunocompetent individuals, can have excellent clinical outcomes with appropriate cultures, antifungals, and surgical debridement where indicated.
Case Report | Volume 7 | Issue 4 | JOCR July – August 2017 | Page 62-65| Aditya Menon, Camilla Rodrigues, Rajeev Soman, Ayesha Sunavala, Vikas M Agashe. DOI: 10.13107/jocr.2250-0685.854
Authors: Aditya Menon[1], Camilla Rodrigues[2], Rajeev Soman[3], Ayesha Sunavala[3], Vikas M Agashe[1]
[1] Department of Orthopedics, P.D. Hinduja Hospital and Medical Research Centre, Mahim, Mumbai, Maharashtra. India.
[2] Department of Microbiology, P.D. Hinduja Hospital and Medical Research Centre, Mumbai, Maharashtra. India
[3] Department of Internal Medicine, P.D. Hinduja Hospital and Medical Research Centre, Mumbai, Maharashtra. India.
Address of Correspondence
Dr. Vikas M Agashe,
Department of Orthopaedics, P.D. Hinduja Hospital and Medical Research Centre, Veer Savarkar Marg, Mahim (West), Mumbai – 400016, Maharashtra. India.
E-mail: agashefam@gmail.com
Abstract
Introduction: Osteomyelitis is rarely caused by fungi, most common among them being Candida. Aspergillus is a rare cause of fungal osteomyelitis mimics tuberculous osteomyelitis. Aspergillus osteomyelitis (AO) of the ribs is relatively uncommon, with an incidence rate of only 9% among all reported cases of AO. With mortality rates of almost 25%, AO is on the rise attributed to increasing numbers of immunocompromised individuals. There are very few case reports of AO of ribs in immunocompetent individuals. We report two such cases.
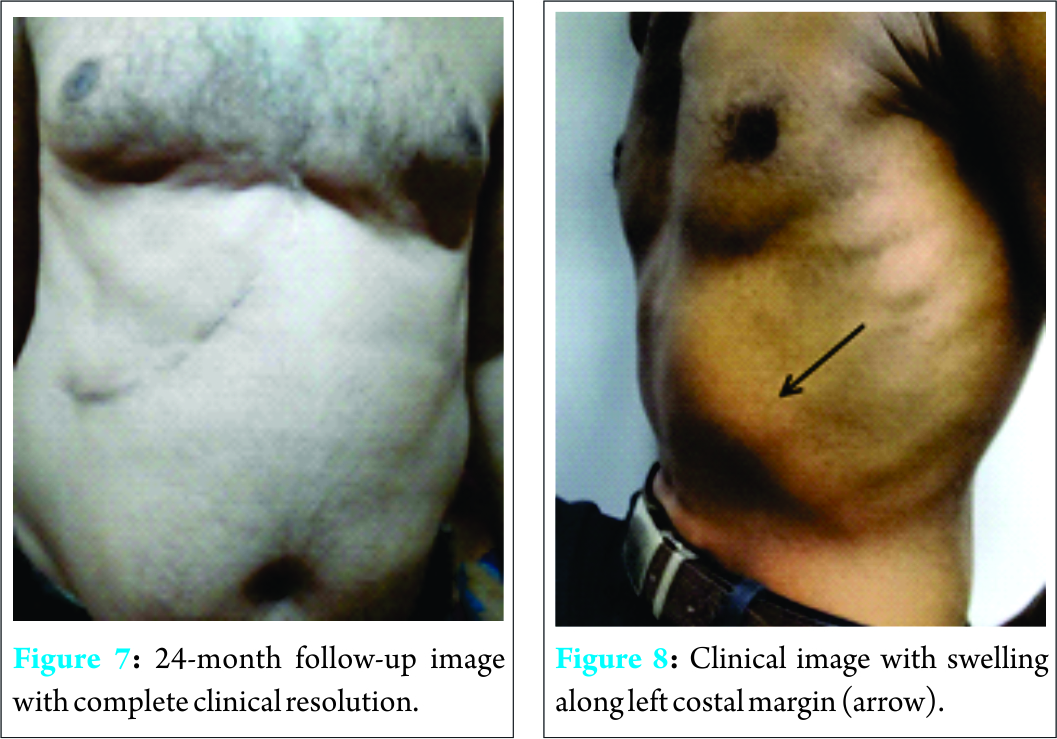
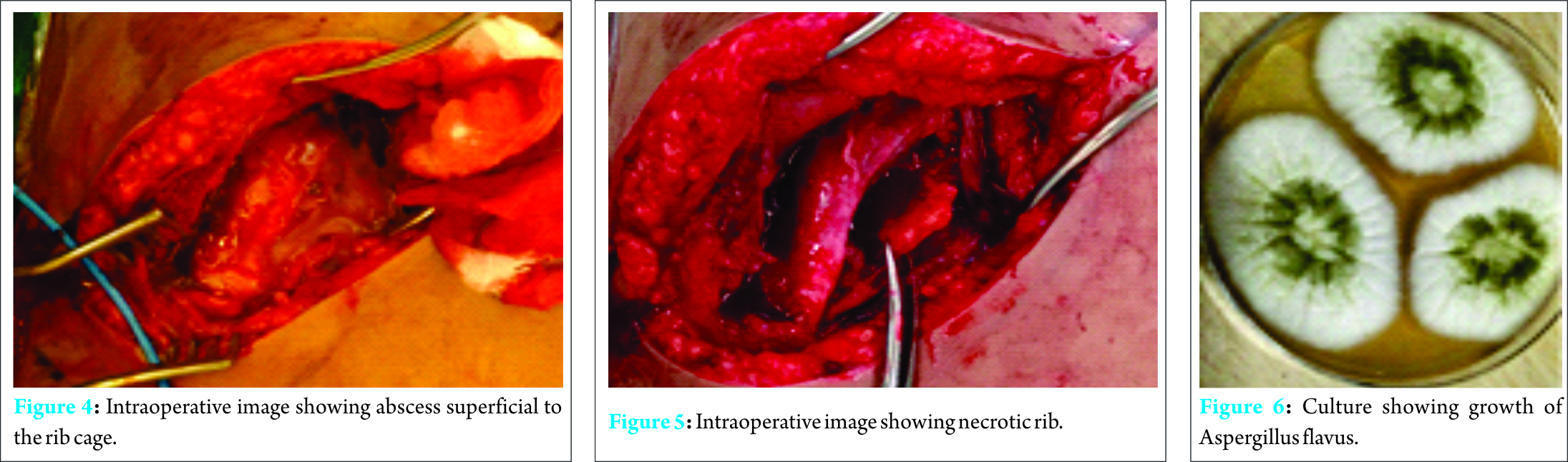
Case Report: Case 1: A 51-year-old male developed spontaneous chest pain along right costal margin with a low-grade fever. High-resolution computed tomography chest revealed osteomyelitis of anterolateral chest wall. He did not improve with empirical antitubercular therapy, and subsequent debridement showed polymicrobial pyogenic infection which was managed with appropriate antibiotics elsewhere. Samples were not sent for fungal culture. He presented to us 3 months later, and surgical debridement showed growth of Aspergillus flavus which was managed with oral voriconazole. The lesion healed with no recurrence at 24-month follow-up. Case 2: A 40-year-old male presented to our institute with left-sided chest pain, low-grade fever, and loss of appetite. There was a history of injury with a sharp piece of wood 2 years earlier. Magnetic resonance imaging defined the lesion which was biopsied under ultrasound guidance. Cultures grew A. flavus which was treated with oral voriconazole. He had complete clinical improvement at 16-month follow-up.
Conclusion: More number of AO cases are being reported in immunocompetent individuals. Variability in clinical picture, rarity, misdiagnosis, empirical therapy, and failure to send deep tissue samples for fungal cultures are some of the reasons for the high mortality rates. It is paramount in today’s scenario of atypical presentations, to obtain deep tissue for all cultures including fungal culture and histopathology, either surgically or under image guidance to achieve good clinical outcomes. Our study highlights that following the strict protocol of obtaining tissue for fungal culture, systemic antifungal therapy, and surgical debridement where necessary can help to diagnose and treat this rare pathology and ensure the good clinical outcome.
Keywords: Aspergillosis, immunocompetent host, rib osteomyelitis, fungal osteomyelitis.
Introduction
Osteomyelitis is rarely caused by fungi, most common among them being Candida [1]. Aspergillus, a ubiquitous saprophytic fungus, is a rare cause of fungal osteomyelitis with a reported incidence rate of <3% [2]. Aspergillosis most commonly involves the spine (49%), with clinical features resembling tuberculous osteomyelitis [3, 4]. Aspergillus osteomyelitis (AO) of the ribs is relatively uncommon, with an incidence rate of only 9% among all reported cases of AO [4]. The incidence of invasive aspergillosis, which has mortality rates of almost 25%, is on the rise attributed to increasing numbers of immunocompromised individuals coupled with increased survival rates afforded by newer therapeutic modalities [4, 5, 6]. There are very few case reports of AO of ribs in immunocompetent individuals [1, 7, 8]. We report two such cases of AO of the ribs in immunocompetent individuals.
Case Report
Case 1
A 51-year-old male developed spontaneous chest pain along right costal margin with low-grade fever. High-resolution computed tomography chest revealed an enhancing soft tissue with central necrotic area involving the right fifth, sixth, and seventh ribs and sternum suggestive of infective chondritis along with enlarged axillary lymph nodes. Needle biopsy of both the lesions done elsewhere showed no growth on bacterial culture with non-specific inflammatory changes on histopathology. Empirical antitubercular therapy was initiated and continued for 5 months in the same facility; however, the symptoms persisted. Subsequent debridement with a midline incision done elsewhere showed polymicrobial infection with Staphylococcus aureus and Klebsiella pneumoniae and was treated with appropriate antibiotics. Samples were not sent for fungal culture. He presented to us 3 months following debridement with excruciating pain and swelling of the right lower chest wall inspite of 8 weeks of appropriate antibiotics (Fig. 1). Magnetic resonance imaging (MRI) showed a large heterogeneous lesion along the right anterolateral chest wall and parasternal region involving the lower ribs and adjacent costal cartilage (Fig. 2 and 3).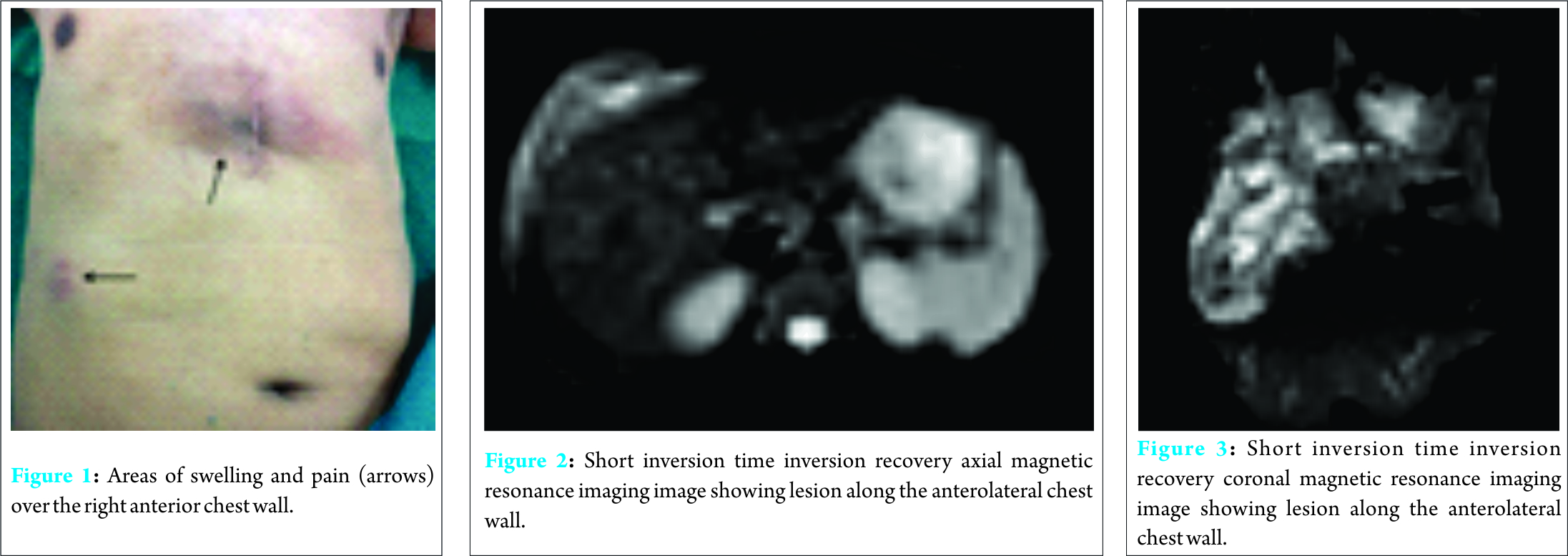
Case 2
A 40-year-old male presented to our institute with a history of left-sided chest pain in the lower part for 2 months. It was associated with intermittent episodes of low-grade fever and loss of appetite. There was a history of injury with a sharp piece of wood 2 years earlier; the patient being asymptomatic in the interim period. He did not have any of the traditional risk factors for Aspergillosis. On examination, he had a soft, tender swelling along the left costal margin extending up to the midaxillary line (Fig. 8).
MRI revealed a diffuse, ill-defined heterogeneous soft tissue swelling in the left anterior lower chest wall with focal areas of erosion/irregularity in the adjacent cartilage and costochondral junction. Suspecting an infective etiology, ultrasound-guided biopsy was done. Cultures grew septate fungal filaments of A. flavus. He was treated with oral voriconazole (200 mg) twice daily for 3 months. He had complete clinical improvement after the same at 16-month follow-up.
Discussion
AO is an extremely rare condition, Candida being the most commonly reported cause of fungal osteomyelitis [1]. Aspergillosis is known to affect immunocompromised individuals more often, and most commonly, individuals with chronic granulomatous disease, acute leukemias, human immunodeficiency virus infection, and solid organ transplant recipients, among others [1, 4, 5, 9, 10]. In developing countries like India, it is also seen in individuals with risk factors such as diabetes mellitus, malnutrition, old tuberculous cavities, and cardiac device implantations [11]. It affects individuals due to a defect in the host immunity, which may be congenital as is the case in chronic granulomatous disease, where an enzymatic defect affects the cell-mediated immunity, or acquired like in patients on chemotherapy, corticosteroids, or those with leukemias, diabetes, malnutrition, and old age [1, 12]. Gabrielli et al. [4], in a recent review of all the reported cases of AO in the literature, have highlighted the nature of this oft-neglected pathology. AO as a subset of its invasive form, though rare, has mortality rates of up to 25% [4, 5]. Delay in diagnosis is associated with high complication rates and disseminated infection. Due to the high incidence of tuberculous osteomyelitis in developing countries and fungal osteomyelitis clinically mimicking the former, there is a high chance of missing fungal osteomyelitis in the initial stages, especially in immunocompetent individuals unless proven by culture and histopathology. This and the slow, protracted natural history results in late diagnosis in most cases, for as long as 32 weeks [1]. A highly variable clinical picture with pain being the most common symptom and fever seen in only 20% of cases confounds the diagnostic dilemma [9]. This fact is highlighted in our first case, who did not improve inspite of 5 months of empirical antitubercular therapy. Subsequent surgical debridement and culture-specific antibiotics did not improve his clinical condition as fungal cultures were not obtained, thereby missing the primary pathology. We obtained ultrasound-guided samples in our second case and did not subject him to empirical antibiotics, avoiding a delay in getting a definitive diagnosis. This emphasizes the importance of obtaining cultures including fungal culture and histopathology for all cases irrespective of our clinical suspicion, as there is an increasing incidence of AO even in immunocompetent patients [9]. Gabrielli et al. [4] reviewed 310 cases reported in the literature till 2013. Of these, 49% were from the spine with only 9% of cases involving the ribs. Moreover, chest wall involvement is seen more often in the pediatric population, while both our patients were adults. Hematogenous involvement is seen in immunocompromised cases, whereas traumatic involvement and iatrogenic causes are seen more often in the immunocompetent ones [5]. Neither of our cases had any medical comorbidity. The chest injury with a sharp piece of wood causing a laceration in our second case could possibly have been a source of the infection. The most common species reported is Aspergillus fumigatus followed by A. flavus [1, 4, 5, 9, 11]. Both our cases grew A. flavus on fungal cultures. There are no strict therapeutic recommendations; a combination of surgical debridement to reduce the fungal burden along with a single or combination therapy of systemically active antifungals seems to be the best option though not statistically better than antifungals alone [4]. Amphotericin B is the most commonly used antifungal, although recent reports suggest that voriconazole has emerged as the drug having a maximum efficacy of all antifungals, with better results in combinations containing it than the ones which do not [4, 5]. Better results have been reported in those with direct inoculation (trauma, postsurgical) as compared to the ones with immunodeficiency, highlighting the role played by the host defense in combating AO [4].
Direct injury with a sharp piece of wood may have been the mode of entry in the second case. The good clinical outcome in both our cases could possibly be attributed to the absence of immunodeficiency or any other medical comorbidity, surgical debridement in the first case, and early diagnosis in the second.
Conclusion
Tuberculosis is one of the most common causes of osteomyelitis, especially in India and other developing countries. Fungal osteomyelitis, a relatively uncommon pathology, closely resembles tuberculous osteomyelitis. Aspergillosis, which commonly affects the lungs in immunocompromised patients, has been shown to involve the osteoarticular system even in immunocompetent patients. More number of AO cases are being reported, including those affecting the ribs and sternum which parallels the ever-increasing incidence of diabetes and elderly population. It is paramount in today’s scenario of atypical presentations, to obtain deep tissue culture, either surgically or under image guidance for bacterial, tubercular, fungal cultures, and histopathology to achieve good clinical outcomes. Variability in clinical picture, rarity, misdiagnosis, empirical therapy, and failure to send deep tissue samples for fungal cultures are some of the reasons for the high mortality rates associated with AO. Our study highlights that following the strict protocol of obtaining tissue for fungal culture, systemic antifungal therapy and surgical debridement where necessary can help diagnose and treat this rare pathology and ensure the good clinical outcome.
Clinical Message
Fungal osteomyelitis is a rare entity. Variable clinical presentation, slow progression, resemblance to tuberculous osteomyelitis, and rarity are all responsible for the delay in diagnosing these pathologies. AO has increased in numbers over the years, affecting immunocompetent individuals as well. Lack of awareness of this entity may deter an orthopedic surgeon from sending a sample for fungal cultures, apart from the usual bacterial and tuberculous cultures. This along with the other causes mentioned result in a very high mortality of almost 25% reported in these cases. Excellent clinical outcomes can be achieved with appropriate cultures, antifungals, and surgical debridement where indicated.
References
1. D’sa SR, Singh S, Satyendra S, Mathews P. Case report of Aspergillus osteomyelitis of the ribs in an immunocompetent patient. J Glob Infect Dis 2013;5(3):118-120.1. D’sa SR, Singh S, Satyendra S, Mathews P. Case report of Aspergillus osteomyelitis of the ribs in an immunocompetent patient. J Glob Infect Dis 2013;5(3):118-120.
2. Frazier DD, Campbell DR, Garvey TA, Wiesel S, Bohlman HH, Eismont FJ. Fungal infections of the spine. Report of eleven patients with long-term follow-up. J Bone Joint Surg Am 2001;83-A(4):560-565.
3. Winterstein AR, Bohndorf K, Vollert K, Wagner T, Gnekow A, Roemer FW. Invasive aspergillosis osteomyelitis in children-A case report and review of the literature. Skeletal Radiol 2010;39(8):827-831.
4. Gabrielli E, Fothergill AW, Brescini L, Sutton DA, Marchionni E, Orsetti E, et al. Osteomyelitis caused by Aspergillus species: A review of 310 reported cases. Clin Microbiol Infect 2014;20(6):559-565.
5. Koehler P, Tacke D, Cornely OA. Aspergillosis of bones and joints-a review from 2002 until today. Mycoses 2014;57(6):323-335.
6. McNeil MM, Nash SL, Hajjeh RA, Phelan MA, Conn LA, Plikaytis BD, et al. Trends in mortality due to invasive mycotic diseases in the United States, 1980-1997. Clin Infect Dis 2001;33(5):641-647.
7. Salloum A, Rao S, Havasi A, Miljkovic G, Amoateng-Adjepong Y. Aspergillus rib and vertebral osteomyelitis in a former intravenous drug user. Am J Med 2004;116(3):208-209.
8. Ranjan R, Mishra S, Ranjan S. Aspergillus vertebral osteomyelitis in an immunocompetent person. Neurol India 2010;58(5):806-808.
9. Gamaletsou MN, Rammaert B, Bueno MA, Moriyama, B, Sipsas NV, Kontoyiannis DP, et al. Aspergillus osteomyelitis: Epidemiology, clinical manifestations, management, and outcome. J Infect 2014;67:478-493.
10. Dotis J, Roilides E. Osteomyelitis due to Aspergillus species in chronic granulomatous disease: An update of the literature. Mycoses 2011;54:e686-e696.
11. Chakrabarti A, Chatterjee SS, Das A, Shivaprakash MR. Invasive Aspergillosis in developing countries. Med Mycol 2011;49 Suppl 1:S35-S47.
12. Tack KJ, Rhame FS, Brown B, Thompson RC Jr. Aspergillus osteomyelitis. Report of four cases and review of the literature. Am J Med 1982;73(12):295-300.
 |
 |
 |
 |
 |
| Dr. Aditya Menon | Dr. Camilla Rodrigues | Dr. Rajeev Soman | Dr. Ayesha Sunavala | Dr. Vikas M Agashe |
| How to Cite This Article: Menon A, Rodrigues C, Soman R, Sunavala A, Agashe VM. Aspergillus Osteomyelitis of the Ribs in Immunocompetent Hosts: Report of Two Rare Cases. Journal of Orthopaedic Case Reports 2017 Jul-Aug;7(4):62-65 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com