[box type=”bio”] Learning Points for this Article: [/box]
Absent pain reporting does not preclude a fracture, and patient mobility must be considered when choosing the appropriate fixation construct.
Case Report | Volume 7 | Issue 5 | JOCR September – October 2017 | Page 7-10| George J M Hourston, Hadyn K N Kankam, Phillip Johnston. DOI: 10.13107/jocr.2250-0685.874
Authors: George J M Hourston [1], Hadyn K N Kankam [1], Phillip Johnston [1]
[1] Department of Orthopaedics, University of Cambridge, School of Clinical Medicine, Addenbrooke’s Hospital, Hills Road, Cambridge CB2 0SP, UK.
Address of Correspondence
Mr. Phillip Johnston,
Department of Orthopaedics, University of Cambridge, School of Clinical Medicine, Addenbrooke’s Hospital, Hills Road, Cambridge CB2 0SP, UK.
E-mail: phillip.johnston@addenbrookes.nhs.uk
Abstract
Introduction: Stress fractures are more common in the weight-bearing bones of the lower limb and are particularly prevalent in athletes. Whereas, those of the upper limb are usually reported as unique events in rare circumstances.
Case Report: We present a case of a 40-year-old White British female with neuromyelitis optica (NMO) who mobilized in a wheelchair and presented to our center in April 2016 with a week-long history of a hot, swollen, and unstable right forearm. Plain radiographs demonstrated fractures of both the radius and ulna of the dominant right arm. These were managed by open reduction and internal fixation to facilitate mobility and transfer using the forearm. Intraoperatively, these were confirmed to be fatigue fractures, and there was evidence that the fracture was several days old. The neurological deficit in this patient had led to a delayed presentation owing to the lack of pain. Unfortunately, this construct failed within 8 days, and a refixation was performed 2 months later. 1 year following the revision, no further problems have been reported, and there has been satisfactory union.
Conclusion: This is the first report in the published literature of a stress fracture in a patient with NMO. We recommend screening for stress fractures with a nuclear bone scan in patients who mobilize in atypical ways, particularly if their sensation is compromised. The use of constructs stronger than those routinely applied to the upper limb should also be considered if patients are weight bearing through their arms.
Keywords: Neuromyelitis optica, stress fracture, forearm fracture.
Introduction
Stress fractures, first described by Breithaupt in 1855 [1], are small cracks in bone caused by repetitive activity and microtrauma, with each injury alone being insufficient to cause an acute fracture. Such fractures caused by abnormal stresses on normal bone are more specifically known as fatigue fractures. Stress fractures and specifically fatigue fractures are usually found within athletes because of the repeated minor injuries that they sustain in their repetitive training and performance. More commonly, these are reported in the weight-bearing bones of the lower limb [2, 3]. As the physicality of various sports which involve recurrent use of the arm, such as tennis, has developed, so has the incidence of these fatigue fractures in the upper limb [4, 5, 6]. However, they are still relatively uncommon and rare outside of sports medicine. Neuromyelitis optica (NMO) has been identified as a central nervous system autoimmune inflammatory disorder and is thought to be a B cell-mediated humoral immune disease. NMO is a heterogeneous condition consisting of both inflammation and demyelination of the optic nerve (optic neuritis) and the spinal cord (myelitis). The international panel for NMO diagnosis defines the unifying term NMO spectrum disorders (NMOSDs), which is stratified further by serologic testing (NMOSD with or without aquaporin-4 immunoglobulin G [AQP4-IgG]). The core clinical characteristics required for patients with NMOSD with AQP4-IgG include clinical syndromes or magnetic resonance imaging findings related to optic nerve, spinal cord, area postrema, other brainstem, diencephalic, or cerebral presentations [7, 8]. To the best of our knowledge, the combination of this surgical presentation set against this neurological background has never been published.
Case Report
Presentation and diagnosis
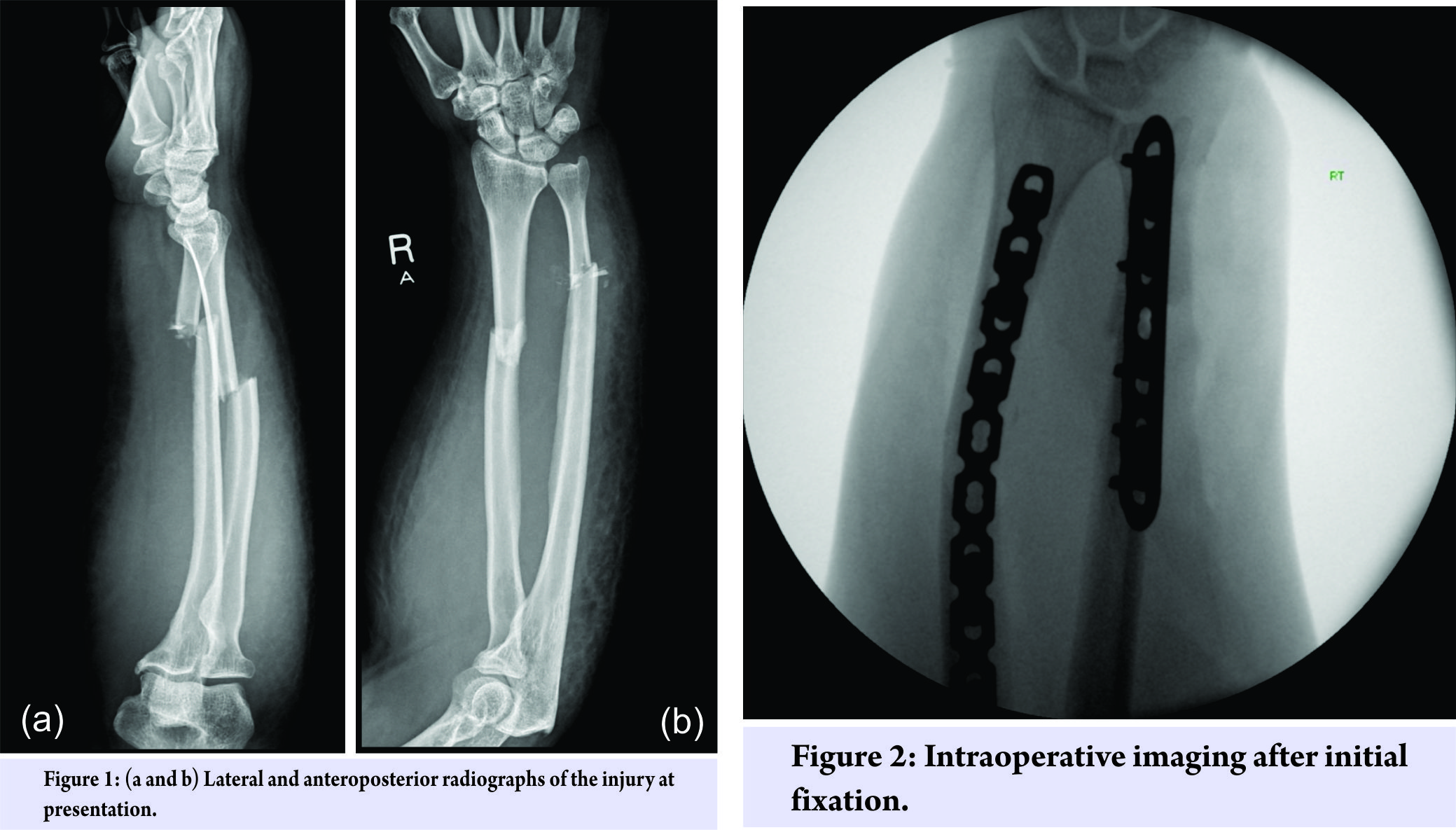
A 40-year-old White British female who mobilized in a wheelchair due to NMO presented to the emergency department in our center with a swollen, hot, painless right forearm. This patient had no current evidence of optic neuritis. She was treated with rituximab, a monoclonal antibody directed against the CD20 antigen. The arm had been in this condition for 8 days, and the patient had taken antibiotics for what was presumed to be an infection. However, the forearm gradually worsened, leading to deformity and instability. After clinical evaluation, the forearm was placed in a cast, and a plain radiograph X-ray was taken to investigate bone fracture (Fig. 1). Comminuted fractures through the mid-radius and ulna were confirmed, and a significant soft-tissue swelling was also noted. Diagnoses considered for her symptoms were cellulitis, stress fractures of the radius and ulna, and pathological fractures of the radius and ulna due to malignancy or osteoporosis. Once instability was clinically evident, the presence of a fracture became obvious. Although this did not exclude the possibility of infection, the C reactive protein and white blood cell count were not suggestive of this differential. It was only after samples of bone were examined histologically that the presence of a malignancy was excluded. The presence of osteoporosis could not be completely excluded without a dual-energy X-ray absorptiometry bone density scan. However, since this patient was not on steroidal therapy for NMO but rather a biologic drug and given her young age, osteoporosis was deemed unlikely. This patient was pre-menopausal with a regular cycle and had no gynecological history of note. Stress fractures of the radius and ulna were the diagnosis most consistent with her symptoms, imaging, and histology.
Treatment and follow-up
Since the patient was dependent on her upper limb to mobilize and transfer weight, we felt that it was important to stabilize the forearm contrary to usual practice. Therefore, the patient was listed for an open reduction and fixation of both the radius and ulna. Intraoperatively, the radial fracture was found to be simple with little comminution. A ten-hole locking compression plate was selected with a reasonable working length and then contoured to respect the radial bow. The ulnar fracture was found to be comminuted with rounding of the fracture ends, suggesting that this had been partially fractured for some time, indicative of a fatigue fracture. Fixed-angle (locking) plates on both radius and ulna were used to minimize the risk of construct failure through implant cut-out, about which the patient would be unaware owing to her lack of sensibility in the arm.Bone samples from the fracture site were sent for histology to exclude malignancy, although this seemed unlikely from the macroscopic appearance of the fracture site. Further, the distal radioulnar joint was found to be stable, and the radiographs (Fig. 2) were satisfactory.
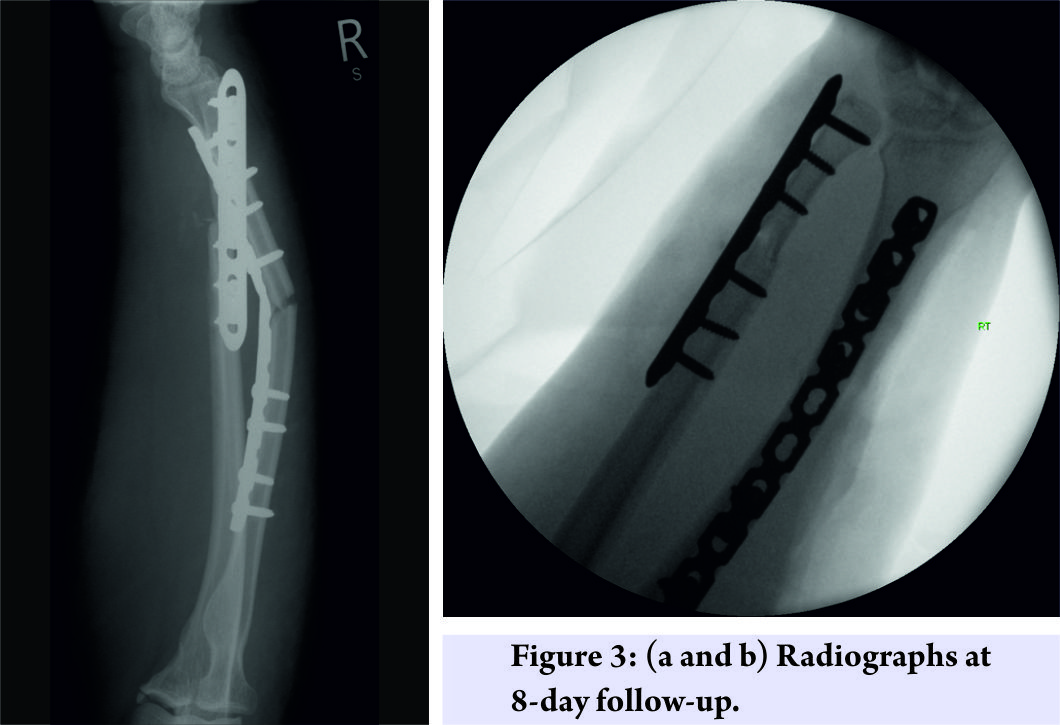
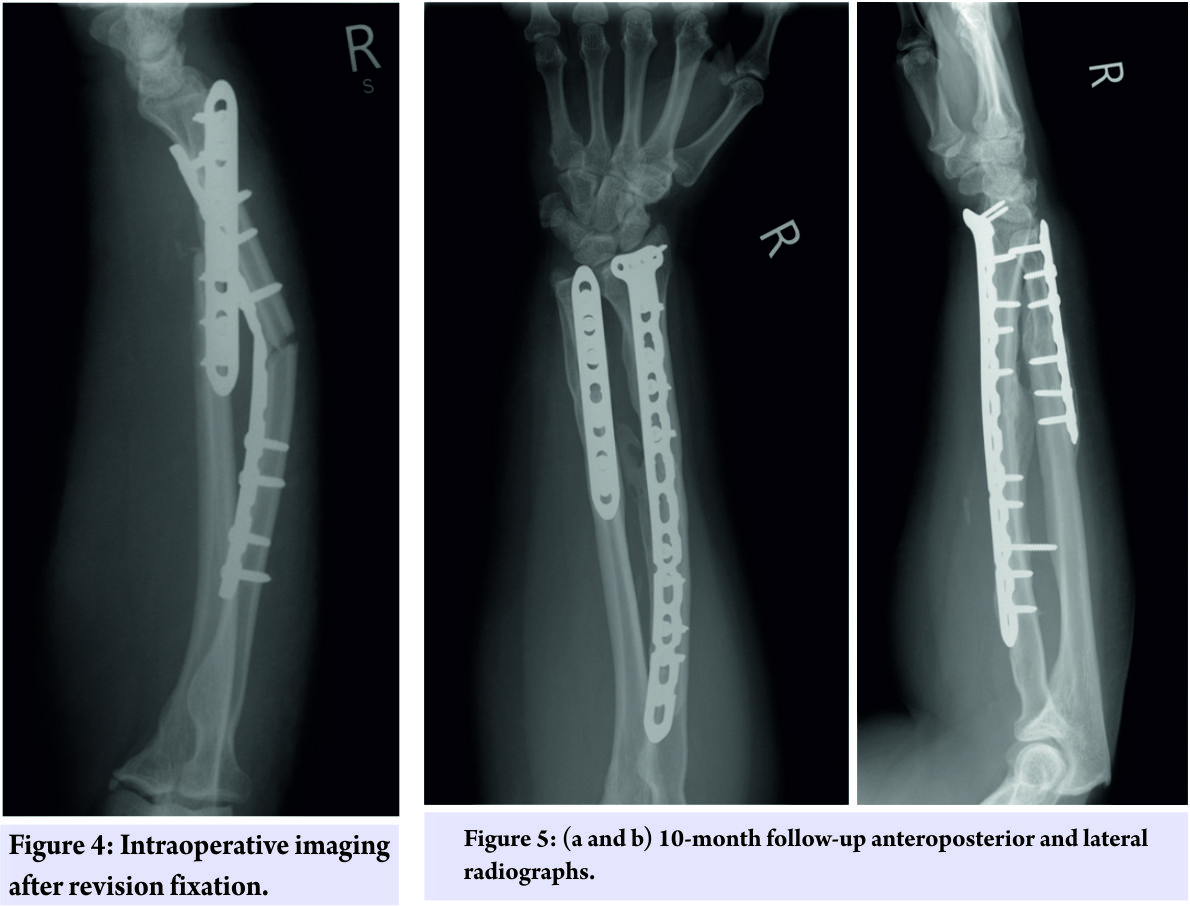
Despite fracture fixation, it was found in the initial follow-up clinic, 8 days later, that the construct had failed. Radiographs showed that the radial plate had flexed and the deformity was approximately 30° (Fig. 3). Both wounds had also dehisced, due to the tension, they were under post-operatively. 5 weeks later, after satisfactory wound healing, a stronger bespoke radial plate was ordered, and the construct failure was successfully revised. The new construct was an eleven plus four hole volar rim plate pre-contoured into extension at the fracture site. It was protected in the immediate post-operative period with external casting in addition to the internal fixation (Fig. 4). 10 months after the revision, the patient has reported no further problems, the X-rays are progressing to union satisfactorily, and the patient has a good range of movement including forearm rotation despite heterotopic ossification in the interosseous membrane (Fig. 5).
Discussion
Stress fractures are rare in the upper limb and are usually observed in sports medicine [9]. The occurrence of such a fracture in a patient weight bearing through the upper limbs in the context of a neurological deficit has, to the best of our knowledge, never been published before. Stress fractures, particularly those of the upper limb, are most often managed with “active rest.” The goals in this period are described by the acronym representational state transfer and include removal of the abnormal stress; exercise to maintain fitness; safe return to the previous level of activity; and time to allow for complete bone remodeling [10]. In this case, the patient needed to use her arms to effectively mobilize and transfer from her wheelchair. It was therefore essential that we achieved adequate stability of the fractured forearm to maintain her quality of life and independence. This case was unusual from the presentation through to the initial treatment and in terms of the follow-up treatment that was required as this patient was asensate. Initially, the presence of a fracture was not apparent clinically owing to of the lack of pain. Post-operatively, the patient would not feel pain from an incipient compartment syndrome and so a more thorough clinical examination including demonstrating active finger movements was required. Subsequently, the stability we needed to achieve in the forearm was greater than first expected because the patient needed to weight bear through her arms but would be unaware if the construct had failed.
Conclusion
We would recommend screening for stress fractures with a nuclear bone scan if there is any clinical suspicion of such an injury in patients who mobilize in atypical ways. Furthermore, we have found that the plating systems regularly used for forearm shaft fractures in adults may not be sufficient to bear the weight of patients who mobilize exclusively with their arms. It is our plan in the future to use stronger constructs as the first line management in fracture fixation for such patients lacking sensibility in any weight-bearing limbs.
Clinical Message
The absence of pain reporting does not exclude fracture diagnosis. Screening for stress fractures may be appropriate in patients who cannot report pain. Commonly used plating systems for forearm fractures may not be appropriate if the patient weight bears through the upper limb.
References
1. Astur DC, Zanatta F, Arliani GG, Moraes ER, Pochini Ade C, Ejnisman B. Stress fractures: Definition, diagnosis and treatment. Rev Bras Ortop 2015;51:3-10.1. Astur DC, Zanatta F, Arliani GG, Moraes ER, Pochini Ade C, Ejnisman B. Stress fractures: Definition, diagnosis and treatment. Rev Bras Ortop 2015;51:3-10.
2. Sanderlin BW, Raspa RF. Common stress fractures. Am Fam Physician 2003;68:1527-32.
3. Kahanov L, Eberman LE, Games KE, Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med 2015;6:87-95.
4. Jones GL. Upper extremity stress fractures. Clin Sports Med 2006;25:159-74.
5. Li X, Heffernan MJ, Mortimer ES. Upper extremity stress fractures and spondylolysis in an adolescent baseball pitcher with an associated endocrine abnormality: A case report. J Pediatr Orthop 2010;30:339-43.
6. Meena S, Rastogi D, Solanki B, Chowdhury B. Stress fracture of ulna due to excessive push-ups. J Nat Sci Biol Med 2014;5:225-7.
7. Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG. Revised diagnostic criteria for neuromyelitis optica. Neurology 2006;66:1485-9.
8. Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 2015;85:177-89.
9. Miller TL, Kaeding CC. Upper-extremity stress fractures: Distribution and causative activities in 70 patients. Orthopedics 2012;35:789-93.
10. Romani WA, Gieck JH, Perrin DH, Saliba EN, Kahler DM. Mechanisms and management of stress fractures in physically active persons. J Athl Train 2002;37:306-14.
 |
 |
 |
| Mr. George Hourston | Mr. Hadyn Kankam | Mr. Phillip Johnston |
| How to Cite This Article: Hourston GJM, Kankam HKN, Johnston P. Radius and Ulna Stress Fractures in a Patient with Neuromyelitis Optica: A Case Report. Journal of Orthopaedic Case Reports 2017 Sep-Oct ; 7(5): 7-10. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com