[box type=”bio”] Learning Point for this Article: [/box]
Tuberculosis of a joint can present in an unusual form and always needs to be suspected in all confusing clinical situations.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 80-84 | Rajiv Shah, Shyam Patel, Shivam Shah. DOI: 10.13107/jocr.2250-0685.1010
Authors: Rajiv Shah[1], Shyam Patel[2], Shivam Shah[2]
[1]Department of Orthopaedics, Baroda Hospital, Vadodara, Gujarat, India, 2Department of Orthopaedics, S. S. G. Hospital & Baroda Medical College, Vadodara, Gujarat, India.
Address of Correspondence:
Dr. Rajiv Shah,
Director, Foot & Ankle Orthopaedics, Baroda Hospital, Anant Apartment, Tilak Road, Vadodara, Gujarat, India.
E-mail: rajivortho@gmail.com
Abstract
Introduction: A case of seronegative variety of subtalar joint arthritis was treated with subtalar joint fusion surgery. In spite of perfect execution of surgery, fusion did not occur. It was only at a revision surgery that case could be diagnosed as a case of tuberculosis of subtalar joint.
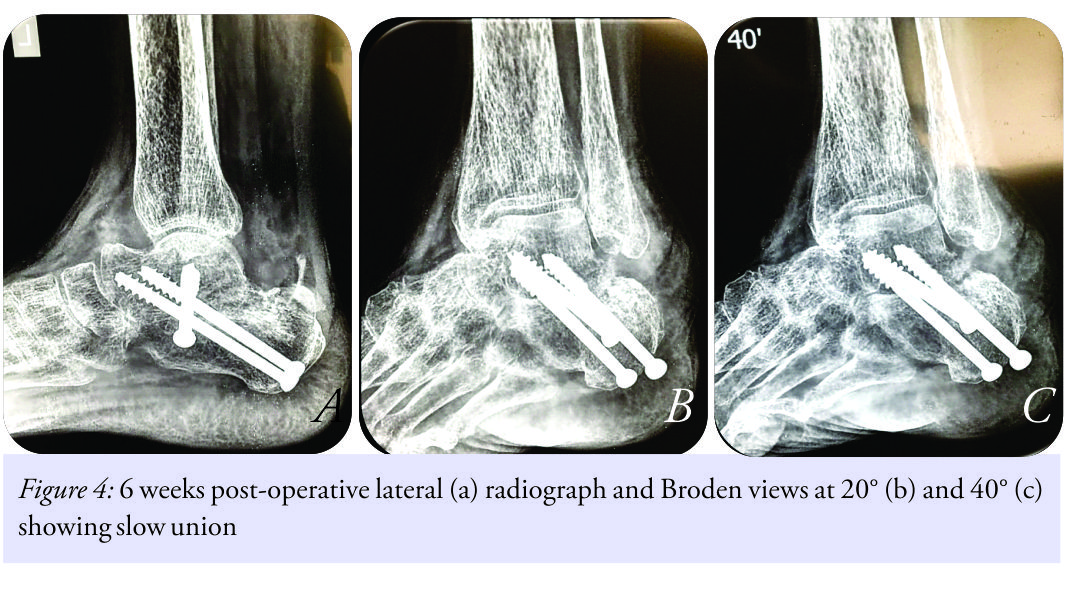
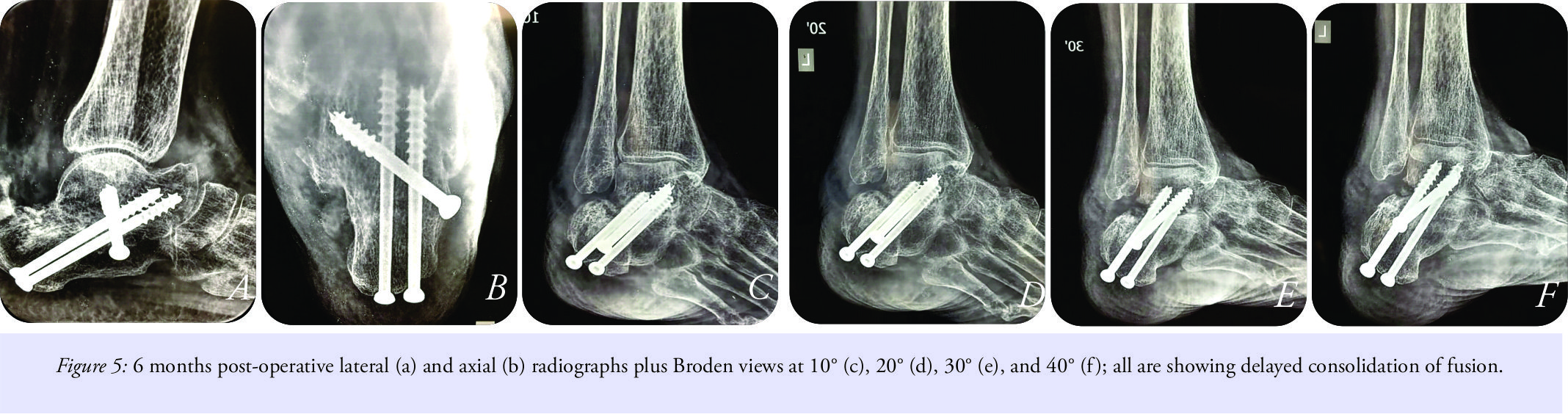
Case Report: Elderly female was operated for seronegative subtalar joint arthritis with fusion plus primary bone grafting. Fusion did not progress in spite of every added efforts such as extended immobilization, calcium supplements, and antibiotic therapy. Revision surgery was undertaken considering the reason of failure being a low-grade infection. At a revision surgery, case was diagnosed as a case of tuberculosis of subtalar joint, a very rare presentation. Fusion succeeded just with addition of antituberculous therapy supported with short-term immobilization.
Conclusion: Tuberculosis of the foot and ankle joints, though are rare, they can mimic like many other disorders. In developing countries, a high index of suspicion is warranted to early diagnose it.
Keywords: Subtalar joint, fusion, antituberculous treatment.
Introduction
Trauma, flat foot, and serological disorders are the common etiologies for arthritis of subtalar joint. The treatment for end-stage subtalar joint arthritis is in the form of fusion of joint [1]. Fusion of subtalar joint has a success rate of more than 80–90% [1, 2]. Failure of subtalar joint fusion is treated with revision surgery, fixation plus bone grafting [1, 2]. We present a case of subtalar arthritis treated with fusion, where fusion failed because of the fact that tuberculosis was the primary etiology giving rise to subtalar arthritis, though tuberculous affection of subtalar joint is rare.
Case report
A 66-year-old female presented with chief complaints of progressively worsening pain in the left ankle with inability to stand or walk, more so while walking over uneven surfaces for the past 8 months. On detailed history taking, no other specific positive points such as trauma, pain in other joints, or any constitutional symptoms were found. Clinical examination revealed diffuse tender horseshoe-shaped swelling all around subtalar joint with markedly restricted, painful subtalar joint movements. Her X-rays revealed a reduction of subtalar joint space with generalized osteoporosis (Fig. 1a and b). 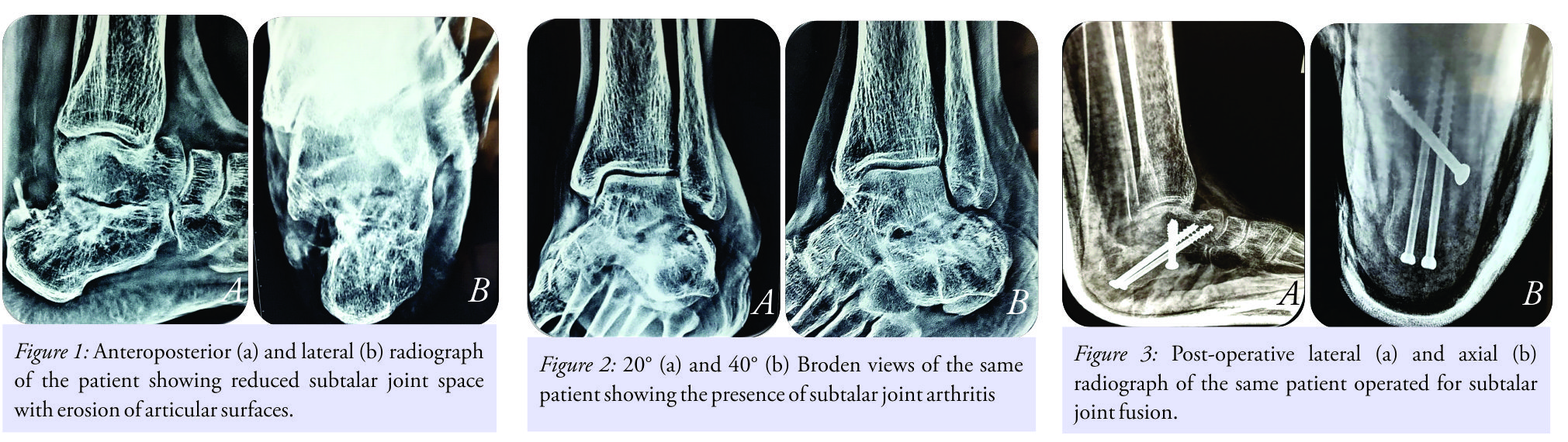
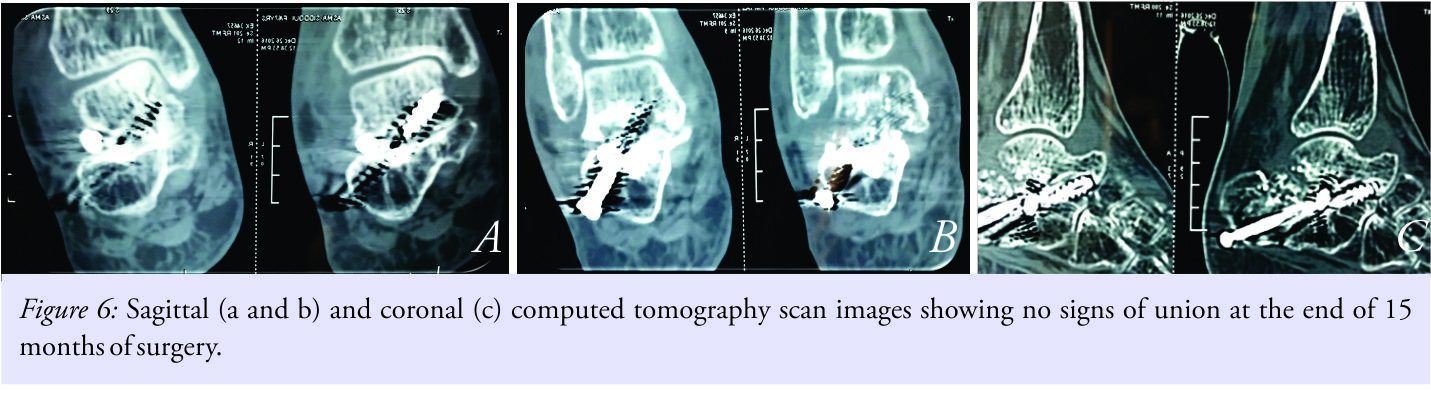
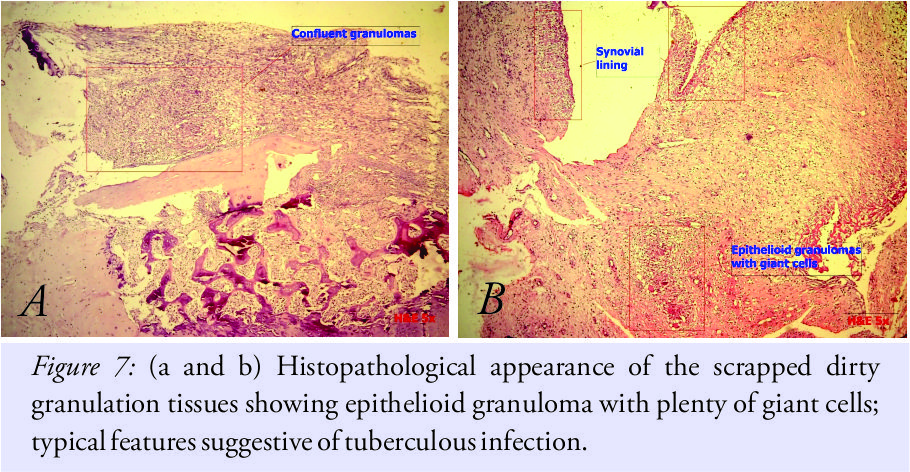
Considering this as a case of non–union plus infection, it was decided to go for two staged surgical interventions, where first stage was planned as removal of implants and debridement and the second stage as revision fusion after a course of antibiotics. At second surgery through the same approach, implants were removed. Fusion was found to be incomplete. No pus discharge was noticed. Dirty granulation tissues were scrapped from the fusion site, and material was sent for histopathology examination. Postoperatively, the patient was immobilized in anterior and posterior below knee plaster splints. The same broad-spectrum intravenous antibiotics were continued. Histopathologic examination showed epithelioid granulomas with plenty of giant cells suggestive of tuberculosis (Fig. 7a and b).
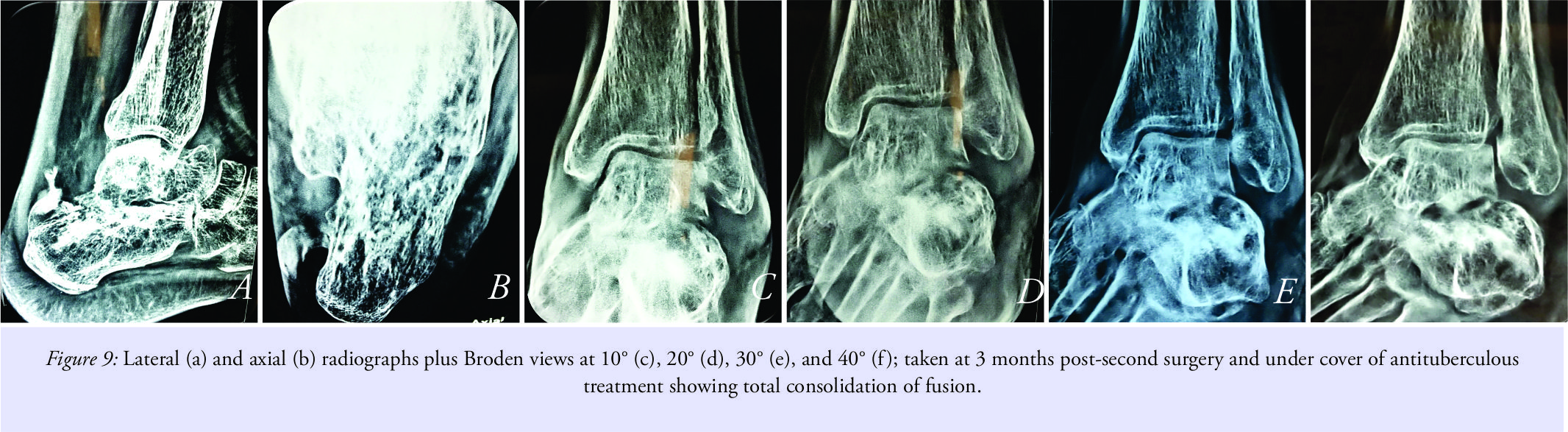
This was of a great surprise as the patient had no previous history of tuberculosis or any constitutive symptoms such as fever, night-pains, weight loss, or loss of appetite. The samples were reviewed at two other laboratories which also confirmed the diagnosis of tuberculosis. Antituberculosis treatment was started and the patient was given rest in the same below knee splint for 6 more weeks. Plan was to do revision fusion after 6 weeks under cover of antituberculous drugs. Serology showed improvement and so was patient. X-rays showed signs of fusion, and hence, surgery was delayed (Fig. 8a and b).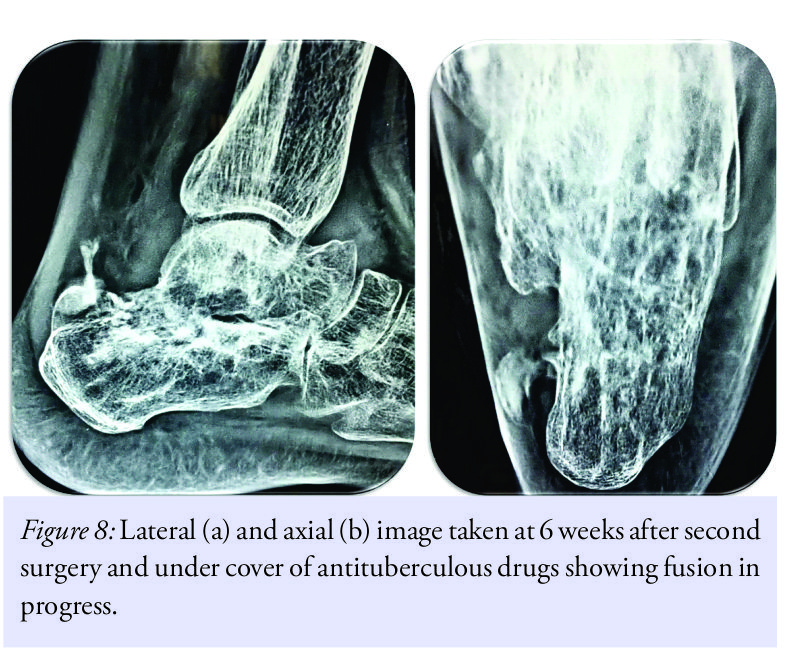
Discussion
Like other foot and ankle joints, subtalar joint does develop arthritis. The arthritis of subtalar joint could be either primary, degenerative, post-traumatic or following acquired flat foot deformity. Rheumatoid disease and other seronegative arthritides may also involve subtalar joint [1]. Initial treatment of subtalar joint arthritis is conservative in the form of rest, drugs, and activity modification [1, 2]. Failure of conservative care is an indication for fusion of subtalar joint [1, 2, 3]. Most commonly fusion of only posterior facet of subtalar joint is carried out [3]. Fusion of all three facets, anterior, middle as well as posterior was advised for difficult situations like post-traumatic subtalar arthritis by Mann et al. [2]. This is carried out with preparations of all subtalar joints plus addition of anterior screw from calcaneus to the neck of the talus. The reported non-union rates for subtalar fusion vary from 5% to 45%. In the largest study of 184 cases, Easely et al. showed union rate up to 84% [2]. The common reasons for failure of subtalar fusion were documented to be the presence of avascular bone at fusion site, smoking and presence of adjacent ankle fusion [1, 2, 3]. Treatment for such failures is in the form of revision fusion with structural bone grafting and addition of fixation [1, 2, 3]. Tuberculosis of bone and joints is a rare entity (10–15%) in comparison to pulmonary tuberculosis (75–90%) [4]. Tuberculosis of the foot and ankle is very rare and it comprises of 0.13% of total extra-pulmonary tuberculosis cases [4]. The bone and joint tuberculosis is characterized by systemic plus local signs and symptoms. Systemic signs and symptoms are in the form of fever, loss of weight, and loss of appetite with night pains. Local signs and symptoms include marked spasm, swelling, pain at rest, and tenderness with painful restrictions of movements and wasting [4, 5]. In the present case of established subtalar arthritis, failure of conservative care was addressed by fusion. In the present case of old-aged postmenopausal female, for successful fusion, all three, anterior, middle, and posterior facets of subtalar joint were fused with addition of anterior screw over and above two standard posterior screws fixing calcaneus body and talus neck. Looking at osteoporosis and the age of the patient, bone grafts were also added. Every efforts for getting successful end result were made, and still, there was failure of fusion. Failure of fusion was initially thought to be because of osteoporosis, and teriparatide was added and immobilization was prolonged. Later on, it was postulated that a low-grade infection could be the reason for failure, though the serological investigations were indeterminate. Chemotherapy with extended immobilization administered to combat low-grade infection also did not work. Magnetic resonance imaging could have given further insight into the reason for failure of fusion, but it was not possible due to the presence of metallic implants. Exploration, implant removal, and curettage were thought to be the last helping procedure for managing failure of fusion in the present case. Tuberculosis of subtalar joint as a reason of non-union was never thought because of the absence of typical systemic as well as local signs and symptoms of disease and rarity of location. It was only when implant removal and debridement of fusion area were done that histopathological study of retrieved material showed the presence of tuberculosis. To the best of our knowledge, in a perfectly executed subtalar fusion procedure, failure of fusion due to the presence of tuberculosis of subtalar joint and absence of typical signs and symptoms of tuberculosis has not been reported till date. The established method of care for tuberculosis of joints in the form of antituberculous drugs, rest in functional position and supportive therapy, succeeded in our case. In India, pulmonary tuberculosis is the most common (75–90%) form of tuberculosis. Rate of involvement of foot and ankle joints is 1–5% of all osteoarticular tuberculosis cases. Most commonly tuberculosis, in foot and ankle, involves calcaneus, talus, first metatarsal, and navicular [4, 6, 7, 8]. With the absence of typical signs and symptoms, tuberculosis of the foot and ankle mimics like many other pathologies and hence is often misdiagnosed [4, 5, 6, 7, 8]. In developing countries, tuberculosis of foot and ankle postulates a challenge in diagnosis and must always be suspected, more so in failure cases. We submit that in developing countries like India, only a high index of suspicion for tuberculosis can only help clinician. For all complex situations, tuberculosis must strike to clinician as a key culprit.
Conclusion
From the present case report, we suggest that, in developing countries, clinician should have a high index of suspicion for tuberculosis as a prime reason for joint fusion failures. Tuberculosis can be noticed even at the rare locations like subtalar joint without supportive signs, symptoms, and investigations.
Clinical Message
Message from this article will stimulate a lateral thinking among clinicians to always think and rule out tuberculosis in many confusing bone and joint problems.
References
1. Easely ME, Trnka HJ, Schon LC, Myerson MS. Isolated subtalar arthrodesis. J Bone Joint Surg Am 2000;82:613-24.
2. Mann RA, Beaman DN, Horton G. Isolated subtalar arthritis. Foot Ankle Int 1988;19:511-19.
3. Russotti M, Cass JR, Johnson KA. Isolated talocalcaneal arthrodesis. J Bone Joint Surg Am 1988;70:1472-78.
4. Tuli SM. Tuberculosis of the Skeletal System. 4th ed. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd.; 2010. p. 131-9.
5. Jeevan P, Anup S, George JP. A case of chronic inflammation of the ankle joint with subtle signs of inflammation: A rare presentation of tuberculosis ankle. J Orthop Case Reports 2017;7:87-90.
6. Dhillon MS, Aggarwal S, Prabhakar S, Bachhal V. Tuberculosis of the foot: An osteolytic variety. Indian J Orthop 2012;46:206-11.
7. Dhillon MS. Nagi on: Tuberculosis of the foot and ankle. Clin Orthop Relat Res 2002;398:107-13.
8. Anand A, Sood LK. Isolated tuberculosis of talus without ankle and subtalar joint involvement. Med J Malaysia 2002;57:371-3.
 |
 |
 |
| Dr. Rajiv Shah | Dr. Shyam Patel | Dr. Shivam Shah |
| How to Cite This Article: Shah R, Patel S, Shah S. Unusual Presentation of Tuberculosis of Subtalar Joint. Journal of Orthopaedic Case Reports 2018 Jan-Feb;8(1):80-84. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com