[box type=”bio”] Learning Point for this Article: [/box]
This report has added a novel mutation variant in the TBX4 gene in association with small patella syndrome which may contribute to early genetic diagnosis in childhood and thus following adequate surgical treatment.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 85-88| Tomoyuki Oda, Masaki Matsushita, Yohei Ono, Hiroshi Kitoh, Tadahiro Sakai. DOI: 10.13107/jocr.2250-0685.1012
Authors: Tomoyuki Oda[1], Masaki Matsushita[2], Yohei Ono[2], Hiroshi Kitoh[2], Tadahiro Sakai[1]
[1]Department of Orthopaedic Surgery, Toyota Memorial Hospital, Toyota, Japan.
[2]Department of Orthopaedic Surgery, Nagoya University Graduate School of Medicine, Showa-Ku, Nagoya, Japan.
Address of Correspondence:
Dr. Tadahiro Sakai, Department of Orthopaedic Surgery, Toyota Memorial Hospital, 1-1 Heiwa-cho, Toyota, 471-8513, Japan.
E-mail: nirmalpatil2008@gmail.com
Abstract
Introduction: Small patella syndrome (SPS) is a rare skeletal dysplasia relating to the T-box protein 4 (TBX4) gene, which regulates the development of lower extremities. Patients typically present with recurrent patellar dislocation (RPD) in childhood or adolescence, leading to a diagnosis of SPS and subsequent treatment to improve activity levels. However, those with mild symptoms may not be diagnosed when young and present later after skeletal maturation, which might compromise treatment options. Further understanding of genetic mutations of SPS could possibly help early diagnosis and following adequate surgical treatment. In this case report, we present a surgically treated adult female case of RPD associated with SPS, carrying a novel heterozygous mutation in the TBX4 gene.
Case Report: A 19-year-old female presented with persistent right knee pain after an atraumatic episode of patellar dislocation during walking. The patient had a history of recurrent patella instability of the right knee with an onset at the age of 8 years due to a minor trauma. Patellar apprehension sign was positive bilaterally. There was radiological evidence of bilateral small patellae, hypoplastic femoral trochlea, and tibial tuberosity. A direct sequencing of the coding regions in the TBX4 gene had confirmed the diagnosis of SPS. A novel heterozygous mutation (p.L39PfsX35) was found in the patient and her father. Surgical treatment was indicated and the patient underwent an isolated medial patellofemoral ligament (MPFL) reconstruction while no distal realignment osteotomy was performed due to hypoplastic tibial tuberosity. Excellent subjective and objective outcomes were obtained at 1 year postoperatively.
Discussion: To the best of our knowledge, this is the first reported SPS case with a novel mutation in the TBX4 gene in an Asian population. While a satisfying short-term outcome was obtained by an isolated MPFL reconstruction, early genetic diagnosis in childhood with adequate surgical treatment (e.g., Roux–Goldthwait procedure) would be ideal considering the limited treatment options in skeletally matured patients. The reported case has added one mutation variant of the TBX4 gene, which may help prevent delays in diagnosis of SPS.
Keywords: Small patella syndrome, T-box protein 4, recurrent patellar dislocation, mutation variant, hypoplastic tibial tuberosity, medial patellofemoral ligament reconstruction.
Introduction
Small patella syndrome (SPS) is a rare autosomal-dominant disorder affecting skeletal structures of the lower limb and pelvis. Essential features for the clinical diagnosis of SPS include patellar aplasia or hypoplasia and absent, delayed, or irregular ossi?cation of the ischiopubic junctions. In addition, a wide space between the ?rst and second toes (sandal gap) and flatfoot are other major signs [1]. Patients typically present with associated recurrent patellar dislocation (RPD) in their childhood or adolescence leading to an initial diagnosis of SPS [2] followed by surgical treatment (e.g., Roux–Goldthwait procedure [3]) to improve their activity levels. However, some with minimum pain even with existing RPD may be diagnosed later after skeletal maturity, which might compromise treatment options. Early diagnosis with adequate treatment is ideal given that remodeling of femoral sulcus can be expected with patella reduction and stabilization before skeletal maturity [4]. Meanwhile, Bongers et al. reported in their series of SPS cases, the associated heterozygous mutations in the transcription factor-encoding T-box protein 4 (TBX4) gene, which plays a crucial role in the developmental pathways of the lower limbs and the pelvis [5]. The authors identified six different mutations in the TBX4 gene in five families and one sporadic individual with SPS in European populations. More recently, the same group has reported 23 cases of SPS in the article discussing the association between TBX4 mutations and child-onset pulmonary arterial hypertension, while some cases were from the same families reported in the initial study [6]. However, little is known about the detailed mechanism of this disease and mutation variances. Further understanding of genetic mutations of SPS would help early diagnosis and adequate surgical treatment. In this case report, we present a surgically treated Japanese adult female case of RPD associated with SPS, carrying a novel heterozygous mutation in the TBX4 gene.
Case presentation
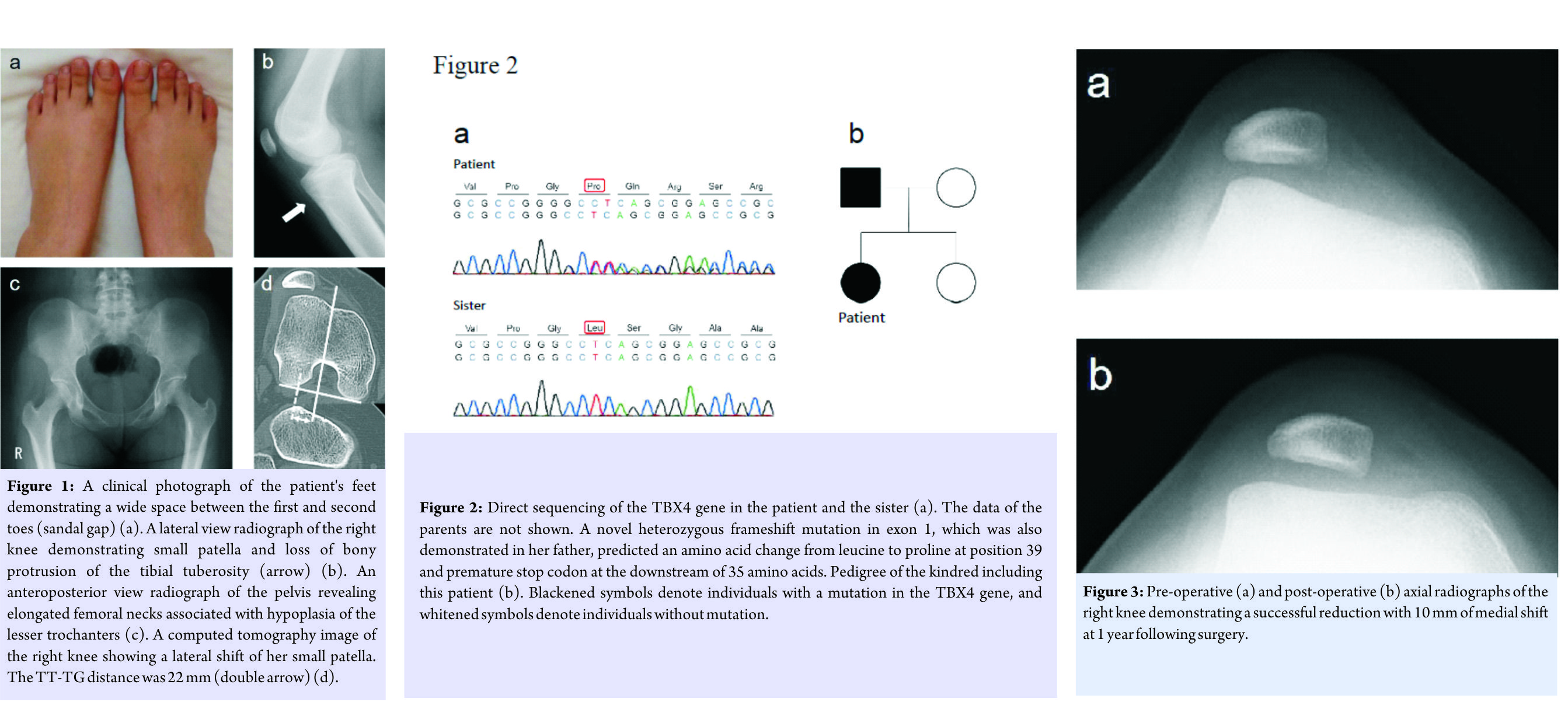
A 19-year-old Japanese female presented with persistent right knee pain after an atraumatic episode of patellar dislocation during walking. Patient had a previous history of right recurrent patella instability with an onset at the age of 8 years due to minor trauma. Mild genu valgum and genu recrurvatum were observed, along with a positive patellar apprehension sign, bilaterally. Flatfeet and sandal gaps were apparent (Fig. 1a). No facial anomalies or nail deformities were observed. Plain radiographs revealed bilateral small patella, hypoplasia of the tibial tuberosity (Fig. 1b), and elongated femoral necks with hypoplastic lesser trochanters (Fig. 1c). Computed tomography images of the right knee revealed a patellar subluxation associated with hypoplasia of the femoral trochlea groove, where the tubercle-trochlear groove (TT-TG) distance was 22 mm (Fig. 1d). After informed consent was obtained from the patient and her family members, mutation analysis of the coding regions in the TBX4 gene was performed. Genomic DNAs purified from peripheral blood of the patient and saliva of the family members (i.e. parents and sister) were assessed by direct sequencing using the QIAamp DNA Blood Midi kit (Qiagen, Inc., Valencia, CA)[7]. A novel heterozygous frameshift mutation (p.L39PfsX35) in exon 1 of the TBX4 gene, was found in the present case (Fig. 2a). Analyses of the parents and sister revealed that the TBX4 variant was derived from her father, who had neither medical history of skeletal dysplasia nor restricted activities of daily living (Fig. 2b).
Since conservative management (i.e. rest, analgesics, physiotherapy, brace, etc.) was not successful, surgical treatment was indicated for worsening pain in the right knee due to RPD. Under general anesthesia, a lateral retinacular release was performed arthroscopically, followed by open medial patellofemoral ligament (MPFL) reconstruction. The semitendinous tendon was harvested from the ipsilateral knee, and both ends of the tendon graft were then prepared with a running baseball stitch using a No.2 FiberWire (Arthrex, Naples, FL). The femoral bone tunnel was established according to the method reported by Schöttle et al. [8], where one end of the graft was passed through and fixed with an EndoButton (Smith & Nephew, London, England). Due to the small size of patella, transosseous graft fixation was not attempted for the patellar side considering a risk of fracture. Therefore, the other end of the graft was subperiosteally passed through one-third of the proximo-medial patella, and fixed onto the lateral aspect of the patella using braided nylon sutures with the knee in 90° of flexion. Distal realignment osteotomy (e.g. Elmslie-Trillat procedure) was not indicated because of the hypoplastic tibial tuberosity with no prominence. Postoperative course was uneventful. No recurrent pain or instability have been reported and maintained reduction of the patella has been radiographically confirmed at one year following surgery (Fig. 3a, b).
Discussion
In the current report, we presented a Japanese adult female case with a diagnosis of SPS. To the best of our knowledge, this is the first reported SPS case in an Asian population possessing a novel heterozygous mutation in the TBX4 gene. Following clinical and genetic diagnosis, the patient underwent an isolated MPFL reconstruction with a satisfying outcome. Typical manifestations, such as patellar hypoplasia, radiological anomalies of the pelvis, and sandal gap, have been reported to present in 100%, 89%, and 76% of SPS patients, respectively [1]. The present case, however, lacked characteristic radiological anomalies of the pelvis. In addition, relatively mild symptoms in childhood might have prevented the patient from early diagnosis, resulting in undergoing a surgery after skeletally matured. Furthermore, her father demonstrated no signs of the disease irrespective of carrying the same mutation. While a frameshift mutation identified in this case is predicted to lead to a truncated protein at exon 2 of the TBX4 gene, the presented milder phenotype than typical SPS cases could be due to haploinsufficiency of the mutant protein. Currently, only several mutations in the TBX4 gene have been reported in association with SPS [6]. However, SPS patients with no or minimum patella instability may not have difficulties in day-to-day activities, like the current case in her childhood or her father. Therefore, presumably, there could be quite a few underdiagnosed patients with SPS. Wang et al. recently reported 12 cases of SPS with satisfactory outcomes following medial and lateral retinaculum plasty for congenital patellar dislocation, although these cases were not genetically diagnosed [2]. Interestingly, while a majority of these cases were diagnosed and operated before their teenage years, there was one case of 31-year-old female included who suffered unilateral patellar dislocation, whereas the other patella presented in the groove [2]. The present case underwent an isolated MPFL reconstruction for RPD with a satisfactory short-term outcome at 1 year postoperatively. When an MPFL reconstruction is performed for RPD, the tendon graft is typically fixed to the patella through the bony tunnel [9]. However, we chose to apply suture technique for the extremely small patella to prevent adverse events such as patellar fracture by drilling. In addition, Dejour et al. recommended that Elmslie-Trillat procedure should be added in the cases with a TT-TG distance of more than 20 mm [10]. In the current case, while the TT-TG distance was over 20 mm, distal bony realignment procedure was not performed considering technical difficulties in performing osteotomy of non-prominent hypoplastic tibial tuberosity. Careful pre-operative planning is necessary in the treatment of RPD for SPS patients, particularly when operated after skeletal maturity, with special attention to the hypoplastic patella and tibial tuberosity. However, even though the current case has experienced no recurrent pain or recurrent instability for a short-term, it is not clear whether this isolated soft tissue reconstruction surgery can provide a successful long-term outcome without causing further recurrent instability and/or patellofemoral osteoarthritis in the future. While a satisfying outcome may be obtained by soft-tissue procedures even for adult patients, early clinical and genetic diagnosis in childhood with following adequate surgical treatment (e.g., Roux–Goldthwait procedure) would be ideal considering the limited surgical options in skeletally matured patients. We have provided additional genetic information for SPS in the hope of further understanding of SPS leading to earlier diagnosis particularly for the patients with milder symptoms.
Conclusions
This case report presented an adult SPS case successfully treated with an isolated MPFL reconstruction, and a novel mutation variant in the TBX4 gene in association with SPS has been reported. While a satisfying outcome may be obtained by surgical treatment even for adult SPS patients, early clinical and genetic diagnosis in childhood followed by adequate surgical treatment would be ideal.
Clinical Message
This report has added a novel mutation variant in the TBX4 gene in association with SPS, which may contribute to early genetic diagnosis in childhood and thus follow adequate surgical treatment.
References
1. Bongers EM, Van Bokhoven H, Van Thienen MN, Kooyman MA, Van Beersum SE, Boetes C, et al. The small patella syndrome: Description of five cases from three families and examination of possible allelism with familial patella aplasia-hypoplasia and nail-patella syndrome. J Med Genet 2001;38:209-14.
2. Wang CH, Shu L, Ma LF, Zhou JW, Ji G, Wang F, et al. Medial and lateral retinaculum plasty for congenital patellar dislocation due to small patella syndrome. Orthopedics 2013;36:e1418-23.
3. Goldthwait JE. V. Permanent dislocation of the patella. The report of a case of twenty years’ duration, successfully treated by transplantation of the patella tendons with the tubercle of the tibia. Ann Surg 1899;29:62-8.
4. Beals RK, Buehler K. Treatment of patellofemoral instability in childhood with creation of a femoral sulcus. J Pediatr Orthop 1997;17:516-9.
5. Bongers EM, Duijf PH, van Beersum SE, Schoots J, Van Kampen A, Burckhardt A, et al. Mutations in the human TBX4 gene cause small patella syndrome. Am J Hum Genet 2004;74:1239-48.
6. Kerstjens-Frederikse WS, Bongers EM, Roofthooft MT, Leter EM, Douwes JM, Van Dijk A, et al. TBX4 mutations (small patella syndrome) are associated with childhood-onset pulmonary arterial hypertension. J Med Genet 2013;50:500-6.
7. Matsushita M, Kitoh H, Kaneko H, Mishima K, Kadono I, Ishiguro N, et al. A novel SOX9 H169Q mutation in a family with overlapping phenotype of mild campomelic dysplasia and small patella syndrome. Am J Med Genet A 2013;161A:2528-34.
8. Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 2007;35:801-4.
9. Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C, et al. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 2012;40:1916-23.
10. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 1994;2:19-26.
 |
 |
 |
 |
 |
| Dr. Tomoyuki Oda | Dr. Masaki Matsushita | Dr. Yohei Ono | Dr. Hiroshi Kitoh | Dr. Tadahiro Sakai |
| How to Cite This Article: Oda T, Matsushita M, Ono Y, Kitoh H, Sakai T. A Novel Heterozygous Mutation in the T-box Protein 4 Gene in an Adult Case of Small Patella Syndrome. Journal of Orthopaedic Case Reports 2018 Jan-Feb;8(1):85-88. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com