[box type=”bio”] Learning Point for this Article: [/box]
The Complete or Near-Complete Functional Recovery for complex elbow dislocation depends on a good physical examination, a good cooperation, a good radiological research and assessment, a good-planned surgery, and a proper rehabilitation.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 15-17 | Erdem Yunus Uymur, Ahmet Köse, Sultan Tuna Akgöl Gür, Recep Dinçer, Murat Topal. DOI: 10.13107/jocr.2250-0685.978
Authors: Erdem Yunus Uymur[1], Ahmet Köse[1], Sultan Tuna Akgöl Gür[2], Recep Dinçer[1], Murat Topal[1]
[1]Department of Orthopedics and Traumatology, Region Research and Education Hospital, Erzurum, Turkey.
[2]Department of First Aid and Emergency Clinic, Region Research and Education Hospital, Erzurum, Turkey.
Address of Correspondence:
Dr. Erdem Yunus Uymur,
Department of Orthopedics and Traumatology, Region Research and Education Hospital, Erzurum, Turkey.
E-mail: tb9bmd@yahoo.com.tr
Abstract
Introduction: We wished to present a case that had elbow posterolateral dislocation accompanying complete medial collateral ligament rupture(MCLR) and complete flexor group origo rupture (FGOR) without fracture.
Case Report: A 30-year-old man came to emergency department after falling on the outstretched palm. After first physical examination and radiologic searches, elbow joint posterolateral dislocation was diagnosed. Together with sedoanalgesia, elbow dislocation was reduced, and instability evaluation by applying varus and valgus stress tests was performed. Positive valgus stress test and palpation sign which indicated soft tissue damage on the medial side of elbow were determined. Control roentgenograms showed no osseous pathology. By magnetic resonance imaging, elbow dislocation diagnosis accompanying MCLR and FGOR without fracture was confirmed. Using medial approach, ruptured MCL and elbow FGO repairing procedures were performed.
Conclusion: The complications of elbow dislocation without fracture, which is barely seen, should be treated through appropriate treatment strategies after meticulous physical examination and radiologic evaluation. Hence, possible sequelae could be prevented or satisfactory results could be obtained.
Keywords: Elbow dislocation without fracture, flexor group origo rupture, medial collateral ligament rupture.
Introduction
Elbow joint anatomically consists of radiohumeral, ulnohumeral, and proximal radioulnar joints. Its passive stabilizators are joint capsule and ligaments among medial collateral ligament (MCL) and lateral collateral ligament (LCL). Its active stabilizators are muscular groups that have connections as periarticular origins and insertions. Elbow is the second most dislocated joint in adults. Elbow periarticular fractures are coexisted with 1/5 of the patients [1]. For simple dislocations, closed reduction and conservative treatment are adequate. When olecranon, coronoid process, radial head fracture, and LCL rupture accompany, it is defined as complex dislocation. Open reduction and internal fixation and ligament repairing are required for the treatment [2]. For seldom cases, MCL repairing or external fixation should be done. For this case, instable elbow dislocation without fracture was present. Surgical treatment was decided because of detecting flexor group origo rupture (FGOR) that accompanies MCL rupture (MCLR) through magnetic resonance imaging (MRI) examination, which had not been reported until now.
Case report
A 30-year-old man came to emergency department after falling on the outstretched palm. On the first examination, elbow deformation and elastic fixation were present. Neurovascular deficit was not detected. Closed reduction was applied on the emergency conditions to the patient who was diagnosed asulnohumeral and radiohumeral convergent posterolateral dislocation without fracture by elbow antero-posterior (A-P) and lateral radiographs (Fig. 1).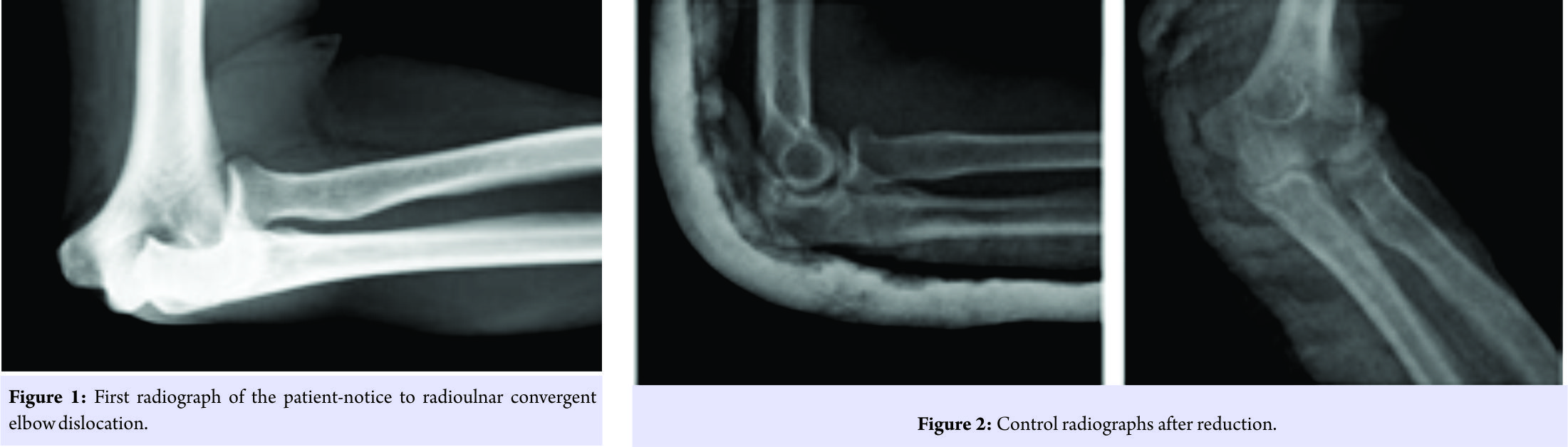 While sedo-analgesia was continuing after reduction (Fig. 2), soft tissue swelling was detected by palpation on the medial side of elbow. Valgus stress test was positive. By palpation, finger sign at the FGO-soft tissue depression at the medial side of elbow-was detected (Fig. 3). After control radiographs, no osseous pathology was found. Due to finger sign, to make separative diagnosis about FGOR, MRI was applied. On MRI images, MCLR and FGOR were observed (Fig. 4).
While sedo-analgesia was continuing after reduction (Fig. 2), soft tissue swelling was detected by palpation on the medial side of elbow. Valgus stress test was positive. By palpation, finger sign at the FGO-soft tissue depression at the medial side of elbow-was detected (Fig. 3). After control radiographs, no osseous pathology was found. Due to finger sign, to make separative diagnosis about FGOR, MRI was applied. On MRI images, MCLR and FGOR were observed (Fig. 4).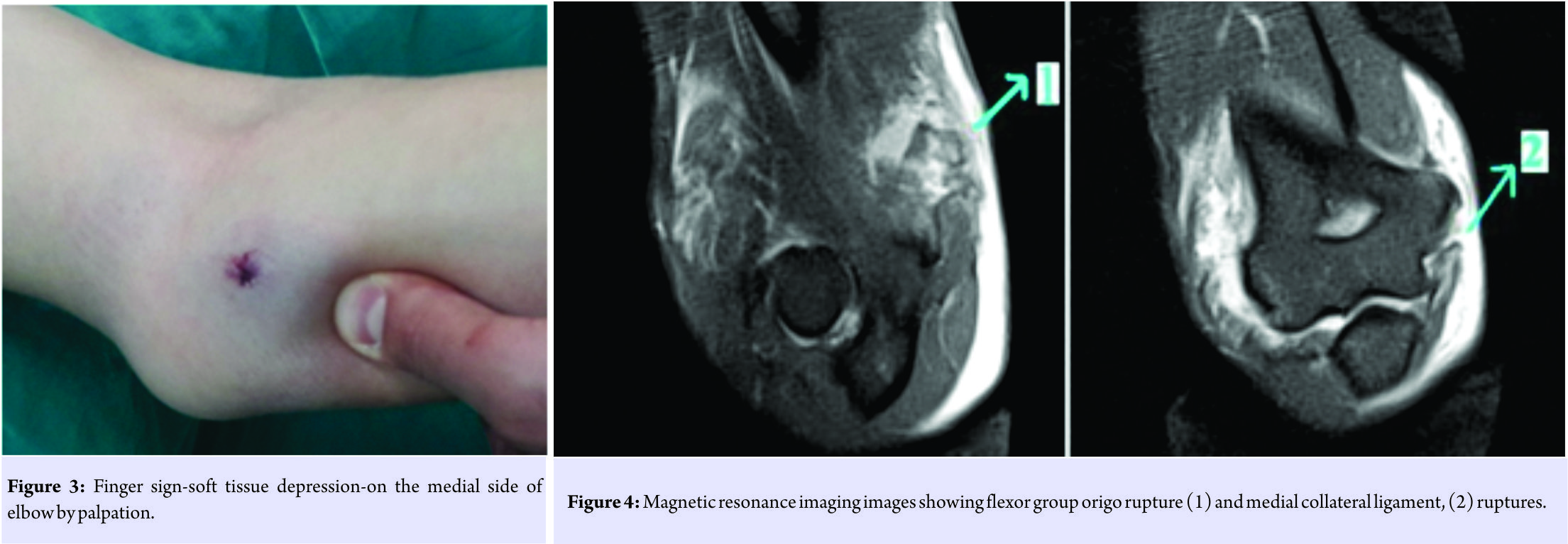 The patient was informed about the diagnosis and planned surgical attempt. Then, his inscriptive informed consent was provided. Surgical treatment was performed urgently. Using medial approach, MCL, FGO, and joint were accessed (Fig. 5).
The patient was informed about the diagnosis and planned surgical attempt. Then, his inscriptive informed consent was provided. Surgical treatment was performed urgently. Using medial approach, MCL, FGO, and joint were accessed (Fig. 5).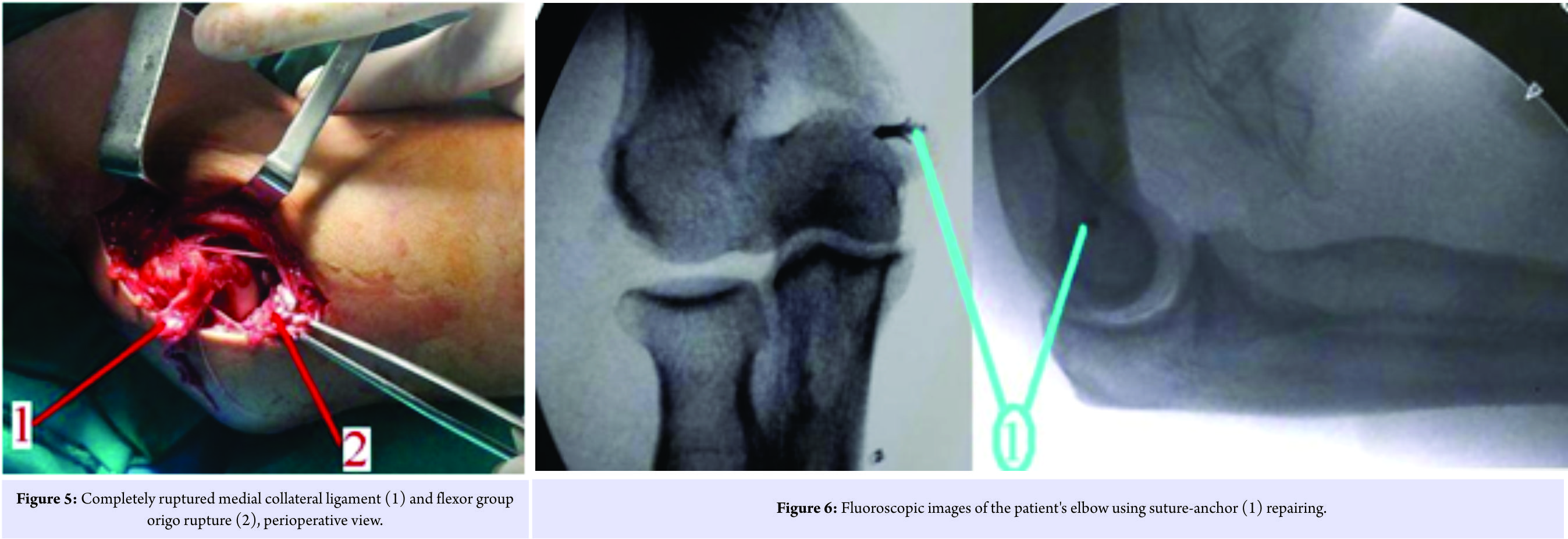 Ulnar nerve was preserved and protected during the operation. MCL was observed completely (containing both A-P bundles) ruptured, and repaired by suture-anchor implant (Fig. 6).FGO was seen completely ruptured and repaired by drilling holes to the bone and transosseous-passing sutures. Long arm splint was applied about 2weeks. After immobilization, appropriate rehabilitation program including passive motion was done using angle-adjustable armrest about 3 weeks. Active motion was begun at the 5th week. No complication was observed during follow-ups (Fig. 7).
Ulnar nerve was preserved and protected during the operation. MCL was observed completely (containing both A-P bundles) ruptured, and repaired by suture-anchor implant (Fig. 6).FGO was seen completely ruptured and repaired by drilling holes to the bone and transosseous-passing sutures. Long arm splint was applied about 2weeks. After immobilization, appropriate rehabilitation program including passive motion was done using angle-adjustable armrest about 3 weeks. Active motion was begun at the 5th week. No complication was observed during follow-ups (Fig. 7).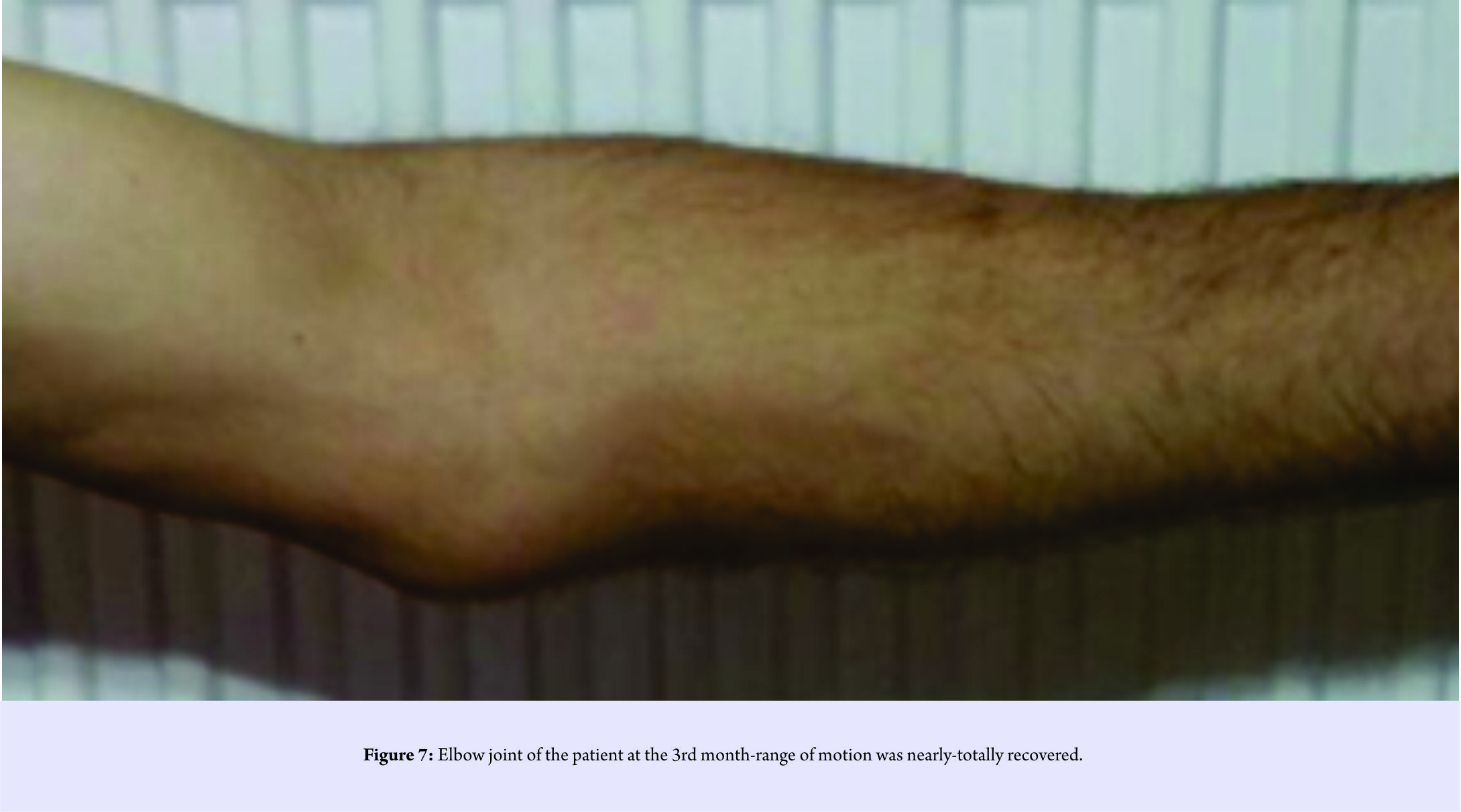
Discussion
Detailed physical examination after reduction of elbow-dislocated patients must be done[3, 4, 5]. In this examination, ligamentous instability, medial and/or lateral humeral condyle and/or epicondyle fractures, radial head fracture, and ulnar coronoid process fracture accompanying elbow joint dislocations should be investigated [3, 4, 5, 6, 7]. Computerized tomography imaging must be done for the patients for advanced research of detected osseous pathology on plain radiographs. In addition, ligamentous instability tests must be performed[8]. After physical examination, if finger sign and valgus stress tests are positive, MRI must be done. To the best of our knowledge, after researches of our patient, we diagnosed complete MCLR and complete FGOR without fracture, which had not been reported until now. Isolated MLCR rarely requires surgery [2]. For our patient, we determined surgery for the treatment strategies because of FGOR accompanying MCLR. Mostly, the fracture is observed on elbow dislocations with ligamentous instability [4]. We have not encountered fracture on our patient. When mentioned elbow dislocation, ulnohumeral dislocation is remembered. We have detected radioulnar convergent and ulnohumeral posterolateral dislocation in our patient. Mostly, closed reduction methods are possible for these cases. We also have performed closed reduction. Treatment strategies and process are directly affected by discovering combined instability reasons in the emergency department meticulously and confirmation by imaging methods[9, 10]. It will be inevitable to meet catastrophic morbidities for elbow joint if accompanying pathologies are missed[4]. Missed soft tissue pathologies cause chronic elbow pain, recurrent chronic elbow instability, and serious elbow dysfunction. As a result, surgical treatment and following proper rehabilitation program application for the cases with FGOR accompanying ligamentous injury is necessary.
Conclusion
Although conservative treatment indications are present for simple elbow dislocations, it is necessary to make thorough physical examination and to use appropriate radiological modalities for complex dislocations. Then, the key point about complete recovery or catastrophe is to combine physical and radiological signs of the patient and proper treatment strategies. Anywhere occurred and seen any joint dislocation is urgency. Diagnosis and reduction must be done quickly as soon as possible. When FGOR coexists with MCLR together without fracture, surgical treatment must be done. In addition, if fracture exists, appropriate fixation methods for the treatment must be performed.
Clinical Message
When encountered an elbow dislocation in the emergency clinic, a good cooperation between emergency and orthopedic department including sedoanalgesia and acute reduction is essential. After reduction, a good clinical evaluation and, if possible, acute radiologic imaging studies must be done to diagnose accompanying other suspicious bone and soft tissue injuries. After advanced research indicated and required surgery, and a good rehabilitation process must be applied to encounter no or minimal morbidity and disability of an elbow joint.
References
1. Canale ST, Beaty JH. Campbell’s Operative Orthopaedics. Philadelphia, PA: Elsevier Health Sciences; 2012.
2. Tashjian RZ, Wolf BR, van Riet RP, Steinmann SP. The unstable elbow: Current concepts in diagnosis and treatment. Instr Course Lect 2016;65:55-82.
3. Sheps DM, Hildebrand KA, Boorman RS. Simple dislocations of the elbow: Evaluation and treatment. Hand Clin 2004;20:389-404.
4. Hackl M, Beyer F, Wegmann K, Leschinger T, Burkhart KJ, Müller LP. The treatment of simple elbow dislocation in adults—a systematic review and meta-analysis. DtschArzteblInt 2015;112:311-9.
5. O’Driscoll SW, Jupiter JB, Cohen MS, Ring D, McKee MD. Difficult elbow fractures: Pearls and pitfalls. Instr Course Lect 2003;52:113-34.
6. Timothy OW, Mackenzie SP, Gray AJ. McRae’s Orthopaedic Trauma and Emergency Fracture Management. Seiten; Verlag: Elsevier Health Sciences; 2015.
7. Martin BD, Johansen JA, Edwards SG. Complications related to simple dislocations of the elbow. Hand Clin 2008;24:9-25.
8. Schnetzke M, Fuchs J, Vetter SY, Beisemann N, Keil H, Grützner P, et al. Intraoperative 3D imaging in the treatment of elbow fractures-a retrospective analysis of indications, intraoperative revision rates, and implications in 36 cases. BMC Med Imag 2016;16:24.
9. Chen HW, Liu GD, Ou S, Fei J, Zhao GS, Wu LJ, et al. Operative treatment of terrible triad of the elbow via posterolateral and anteromedial approaches. PLoS One 2015;10:e0124821.
10. Egol KA, Immerman I, Paksima N, Tejwani N, Koval KJ. Fracture-dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU HospJt Dis 2007;65:263-70.
 |
 |
 |
 |
 |
| Dr. Erdem Yunus Uymur | Dr. Ahmet Köse | Dr. Sultan Tuna Akgöl Gür | Dr. Recep Dinçer | Dr. Murat Topal |
| How to Cite This Article: Uymur E. Y, Köse A, AkgölGür S. T, Dinçer R, Topal M. Elbow PosterolateralDislocation Accompanying Flexor Group Origo Rupture without Fracture – A Case Report. Journal of Orthopaedic Case Reports 2018 Jan-Feb; 8(1): 15-17 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




