[box type=”bio”] Learning Point for this Article: [/box]
Computer-assisted navigation may assist with the accuracy of acetabular component selection and positioning during BHR.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 48-52| Jonathan M Vigdorchik, Ameer Elbuluk, Jessica R Benson, Jeffrey M Muir. DOI: 10.13107/jocr.2250-0685.994
Authors: Jonathan M Vigdorchik[1], Ameer Elbuluk[1], Jessica R Benson[2], Jeffrey M Muir[2]
[1]Department of Orthopaedic Surgery, NYU Langone Medical Center-Hospital for Joint Diseases, New York, USA.
[2]Department of Clinical Research, Intellijoint Surgical, Inc., Waterloo, Ontario, Canada.
Address of Correspondence:
Dr. Jonathan Vigdorckik,
301 E 17th Street, New York – 10003, USA.
E-mail: jonathan.vigdorchik@nyumc.org
Abstract
Introduction: Inaccurate positioning of acetabular and femoral components during Birmingham Hip Resurfacing (BHR) can lead to increased wear, edge-loading, and failure of the prosthesis, a consequence of substantial concern for young and active patients seeking long-term, post-operative survival of the joint. In turn, sizing of the acetabular component during BHR is limited by the size of the native femoral neck, and reaming of the acetabulum should be minimized to optimize the bony architecture for potential subsequent arthroplasties. Computer-assisted navigation systems (CAS) can improve the accuracy of component selection and positioning during total hip arthroplasty (THA); however, evidence for the usefulness of CAS in BHR is lacking. The present report summarizes a case of BHR performed with navigation to assist with component positioning.
Case Report: A 34-year-old male martial arts instructor presented with a constant and localized pain in the left hip and groin. Following the examination, the patient was diagnosed with left hip impingement and osteoarthritis. Due to his age and active lifestyle, the patient elected to undergo BHR rather than THA. The navigation tool was used to assist with acetabular reaming and to confirm final cup placement. Post-operatively, standard, anteroposterior pelvic radiographs showed a final cup position of 39.0° inclination and 24.7° anteversion, which was confirmed by the navigation tool. A pre-operative leg length differential of 3mm was measured from pre-operative radiographs; however, leg lengths were equalized following BHR.
Conclusion: This report summarizes a case of BHR performed in a young, active patient with the assistance of a novel surgical navigation tool. The use of the navigation device allowed for more accurate acetabular preparation and component positioning, maximizing the bone-sparing characteristics of BHR.
Keywords: Birmingham hip resurfacing, computer-assisted navigation, accuracy.
Introduction
Total hip resurfacing (THR) is an alternative to total hip arthroplasty (THA) that constitutes approximately 10% of arthroplasty procedures performed annually [1]. Performed most commonly in young, active adults, hip resurfacing is characterized by the conservation of femoral bone stock and improvements in post-operative mobility and stability when compared to THA [2]. The vast majority of THR procedures are performed using the Birmingham Hip Resurfacing (BHR) system (BHR, Smith and Nephew, Andover, MA), utilizing metal-on-metal (MoM) prosthetic components. As such, concerns have been raised regarding impingement and metal wear, which can induce increased serum levels of metal ions, potentially subjecting the patient to adverse events including osteolysis and metallosis [3]. Cases regarding patient metal sensitivity are also of recent concern due to their increased incidence [4]. As with THA, accurate component placement in BHR has proven vital to the stability, survival, and potentially long-term safety of the joint, with malpositioning leading to increased edge loading, wear, and impingement [5]. Overall, malalignment of femoral and acetabular components during THR has been shown to account for 81% of required revision surgeries and may associate with premature failure of the joint prosthesis [6].
Computer-assisted navigation systems (CAS) represent an emerging and growing technology in THA, but the described use of CAS in THR is sparse. While CAS has been shown to effectively assist surgeons with the accurate sizing and placement of prosthetic hip components during THA [7], the utilization of CAS in BHR is less characterized, with some reports suggesting no significant benefit [8]. Here, we report a case of BHR performed in a young, active male patient in which a novel navigation device was used to assist with correct positioning of prosthetic components.
Case Report
Patient presentation
A 34-year-old martial arts instructor presented with a chief complaint of progressive left hip pain of insidious onset and approximately 8-year duration. The pain was constant and localized to the left hip and groin, particularly with prolonged sitting and walking, with radiation to the knee. The patient denied any antecedent trauma or major hip injuries since childhood. Past medical, family, and social history were unremarkable. Conservative management including over-the-counter nonsteroidal anti-inflammatory medications, activity modification, and physical therapy had only provided minimal relief.
Orthopedic examination and diagnosis
Initial orthopedic examination revealed the patient walking with an antalgic gait associated with anterior left hip pain. Anterior impingement testing (internal rotation and adduction during passive flexion of the knee to 90°) was positive, reproducing the patient’s symptoms. Patrick’s test revealed moderate groin pain and restricted sacroiliac joints. Lower limb neurologic examination was unremarkable. A pre-operative Harris Hip Score of 60 was recorded.
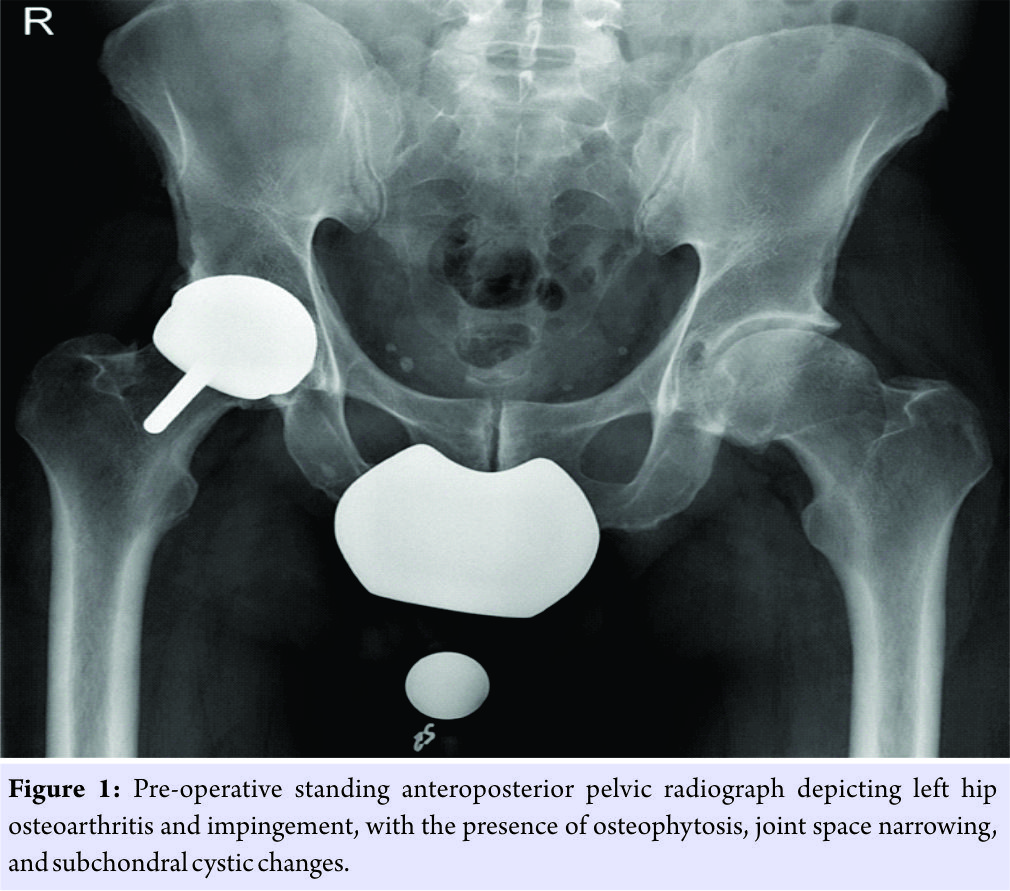
Plain film radiographs were obtained and revealed bilateral hip joint osteoarthritis, with osteophytosis, joint space narrowing, and subchondral cystic changes in the left hip (Fig. 1). A cam-type deformity of the femur, pincer deformity of the acetabulum, and a calcified labrum were also observed. Magnetic resonance imaging confirmed advanced left hip osteoarthritis. Based on patient history, age, and examination findings, the final diagnosis was left hip impingement and osteoarthritis. Following a lengthy discussion regarding BHR versus THA, the patient decided to proceed with BHR, due to his highly active lifestyle.
Treatment
Surgery was performed with the assistance of Intellijoint HIP® (Intellijoint Surgical, Inc., Waterloo, ON, Canada), a 3D mini-optical navigation device currently approved for use in posterior, lateral, and direct anterior approaches in THA. This navigation tool utilizes optical technology, infrared light, and microelectronics to deliver measurements for cup position and leg length in real time which are made accessible to the surgeon on a workstation monitor located just outside of the sterile field. The device has received clearance from the US Food and Drug Administration for use in primary hip arthroplasty but has not been evaluated for use in hip resurfacing procedures.
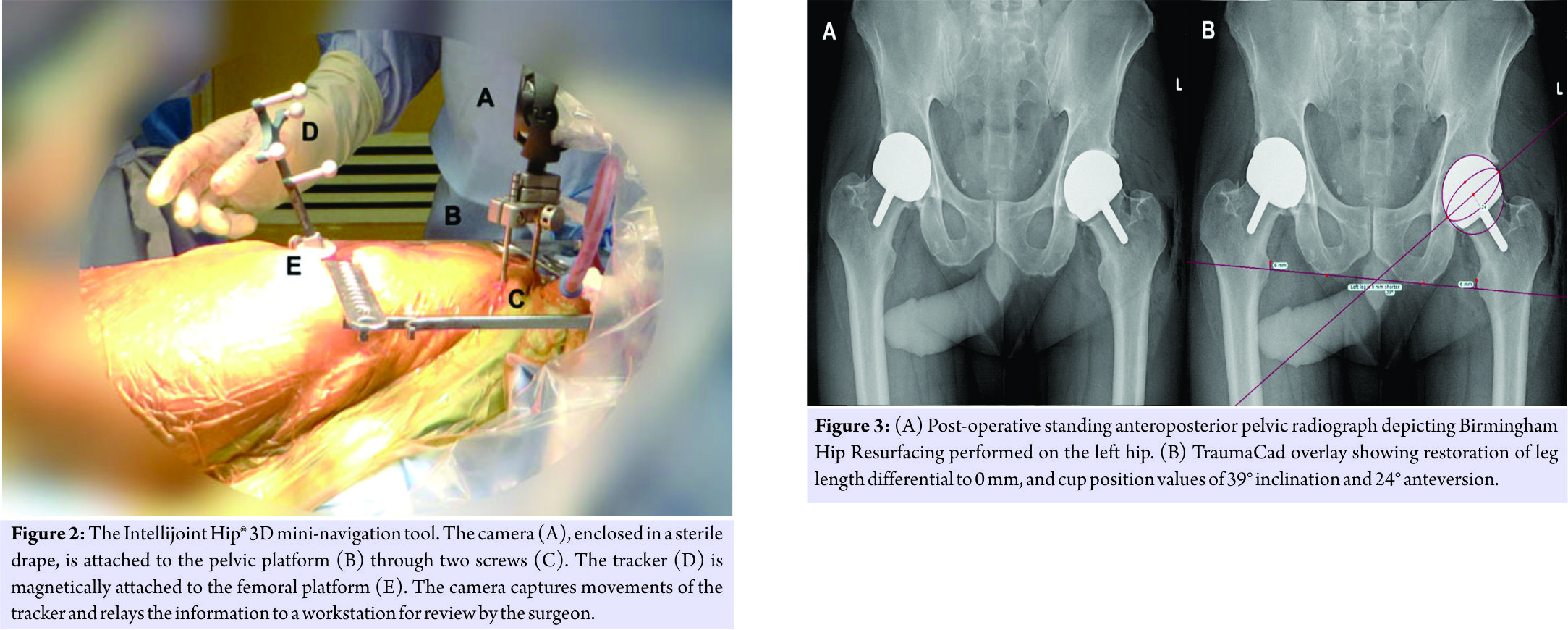
The use of the device in the presented case followed the surgical workflow for the posterior THA application, which has been described previously [9]. In brief, the navigation system contains a camera, probe, and tracker located within the sterile field. The camera is magnetically attached to a pelvic platform that sits atop two surgical screws inserted into the ipsilateral iliac crest. The tracker is similarly attached to a small femoral platform installed laterally on the greater trochanter through a single screw. The camera captures the movements and position of the tracker and relays data in real time to a computer workstation placed outside of the sterile field. In addition to the femoral platform, the tracker can be fixed to various other objects (e.g., impactor and surgical probe) during surgery to provide data regarding their position and orientation (Fig. 2).
The patient was placed in the lateral decubitus position per normal surgical protocols and fixed with rigid pelvic fixation. The affected hip area was then prepped and draped in the usual sterile fashion. Using an 11-blade, two stab incisions were made over the iliac crest. Two threaded pins were inserted into the crest and confirmed to be placed in bone. The pelvic platform was installed on the pins, tightened, and the camera attached. A standard posterolateral incision was made through the skin, and dissection was carried down through subcutaneous tissue to the underlying fascia achieving hemostasis where necessary. The femoral platform was then installed on the greater trochanter. The femoral head was dislocated and sized to 50mm without evidence of notching. An anterior capsulotomy was made to further release the femur. The acetabulum was then exposed with a plan for a 56 mm cup. The labrum was excised with a long-handle knife, and the acetabular rim and cotyloid fossa were exposed. The acetabulum was reamed in accordance with the pre-operative plan, using the navigation tool to intermittently monitor the orientation of the acetabular cup component. Following copious irrigation, the final cup was impacted into position, confirmed by the navigation tool at 36° inclination and 24° anteversion. Following the procedure, the patient was returned to the supine position to verify all lower extremity compartments which were soft and compressible and to confirm intact distal pulses and leg length restoration. An anteroposterior (AP) pelvic radiograph was taken in the operating room (OR) and reviewed before transfer. The patient was transferred to the recovery room in stable condition.
Post-operative outcomes
Standard, post-operative AP pelvic radiographs were obtained and analyzed using TraumaCad (Brainlab, Chicago, USA). Final cup inclination and anteversion values were measured in triplicate and averaged. Final cup position was calculated from radiographs as 39.0° inclination and 24.7° anteversion (Fig. 3). Pre-operative leg length differential was measured on the pre-operative AP radiograph at 3 mm and was restored to 0 mm following BHR.
Follow-up
Post-operatively, the patient was doing extremely well and was pain free with no physical limitations. At his 12-week follow-up visit, a Harris Hip Score of 92 was recorded, showing an improvement from his pre-operative score of 60.
Discussion
A substantial challenge in THR is proper positioning of the prosthetic components and subsequent avoidance of edge loading and wear. Improper component positioning in surgeries utilizing MoM components specifically, such as BHR, can additionally contribute to increases in serum metal ions, patient metal sensitivities, and metallosis. While CAS can improve the accuracy of component selection and positioning during THA, the effectiveness of CAS in BHR is less understood. In the present case, a novel navigation tool was used to assist with accurate positioning of the acetabular and femoral components. Intraoperative monitoring of cup position and orientation allowed for placement of the acetabular cup component in an optimal orientation of 39° of inclination and 25° of anteversion, and to equalize a 3 mm leg length inequality, both of which were confirmed on post-operative imaging.
Malpositioning of the acetabular cup can lead to serious consequences, with increased wear and edge-loading resultant of improper positioning of prosthetic components a well-documented concern for hip arthroplasties [5]. Increased wear on the joint in these circumstances may decrease joint stability, and in turn, promote dislocation and the likelihood of revision surgery [6]. Indeed, DeHaan et al. [10] suggest that increased wear occurs in prosthetic joints placed at steep inclination angles >55°. Similarly, Ollivere et al. [11] found that misplaced acetabular components, especially at inclination angles >45°, were linked to increased requirements for revision surgery. MoM prosthetic joints, such as in BHR, have specific consequences pertaining to misplaced components. Studies have shown a significant increase in the joint fluid levels and serum levels of cobalt and chromium ions in individuals with an MoM prosthetic hip, correlating with increased wear and metallosis [3]. In addition, adverse reactions to metal debris associated with THR requiring early revision surgery have been well documented, to the extent that two commercial implants have been recalled from the marketplace [12]. Moreover, patient sensitivity to metal implants is a recent concern, as numerous reports of serious adverse events of groin pain leading to revision surgery have been documented [4]. In such cases, a complete alleviation of symptoms was achieved by switching to ceramic-on-ceramic bearings.
The removal of large volumes of acetabular bone during BHR may compromise the integrity of the bony architecture and limit the ability to perform future THA procedures. Brennan et al. [13] have discussed this concern, stating that while THR conserves femoral bone stock, the conservation of the acetabulum cannot be guaranteed, as the acetabular component must be sized according to the native femoral neck. Indeed, recent studies have confirmed that significantly more acetabular bone is removed during BHR when compared to traditional THA [14]. Conversely, while THA may offer the advantage of less restricted sizing of the acetabular component due to femoral head excision, the procedure in turn removes much of the native femoral bone. These procedural features are of concern for young and active adult patients, as optimizing bone conservation should be a primary concern, to maintain the ability to subsequently perform full arthroplasty procedures.
In the present case, we found that the utilization of CAS allowed for meticulous and accurate acetabular reaming, potentially mitigating excess acetabular bone loss. The final orientation of the acetabular cup component was confirmed with both the navigation device and post-operative radiographs, with the accuracy of intraoperative measurements matching the device accuracy observed in previous clinical studies of THA [15]. This approach better maintained the patient’s pelvic architecture without jeopardizing the ability to perform subsequent revision procedures, should further surgical intervention be required. Finally, accurate positioning of prosthetic components should help to reduce the risk of post-operative complications and the potential for subsequent revision surgery following BHR.
Conclusion
This case demonstrates the value of a novel surgical navigation tool during BHR, allowing for increased specificity when preparing the acetabulum and optimizing the accuracy of acetabular component positioning while limiting the volume of excavated bone. Increased accuracy and the potential bone-sparing benefits of CAS may be advantageous for young and active patients seeking less invasive surgical intervention.
Clinical Message
Conservation of the native femoral head and neck during BHR places limitation on the sizing of the acetabular component. Acetabular reaming should be minimized to optimize the bony architecture for potential subsequent arthroplasties. Computer-assisted navigation may assist with the accuracy of acetabular component selection and positioning during BHR.
References
1. The NJR Centre HH. 9th. Annual Report; 2009.
2. McMinn D, Treacy R, Lin K, Pynsent P. Metal on metal surface replacement of the hip. Experience of the mcMinn prothesis. Clin Orthop Relat Res 1996;329:S89-98.
3. De Smet K, De Haan R, Calistri A, Campbell PA, Ebramzadeh E, Pattyn C, et al. Metal ion measurement as a diagnostic tool to identify problems with metal-on-metal hip resurfacing. J Bone Joint Surg Am 2008;90 Suppl 4:202-8.
4. Campbell P, Shimmin A, Walter L, Solomon M. Metal sensitivity as a cause of groin pain in metal-on-metal hip resurfacing. J Arthroplasty 2008;23:1080-5.
5. Campbell P, Beaulé PE, Ebramzadeh E, Le Duff MJ, De Smet K, Lu Z, et al. The john charnley award: A study of implant failure in metal-on-metal surface arthroplasties. Clin Orthop Relat Res 2006;453:35-46. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00003086-200612000-00009.
6. De Haan R, Campbell PA, Su EP, De Smet KA. Revision of metal-on-metal resurfacing arthroplasty of the hip: The influence of malpositioning of the components. J Bone Joint Surg Br 2008;90:1158-63.
7. Gross A, Muir JM. Identifying the procedural gap and improved methods for maintaining accuracy during total hip arthroplasty. Med Hypotheses 2016;94:93-8.
8. Krüger S, Zambelli PY, Leyvraz PF, Jolles BM. Computer-assisted placement technique in hip resurfacing arthroplasty: Improvement in accuracy? Int Orthop 2009;33:27-33.
9. Paprosky WG, Muir JM. Intellijoint HIP®: A 3D mini-optical navigation tool for improving intraoperative accuracy during total hip arthroplasty. Med Devices (Auckl) 2016;9:401-8.
10. De Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, De Smet K, et al. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br 2008;90:1291-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18827237%5Cnwww.bjj.boneandjoint.org.uk.
11. Ollivere B, Duckett S, August A, Porteous M. The birmingham hip resurfacing: 5-year clinical and radiographic results from a district general hospital. Int Orthop 2010;34:631-4.
12. Seppänen M, Karvonen M, Virolainen P, Remes V, Pulkkinen P, Eskelinen A, et al. Poor 10-year survivorship of hip resurfacing arthroplasty. Acta Orthop 2016;87:554-9.
13. Brennan SA, Harty JA, Gormley C, O’Rourke SK. Comparison of acetabular reamings during hip resurfacing versus uncemented total hip arthroplasty. J Orthop Surg (Hong Kong) 2009;17:42-6.
14. Crawford JR, Palmer SJ, Wimhurst JA, Villar RN. Bone loss at hip resurfacing: A comparison with total hip arthroplasty. Hip Int 2005;15:195-8.
15. Paprosky W, Muir J. Improved Accuracy of Component Placement During Total Hip Arthroplasty: A Retrospective Cohort Study. In: The Hip Society Annual Meeting; 2016.
 |
 |
 |
 |
| Dr. Jonathan M. Vigdorchik |
Mr. Ameer Elbuluk | Ms. Jessica R. Benson |
Dr. Jeffrey M. Muir |
| How to Cite This Article: Vigdorchik JM, Elbuluk A, Benson JR, Muir JM. Birmingham Hip Resurfacing Using a Novel Mini-navigation System: A Case Report. Journal of Orthopaedic Case Reports 2018 Jan-Feb; 8(1): 48-52 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com