[box type=”bio”] Learning Point for the Article: [/box]
It should be careful that HA debris may become cause of osteolysis with hematoma.
Case Report | Volume 8 | Issue 4 | JOCR July – August 2018 | Page 25-28| Shougo Matsuda, Nobuhiro Kaku, Tomonori Tabata, Hiroshi Tsumura. DOI: 10.13107/jocr.2250-0685.1142
Authors: Shougo Matsuda[1], Nobuhiro Kaku[1], Tomonori Tabata[1], Hiroshi Tsumura[1]
[1]Department of Orthopaedic Surgery, Faculty of Medicine, Oita University, 1-1 Idaigaoka Hazama-Machi, Yufu City, Oita. Japan.
Address of Correspondence:
Dr. Dr. Nobuhiro Kaku,
Department of Orthopaedic Surgery, Faculty of Medicine, Oita University,
1-1 Idaigaoka Hazama-Machi, Yufu City, Oita 879-5593. Japan.
E-mail: nobuhiro@oita-u.ac.jp
Abstract
Introduction: Osteolysis around the prosthesis following total hip arthroplasty (THA) is usually expanded slowly in the mid to long term, not progressive in the short term. Hematoma around the prosthesis is a rare phenomenon after a period of 1 year or more after surgery other than metal on metal THA. In addition, there are no studies reporting that hydroxyapatite (HA) itself has a possibility to cause osteolysis or hematoma after THA. This case has a particular disease phenomenon with three unusual factors, such as progressive osteolysis, hematoma, and HA debris in granulation tissue, following revision THA.
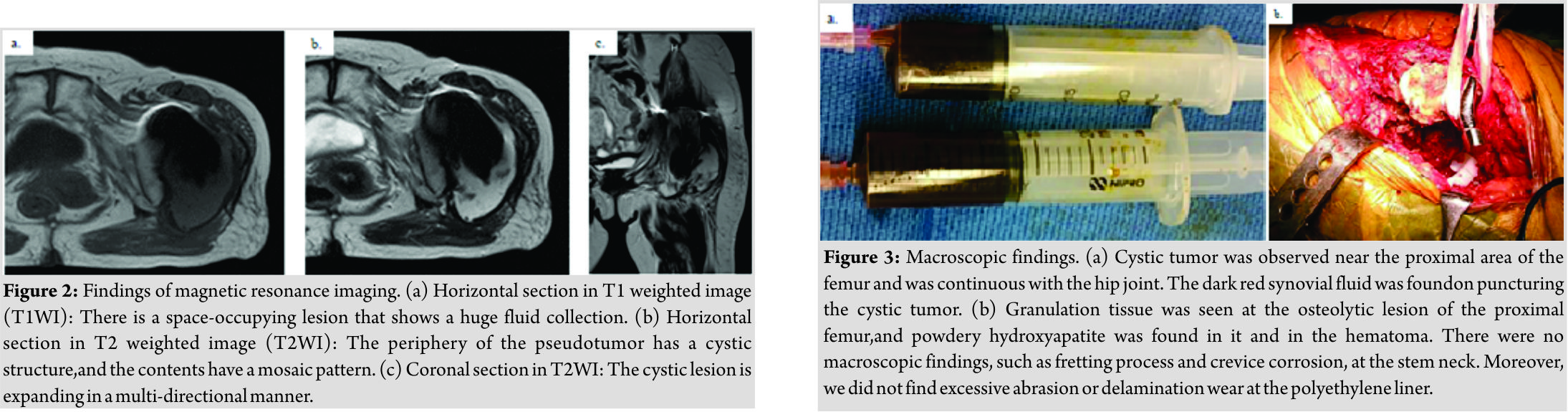
Case Report: A 79-year-old woman with pain in the left hip joint underwent a revision THA, using HA mesh and ultra high molecular weight polyethylene fiber cable for impaction bone grafting to fill a bone defect in the proximal femur in 2011. There were no abnormal findings clinically or on radiograph until 2014.Moderate osteolysis was observed at the lesser trochanter and the area distal to the greater trochanter on the radiograph in 2015. The synovial fluid culture was negative. On magnetic resonance imaging examination, the margin showed a low-density shell in both the T1- and T2-weighted images, and the inside was a mosaic mass, with mixed low- and high-density are as extending in a multidirectional manner. During surgery, cystic mass covered with a thick membrane was found around the artificial hip joint, and the inside of the capsule was full of solid and fluid hematoma and dark blood. There was no apparent wear and tear debris of the implant. On pathological examination, evidence of chronic hematoma, granulation tissue, and HA debris, interspersed inside the granulation tissue were observed.
Conclusion: We experienced an extremely rare case with osteolysis and hematoma that progressively expanded in a short period of time after revision THA using HA mesh, which seemed to be caused by, crushed HA and resulted in osteolysis accompanied by hematoma. This case revealed that HA it has a possibility to cause osteolysis or hematoma after THA.
Keywords: Total hip arthroplasty, Revision surgery, Hematoma, Osteolysis, Hydroxyapatite, Polyethylene fiber cable.
Introduction
Osteolysis around the prosthesis following total hip arthroplasty (THA) is usually caused by wear and tear debris, such as polyethylene (PE), on the weight-bearing surface and expanded slowly in mid-long term, not progressive in the short term. Hematoma around the prosthesis is a rare phenomenon after a period of 1 year or more after surgery other than metal on metal THA. There are a few reports of progressive osteolysis with hematoma following THA. However, there are no studies reporting that hydroxyapatite (HA) itself has a possibility to cause osteolysis or hematoma after THA. This is a case of progressive osteolysis with hematoma after THA using HA mesh.
Case Report
A 79-year-old female with no medical history complained of left hip pain. She under went a primary THA in 1986(Charnley cemented monoblock stem and cup; DePuy Synthes, Johnson and Johnson, Warsaw, IN, US)for dysplastic osteoarthritis, and the revision THA (Secure-Fit PSL cup and Omnifit Specialty Stem, Stryker Orthopaedics, Mahwah, NJ, US)was performed at another hospital due to loosening of the cup and stem in 1997.Due to the loosening of the stem again, the patient was brought to our hospital for revision THA in 2011. A metal shell had achieved good fixation to the iliac bone with osseointegration; however, the pelvic discontinuity was seen on the radiograph. Hence, we performed a revision surgery which exchanged the PE liner alone on the acetabular side and stem, without replacing the metal shell. Since there was a moderate bone defect in the proximal part of the femur, we used the bioabsorbable plates used in this study, which were formed from 50×50-mmmesh sheets made from HA (40% w/w) and PLLA (60% w/w) composites Super Fixsorb MX40 mesh; Johnson and Johnson, Tokyo, Japan, and Takiron, Osaka, Japan) and ultrahigh molecular weight PE fiber cable (Nesplon tape; Alfresa, Osaka, Japan).Atwo Nesplon tapes with 3mm width was used to make a paling, which was prepared by transplantation with morcellized frozen allogeneic bone using an impaction bone grafting(IBG) technique. An 80 g of Simplex bone cement (Stryker Orthopaedics) was injected under compression using a cement gun, and a 200-mm long Exeter stem(Stryker Orthopaedics)was fixed.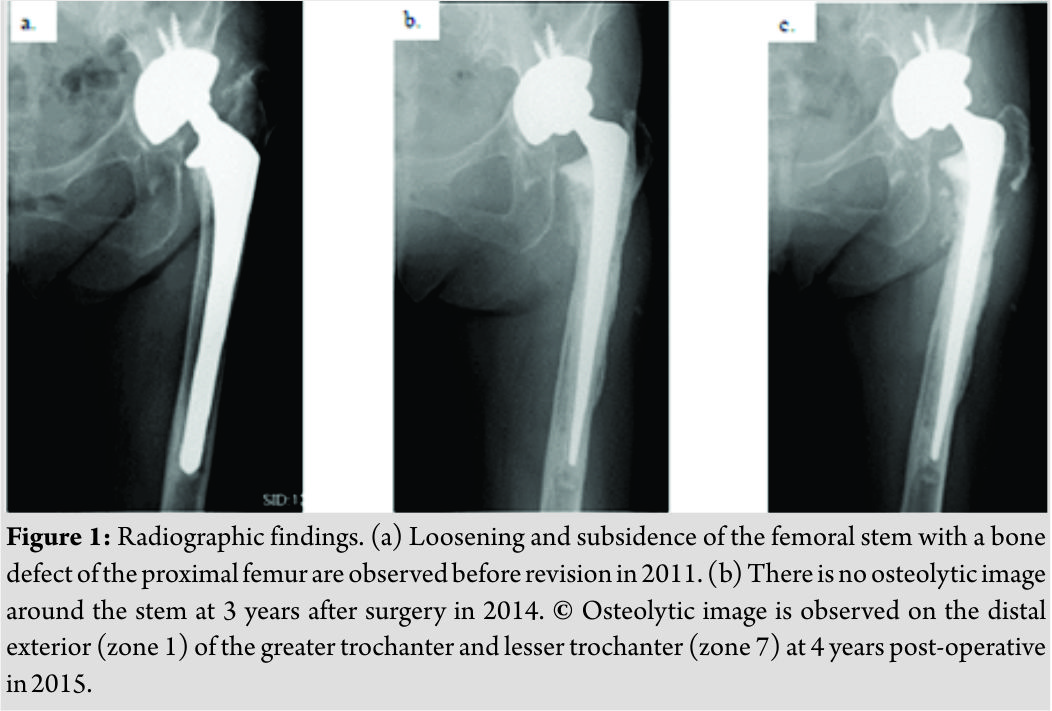
We analyzed the granulation tissue through a rapid pathological examination and did not find any pathological findings of infection or tumor. The pelvis showed discontinuity; however, there was no bleeding source. There was no macroscopic damage of implants, such as wear or corrosion of the stem neck, ball head, and PE liner. Hence, the liner, metal shell, and stem were preserved and thoroughly washed after the removal of hematoma, capsule, HA debris, and granulation tissue as much as possible. Only the ball head was replaced. Since a pathological fracture had already occurred distal to the greater trochanter, we performed osteosynthesis with an Accord cable (Smith and Nephew Inc., Memphis, TN, US) after grafting the allograft bone(Fig. 4).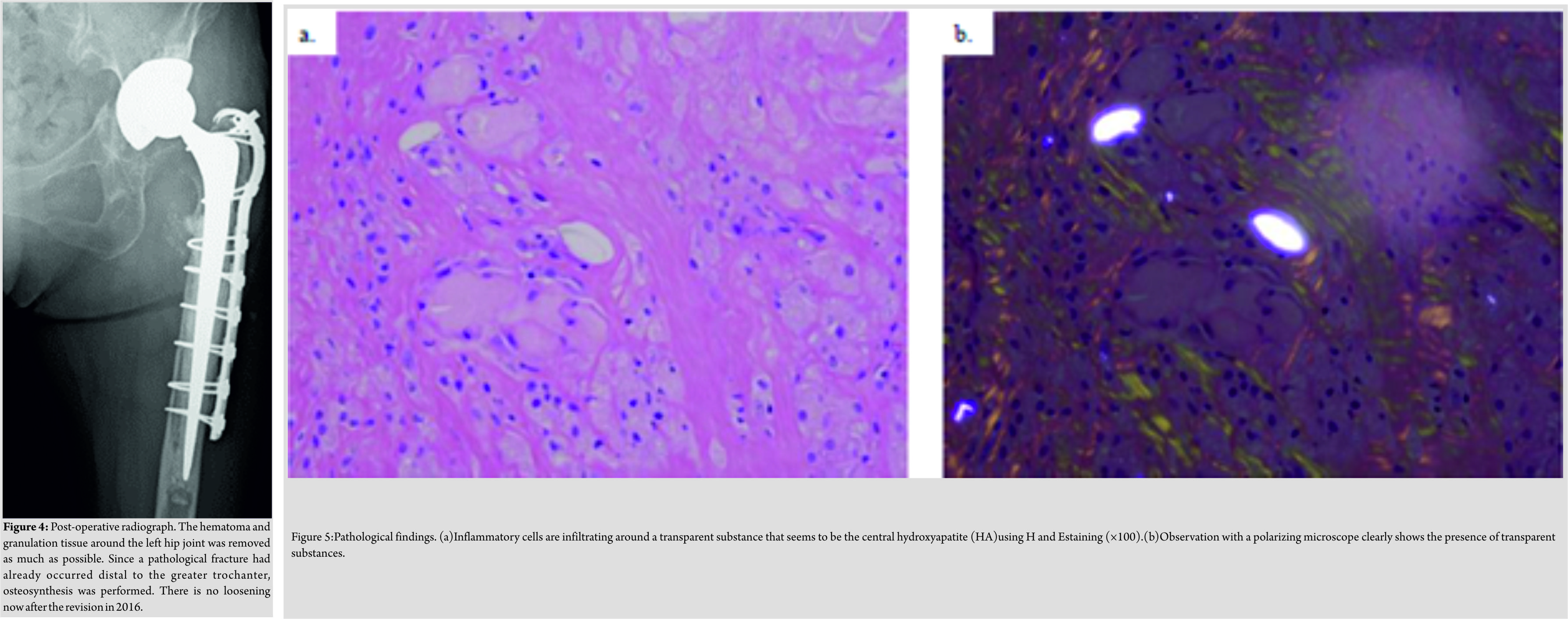
Discussion
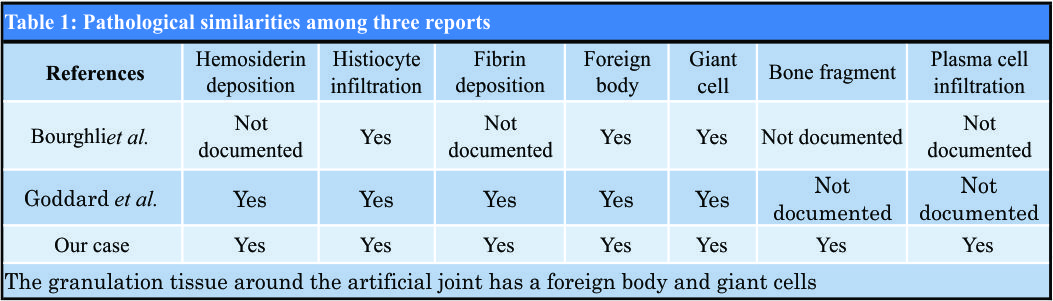
Devices such as screws made of HA, which might be replaced by the bone, are useful and regularly used in orthopedic surgeries. For a large bone defect during revision surgery for failed THA, we usually perform IBG after creating a barrier using HA mesh for reconstruction of the acetabulum and femur. These devices have proven useful, and since HA mesh has high transparency on X-ray than stainless steel, it is feasible to observe the change in the graft bone and avoid the heavy metal artifact. The cause of osteolysis around a non-infectious hip prosthesis is mainly abrasion from wear and tear of the weight-bearing surface. The device used during the previous surgery may have resulted in the generation of the wear from the bearing surface as the third body, such as metallic or HA wear debris, which has been reported[1, 2]. However, there is no study reporting that HA it has the possibility to cause osteolysis or hematoma after THA. In this case, the hematoma was formed within a short period of time, osteolysis had extended, and a large number of fragments of HA existed in the granulation tissue. The causal relationship between each factor is still unknown. The mechanism of the combination of Nesplon tape and HA mesh causing the complication as well as the breakage of the HA remains unknown. Moreover, the mechanism for progressive osteolysis in a short period of time is not well known. Osteolysis around the artificial joint with hematoma is formed as a pseudo tumor due to the friction of the metal with a metal-bearing surface[3]. Ando et al. have reported a case with a hematoma at the buttock after metal-on-metal THA [4]; but, osteolysis was absent in their case. Bourghli et al. [5] and Goddard et al. [6] have reported osteolysis accompanied by hematoma with metal on PE, as in this case. Bourghli et al. believed that inflammatory reactions are induced by wear and tear debris, which leads to easy bleeding due to the occurrence of synovitis, pseudo tumor formation from old bleeding and granulation tissue, and osteolysis. Goddard et al. considered that the cause of osteolysis around the artificial hip joint is a pseudotumor, which was covered with a fibrous thick film including necrotic tissue, fibrin, and hemorrhage inside with chronic expanding hematoma. There was no obvious trigger for hematoma formation in either report, and the cause was unknown. There were common findings on the histopathological examination in the past reports and our case (Table 1), for example, deposition of hemosiderin and invasion of some cells in the capsule of the hematoma. Fibrin deposition was also observed. Granulation tissue around the artificial joint showed a foreign body and giant cells surrounding it. Thus, it was confirmed that in this case, the components of the hematoma and granulation tissue formed due to a foreign body existed separately in the same space. Hence, it is assumed that osteolysis due to hematoma and reactive osteolysis due to foreign body debris were mixed. It has been known that osteolysis due to hematoma occurs even in hemophilicarthropathy [7, 8]. Hemosiderin adheres to the synovium, resulting in synovial inflammation, hyperplasia, joint destruction, and osteolysis. Furthermore, it leads to a vicious circle by easy bleeding from increasing, brittle, and new blood vessels. However, the detailed mechanism is still unknown. In this example, osteolysis accompanied by the hematoma, expanded in a short period of time, and pathological findings showed that HA debris was present in the granulation tissue, but the mechanism on how hematoma or HA debris affected osteolysis was not clear.
Conclusion
We experienced an extremely rare case with osteolysis and hematoma that progressively expanded in a short period of time following revision THA using HA mesh and Nesplon tape for IBG, which seemed to be caused by, crushed HA and resulted in osteolysis accompanied by hematoma. This case has a particular disease phenomenon with three unusual factors, such as progressive osteolysis, hematoma and HA debris, in granulation tissue.
Clinical Message
Inpatients who present with progressive osteolysis around an artificial joint in a short period of time as seen on a radiograph, an evaluation of chronic expanding hematoma with CT, MRI, or ultrasound is necessary. In addition, this case revealed that HA debris itself has a possibility to cause osteolysis or hematoma after THA.
References
1. Murali R, Bonar SF, Kirsch G, Walter WK, Walter WL. Osteolysis in third-generation alumina ceramic-on-ceramic hip bearings with severe impingement and titanium metallosis. J Arthroplasty 2008;23:1240-e13-9.
2. Furlong R. Severe osteolysis after third-bodywear due to hydroxyapatite particles from acetabular cup coating. J Bone Joint Surg Br 1998;80:745-6.
3. Pandit H, Glyn-Jonens S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, et al. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br 2008;90:847.
4. Ando W, Yamamoto K, Ohzono K. Chronic expanding hematoma after metal-on-metal total hip arthroplasty. Orthopedics 2017;40:e1103-6.
5. Bourghli A, Fabre T, Tramond P, Durandeau A. Total hip replacement pseudotumoral osteolysis. Orthop Traumatol Surg Res 2010;96:319-22.
6. Goddard MS, Vakil JJ, McCarthy EF, Khanuja HS. Chronic expanding hematoma of the lateral thigh and massive bony destruction after a failed total hip arthroplasty. J Arthroplasty 2011;26:338.e13-338.e15.
7. Park JS, Ryu KN. Hemophilic pseudotumor involving the musculoskeletal system: spectrum of radiologic findings. AJR Am J Roentgenol 2004;183:55.
8. Jansen NW, Roosendaal G, Lafebar FP. Understanding haemophilic arthropathy: An exploration of current open issues. Br J Haematol 2008;143:632-40.
 |
 |
 |
 |
| Dr. Shougo Matsuda | Dr. Nobuhiro Kaku | Dr. Tomonori Tabata | Dr. Hiroshi Tsumura |
| How to Cite This Article: Matsuda S, Kaku N, Tabata T, Tsumura H. Progressive Osteolysis with Hematoma Following Revision Total Hip Arthroplasty using Hydroxyapatite Mesh: A Case Report. Journal of Orthopaedic Case Reports 2018 Jul-Aug; 8(4): 25-28. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com