[box type=”bio”] Learning Point for the Article: [/box]
Being a very rare injury and having inconspicuous presentation, bilateral posterior fracture-dislocation of shoulder can be missed and needs evaluation and screening of both shoulders by CT scan in Triple E pathologies presenting even with unilateral shoulder complaints.
Case Report | Volume 8 | Issue 4 | JOCR July – August 2018 | Page 49-52| Srinivas Kasha, Gopinath Bandari. DOI: 10.13107/jocr.2250-0685.1156
Authors: Srinivas Kasha[1], Gopinath Bandari[1]
[1]Department of Orthopaedics, Krishna Institution of Medical Sciences Ltd.,Secunderabad, Telangana. India.
Address of Correspondence:
Dr. Srinivas Kasha,
Department of Orthopaedics, Krishna Institution of Medical Sciences Ltd., Minister Road, Secunderabad, Telangana. India.
E-mail: drsrinivaskasha@gmail.com
Abstract
Introduction: Bilateral posterior fracture dislocation of both shoulders is a rare condition which can easily be missed due to its imprecise presentation. In this case report, we emphasize its diagnosis and summarize the various treatment options available for bilateral posterior fracture-dislocation of shoulders and also its management in conjunction with cavernous sinus venous thrombosis (CSVT).
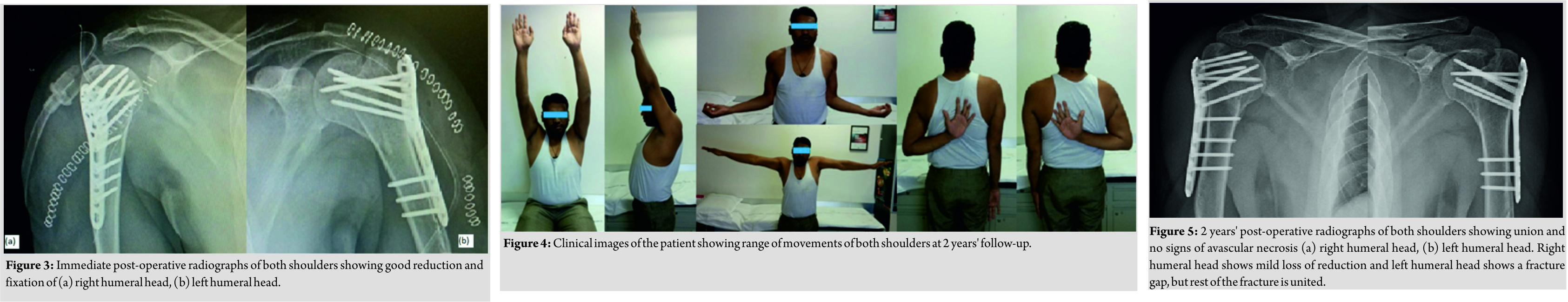
Case Report: A 29-year-old gentleman had bilateral posterior fracture-dislocation of shoulders, with comminuted three-part fractures of both humeral heads, after two episodes of seizures, following CSVT. Unlike posterior fracture-dislocation secondary to any other causes, patients with CSVT are usually intensive care unit bound and have low Glasgow coma scale, in a state of inability to complain, causing a delay in diagnosis and chances of delay in treatment due to the concomitant treatment of CSVT. This patient was treated in coordination with the neurologists and operated by bilateral open reduction and internal fixation using proximal humerus locking plates and greater tuberosity reconstruction. 2 years post-operatively, the patient had painless shoulders, with satisfactory and functional range of motion.
Conclusion: Bilateral shoulder screening using computed tomography scan is helpful for diagnosing bilateral shoulder posterior fracture-dislocation, which can be easily missed in patients presenting with Triple E pathologies. Early recognition and appropriate treatment are very much essential in giving best functional outcomes of such cases.
Keywords: Shoulder, posterior, fracture dislocation, bilateral.
Introduction
The most common cause of fracture-dislocation of the shoulder is convulsions. Posterior fracture-dislocation of shoulders is less common; Neer has reported it to be 0.9% among the 1500 fracture-dislocations he reviewed. Bilateral posterior fracture-dislocation of the shoulders is still rare injury. Delay in diagnosis causes significant functional loss to the affected. Its association with convulsions secondary to cavernous sinus venous thrombosis (CSVT) is very unusual and treating both the conditions needs expertise. Treatment of CSVT needs anticoagulants, making it a challenge in planning the timing of surgery.
Case Report
A 29-year-old gentleman, bank employee by occupation, was brought to emergency department in a stuporous condition. According to his parents, he had headache and blurring of vision which got relieved after rest. Later, he had two episodes of generalized convulsions. There was a history of upper respiratory tract infection, fever, and headache for 5 days before the seizures. The patient was drowsy at the time of admission. Computed tomography (CT) brain revealed right sigmoid sinus and right distal transverse sinus venous thrombosis with hemorrhagic venous infarct in the posterior temporo-occipital lobe. During primary assessment, the patient had ecchymosis around right shoulder, for which right shoulder plain anteroposterior (AP) X-ray was done. It revealed right shoulder posterior fracture dislocation. Left-sided X-ray was not done as primary assessment did not reveal significant findings. Once the patient regained full consciousness, he complained of pain in both shoulders. Left side X-ray was also done, which showed left shoulder posterior fracture-dislocation too. CT scan of both the shoulders was done. These studies revealed bilateral shoulder posterior fracture dislocation, bilaterally Neer’s three-part fracture (Fig. 1 and 2).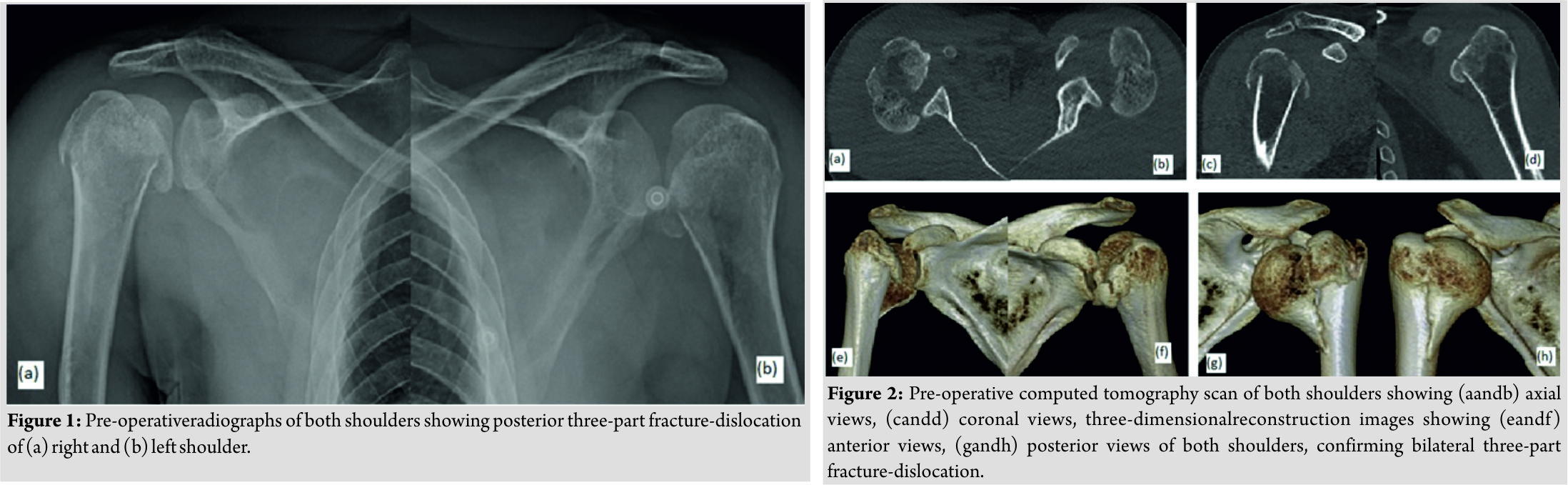
Discussion
Bilateral posterior fracture dislocation of shoulder was first described by Mynter in 1902 [1].It is almost pathognomonic of “Triple E syndrome” (epilepsy or any other convulsive seizure, extreme trauma, and electric shock) [1]. The mechanism of posterior dislocation of shoulder was described by Shaw in 1971 [2].The typical position of the shoulder during a seizure activity is adduction, flexion, and internal rotation. Massive contractions of the shoulder girdle muscles force the humeral head superiorly and posteriorly against the acromion and medially against glenoid fossa. The major muscles contributing to dislocation are infraspinatus and teres minor, along with contributions from deltoid, latissimus dorsi, and teres major. At the end of seizure activity, the humeral head is lodged behind glenoid rim, often with a reversed Hill-Sachs lesion. Further, convulsive forces may result in complex proximal humeral fracture [3]. Typical presentation of a posterior dislocation is arm in internal rotation and adducted position. Coracoid process is prominent anteriorly, deltoid appears flattened laterally and humeral head bulging out posteriorly [4]. A simple posterior dislocation of shoulder would present with impossible external rotation, but in a fracture dislocation, passive external rotation may be possible, due to motion at the fracture site; however, eliciting this may be very painful. Clinical examination may be obscure in drowsy patients, making diagnosis difficult. Attention should be given to nerve injuries once the patient regains consciousness. Diagnosis is often delayed. It can be difficult to detect posterior fracture-dislocation by plain AP X-rays. When AP X-rays do not show obvious lesion, specific views will be needed. However, in settings of fracture-dislocation obtaining specific X-ray views may be difficult and painful to patient. Specific views include an axial view, scapular Y view, and transthoracic view. Axial view is easy to interpret, whereas obtaining other special views are difficult due to lack of mobility and severe pain. The best investigation is CT scan of the shoulders, which is rapidly and easily performed and gives complete, accurate picture. It does not cause discomfort and also helps in planning treatment [5]. Treatment must be planned adaptive to the type of fracture and interval between trauma and the surgery. Factors such as age, occupation, and desired levels of activity have to be considered. Respect to the anatomy and restoration of a stable joint are essential to expect good results. For posterior dislocation with minimally displaced fractures, closed reduction can be done. K-wires can be added if necessary. Closed reduction can be achieved by pressure with both thumbs in infraspinatus fossa, with traction and adduction by assistant [5]. Closed reduction may not be successful in acute settings. In such cases, a small posterior arthrotomy can be performed to reduce the shoulder by inserting one finger. Interposition of biceps tendon into the joint space or fracture fragments may prevent reduction even with posterior arthrotomy, which warrants open reduction [5]. Closed reduction is almost impossible 3weeks after fracture-dislocation and surgery is indicated in such cases [1]. For displaced fractures, if an attempt of closed reduction fails, open reduction and internal fixation are indicated. After openly reducing, if the joint is stable, internal fixation can be achieved. Unstable joints after reduction may have reversed Hills-Sachs lesion, which needs to be addressed. If open reduction is not achieved or is unstable due to loss of more than 50% of humeral head, prosthetic replacement is recommended. For older patients (>65 years) with 3 or 4 part fracture, or younger patients with highly comminuted fractures where chances of AVN of humeral head is very high, or >50% of the humeral head loss is present, hemiarthroplasty is the best option. If there is glenoid damage in addition to the involvement of humeral head, total shoulder arthroplasty may be considered [6]. Delay in diagnosis for longer periods leads to extensive tissue scarring and anatomical distortion. After ruling out the osteonecrosis of the head of humerus, malunion correction by humeral osteotomy, McLaughlin’s procedure, and reconstruction of humeral head defect using autogenous or allogenous bone graft to maintain reduction can be the options [7]. With the above available literature, we proceeded with bilateral shoulder open reduction and internal fixation with proximal humerus locking plates. We used a deltopectoral approach on the right side and a deltoid-splittingapproach on the left side. Chances of osteonecrosis of the humeral head have to be seen for in the follow-up, even though the patient is pain free. If osteonecrosis sets in, it is well tolerated if anatomic tuberosity fixation is achieved. Bilateral posterior fracture-dislocation of shoulders can pose devastating limitation of function to the patient. Early diagnosis and early management with restoration of proper anatomy maximize the functional outcome.
Conclusion
Posterior fracture-dislocation is a diagnostic challenge and can be missed at initial presentation because of its rarity. Bilateral shoulder studies must be done in any suspicious case among Triple E pathologies (epilepsy, electric shock, and extreme trauma), even though the patient has unilateral findings. In cases associated with CSVT, planning of timing of surgery along with neurologists is essential. Restoration of bilateral shoulder anatomy is essential for achieving good functional results.
Clinical Message
An eye of suspicion is always needed for unilateral shoulder pathology in Triple E pathologies and such patients have to be screened thoroughly using CT scans bilaterally, to avoid missing of a bad unsuspectable injury.
References
1. Claro R, Sousa R, Massada M, Ramos J, Lourenço JM. Bilateral posterior fracture-dislocation of the shoulder: Report of two cases. Int J Shoulder Surg 2009;3:41-5.
2. Shaw JL. Bilateral posterior fracture-dislocation of the shoulder and other trauma caused by convulsive seizures. J Bone Joint Surg Am. 1971;53:1437–40.
3. DinKM,MeggittBF. Bilateralfour-part fractures withposteriordislocation of the shoulder. A case report. J Bone Joint Surg Br 1983;65:176-8.
4. Cicak N. Posterior dislocation of the shoulder. J Bone Joint SurgBr2004;86-B:324-32.
5. Bell HM. Posteriorfracture-dislocationof theshoulder-amethodofclosedreduction; A case report. JBoneJoint Surg Am 1965;47:1521-4.
6. MartensC,Hessels G. Bilateral posterior four-part fracture-dislocation of the shoulder. ActaOrthopBelg1995;61:249-54.
7. Gerber C,Lambert SM. Allograft reconstruction of segmental defects of the humeral head for the treatment of chronic locked posterior dislocation of the shoulder. J Bone Joint Surg Am 1996;78:376-82.
 |
 |
| Dr. Srinivas Kasha | Dr. Gopinath Bandari |
| How to Cite This Article: Kasha S, Bandari G. Bilateral Posterior Fracture-Dislocation of Shoulder Following Seizures Secondary to Cavernous Sinus Venous Thrombosis – A Rare Association. Journal of Orthopaedic Case Reports 2018 Jul-Aug; 8(4): 49-52. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com