[box type=”bio”] Learning Point for the Article: [/box]
This article highlights the importance of having a low threshold for infection for patients who have a chronic immuosuppressive state. Appropriate work up and investigations are required to rule in, or out, the possibility of infection, and ultimately therefore best manage the patient.
Case Report | Volume 8 | Issue 4 | JOCR July – August 2018 | Page 89-92| Shafiq A Shahban, Ahmed I Saad, Tarek Elgamal. DOI: 10.13107/jocr.2250-0685.1176
Authors: Shafiq A Shahban[1], Ahmed I Saad[1], Tarek Elgamal[1]
[1]Department of Trauma and Orthopaedics, Heart of England NHS Trust, UK.
Address of Correspondence:
Dr. Shafiq Shahban,
11 Field Close, Littlethorpe, Leicester, LE19 2JY, UK.
Email: shafiqshahban@hotmail.com
Abstract
Introduction: Hyper-IgE syndrome (HIES) is a relatively rare condition which, from childhood, renders patients susceptible to infection. Typically patients with HIES can develop various orthopaedic manifestations of this disease, namely scoliosis, pathological fractures, osteoporosis, and potentially septic arthritis.
Case Report: We present the case of WJ, a 44-year old patient with known HIES(since the age of 11) and a 7-week history of left hip pain. We discuss the clinical presentation and the curveballs which came our way when investigating this patient and how we overcame them.We also demonstrate a very interesting pelvic radiograph from this patient which shows multiple sites of calcified apophyses. Something which is first unexpected in such patients and second something not previously reported in the literature.
Conclusion: Several issues and conundrums can present themselves when dealing with patients known to have HIES. We demonstrate how we managed such a patient and maintained a high level of suspicion in such patient.
Keywords: Hyper-IgE syndrome, hip pain, bone mineral density, calcified apophyses, immuno suppression, septic arthritis.
Introduction
The hyper-IgE syndromes (HIES; originally named Job’s syndrome) are a collection of primary immunodeficiency syndromes resulting in elevated serum IgE levels and typified by recurrent staphylococcal skin abscesses, eczema, and pulmonary infections. This rare group of diseases often makes itself known during childhood and affects males and females equally[1]. The cause of HIES has been linked with hypomorphic mutations in the signal transducer and the activator of transcription 3 (STAT3) and tyrosine kinase 2 gene. Many studies have shown that the autosomal dominant (AD) form of HIES is also associated with musculoskeletalab normalities, such as scoliosis, pathological fractures, osteoporosis, and hypermobility[2, 3, 4]. Within this report, we present a case of a 44-year-old gentleman with known HIES presenting with left hip pain, and who was investigated for septic arthritis. We highlight the importance of having a low threshold for the suspicion of infection in such patients. We also demonstrate the pelvis X-ray for this patient and its findings.
Case Report
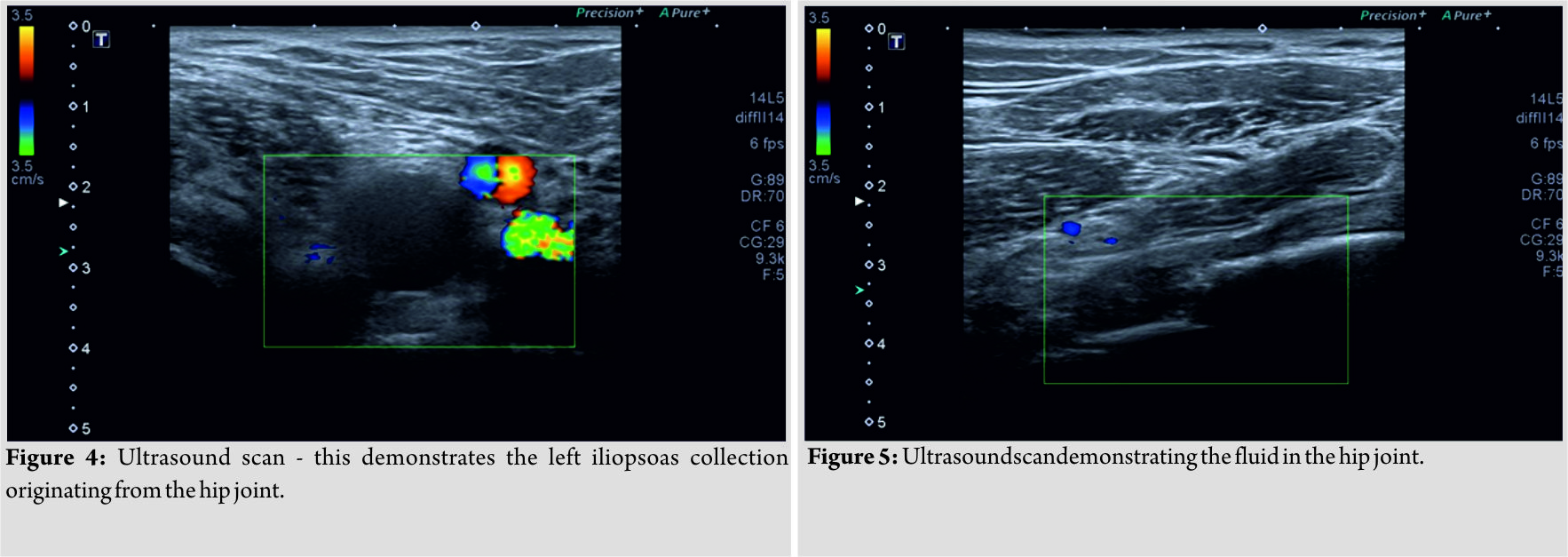
WJ, a 44-year-old gentleman, with a background of HIES and recurrent chest infections, was initially seen by his consultant immunologist in the outpatient clinic and from there admitted directly to the acute trauma and orthopaedic ward. He gave a 7-week history of worsening left hip pain, with no history of trauma, and no pre-existing history of joint arthritis (given his known HIES). A week before this outpatient attendance, WJ had organized a private magnetic resonance imaging (MRI) pelvis, which demonstrated a fluid collection within the left hip joint (Fig. 1 and 2). 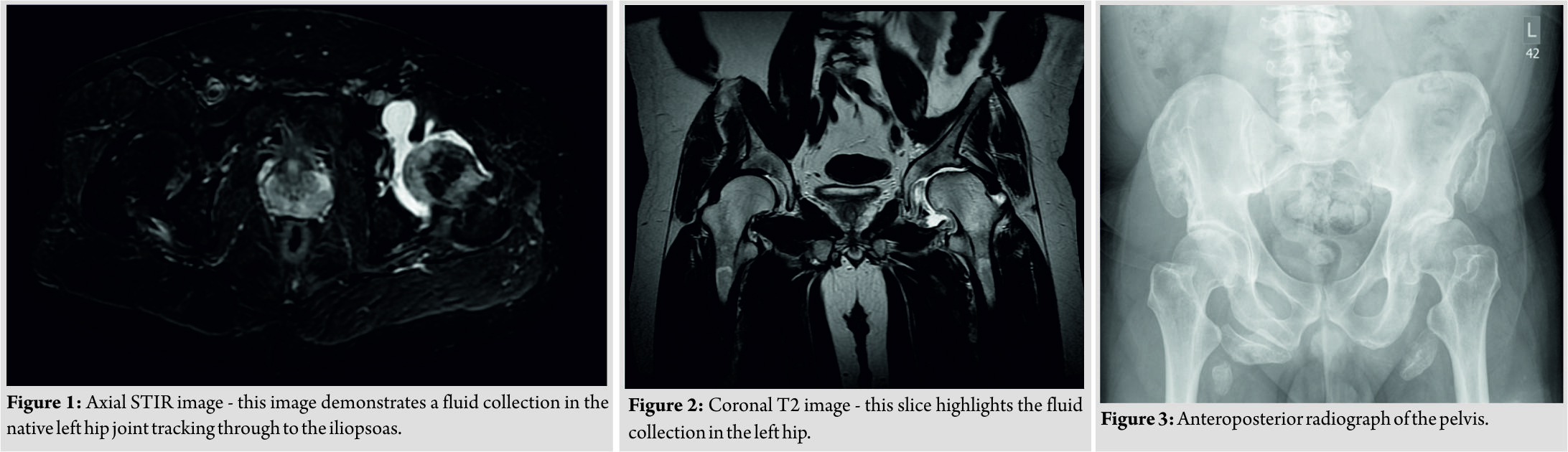
Discussion
HIES is a rare primary immunodeficiency characterized by recurrent eczema, skin abscesses, lung infections, eosinophilia, and high serum levels of IgE. Two forms of HIES have been described, including an (AD or type 1) and an (autosomal recessive or type 2) form. Involvement of both the connective and skeletal tissues is an important feature of AD-HIES with STAT3 mutations. Patients frequently sustain fractures from seemingly insignificant trauma, and bone density is likely to be reduced [5]. Studies have shown monocytes from patients with AD-HIES resorb bone at an increased rate, similar to that of postmenopausal women. Increased osteoclastic (OC) activity and increased bone resorption predispose HIES patients to osteoporosis and a subsequent high incidence of fractures [6].Moreover, although genetic studies had not been performed in this patient, studies have shown that common findings among HIES patients are recurrent fractures (in 57% of patients), joint hypermobility (in 68% of patients), scoliosis (in 76% of16-year-old patients and older), and reduced bone mineral density (BMD) in 54% of adults[7, 8]. Studies have shown that the hematopoietic cell-specific disruption of the STAT3 gene induces hyperproliferation of cells of the myeloid lineage. OC, the bone-resorbing cells, are from this family of precursors and are thus generated in high numbers. The same study demonstrated the STAT3 mutation in mice which all went on to exhibit increased numbers of OC, reduced bone volume and BMD[9]. Patients with a diagnosis of HIES are inherently immuno compromised and should be investigated and treated as such. Normal inflammatory/infective markers and/or physiological parameters should not be taken at face value and may always require further (sometimes invasive) investigation. This case highlights these points. In this case, as with other similar cases, a difficult decision had to be made with regard to the US-guided needle aspiration. On the one hand, it is important for us to correctly rule in (or out) a diagnosis of infection, while also trying to isolate the organism, however in doing this, we risk the possibility of introducing infection. On balance, given the clinical examination and MRI findings, we felt it was the correct decision in choosing to proceed with this procedure. What was also of interest in this case was the plain radiograph of this patient’s pelvis. Classically in patients with a history of HIES, from an orthopaedic perspective, osteoporosis, and fragility fractures are the radiographic features frequently seen. However, in this case, we see a left flattened and broad femoral head with a dysplastic acetabulum, with several areas of calcified apophyses. The MRI and X-ray reports, too comment on the well-corticated ossified bodies over the right and left iliac crests, iliac wings, anterior superior iliac spines, ischial tuberosities, and lesser trochanters – thus paradoxically demonstrating increased osteoblastic activity, and not that of OC. Of course, the reason for this patient hip discomfort may well be due to these findings, however, with a background HIES, and MRI findings demonstrating a fluid collection in the left hip, there was not enough evidence to rule out a diagnosis of hip septic arthritis, before an US-guided aspiration.
Conclusion
The success in the management of this patient was two-fold. First, being able to appreciate and take into account the immuno suppressed state that HIES causes, and second, appropriate and timely clinical examination and investigation to rule out infection. Patients with a diagnosis of HIES always require a high index of suspicion for the possibility of infection. On the same note, despite the increase in OC numbers and activity, skeletal imaging may still take you by surprise.
Clinical Message
Septic arthritis is an orthopaedic emergency, and early diagnosis has been shown to influence the outcome. Whether, it be a native or prosthetic joint, the appropriate investigations need to be conducted to try to rule in (or out such a diagnosis). Of course, invasive investigations, such as an US-guided aspiration, especially in immuno compromised patients, pose the risk of introducing infection, at the risk of trying to diagnose it. Finally, arthralgia in HIES patients, although may represent infection, can be a sign of other chronic orthopaedic problems, which one may not be anticipating.
References
1. Yong PF, Freeman AF, Engelhardt KR, Holland S, Puck JM, Grimbacher B, et al. An update on the hyper-IgE syndromes. Arthritis Res Ther 2012;14:228.
2. Minegishi Y, Karasuyama H. Defects in Jak-STAT-mediated cytokine signals cause hyper-IgE syndrome: Lessons from a primary immunodeficiency. Int Immunol 2009;21:105-12.
3. Renner ED, Rylaarsdam S, Anover-Sombke S, Rack AL, Reichenbach J, Carey JC, et al. Novel signal transducer and activator of transcription 3 (STAT3) mutations, reduced T(H)17 cell numbers, and variably defective STAT3 phosphorylation in hyper-IgE syndrome. J Allergy Clin Immunol 2008;122:181-7.
4. Holland SM, DeLeo FR, Elloumi HZ, Hsu AP, Uzel G, Brodsky N, et al. STAT3 mutations in the hyper-IgE syndrome. N Engl J Med 2007;357:1608-19.
5. Immune Deficiency Foundation – Patient & Family Handbook or Primary Immunodeficiency Diseases. 5th ed. Immune Deficiency Foundation; 2013. Available from: https://www.primaryimmune.org/sites/default/files/publications/IDF-Patient-Family-Handbook-5th-Edition-2015-Reprint.pdf.(Accessed 5thApril, 2018)
6. Cohen-Solal M, Prieur AM, Prin L, Denne MA, Launay JM, Graulet AM, et al. Cytokine-mediated bone resorption in patients with the hyperimmunoglobulin E syndrome. Clin Immunol Immunopathol 1995;76:75-81.
7. Grimbacher B, Holland SM, Gallin JI, Greenberg F, Hill SC, Malech HL, et al. Hyper-IgE syndrome with recurrent infections – An autosomal dominant multisystem disorder. N Engl J Med 1999;340:692-702.
8. Li J. JAK-STAT and bone metabolism. JAKSTAT 2013;2:e23930.
9. Zhang Z, Welte T, Troiano N, Maher SE, Fu XY, Bothwell AL, et al. Osteoporosis with increased osteoclastogenesis in hematopoietic cell-specific STAT3-deficient mice. Biochem Biophys Res Commun 2005;328:800-7.
 |
 |
 |
| Dr. Shafiq A Shahban | Dr. Ahmed I Saad | Dr. Ahmed I Saad |
| How to Cite This Article: Shahban S A, Saad A I, Elgamal T. An Unusual Presentation of Hip Pain in a Patient with Known Hyper-IgE Syndrome and Multiple Calcified Pelvic Apophyses. Journal of Orthopaedic Case Reports 2018 Jul-Aug; 8(4): 89-92. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com